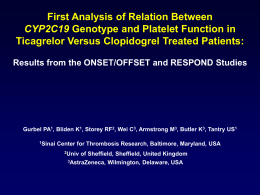
Dúvidas [email protected] Arquivo Farmacogenômica Site www.gilbertodenucci.com Aulas - Unicastelo – Fernandópolis – 2014 Pacientes com o mesmo diagnóstico Resposta preditiva boa para o medicamento Resposta preditiva ruim ou ausente Use outro medicamento Risco de toxicidade alto Diminuir a dose ou usar outro medicamento Tratamentos estabelecidos com alta eficácia e % dos pacientes beneficiados e não beneficiados com o tratamento Ensaio Droga Eventos (%) Placebo Tratad Benefício/100 Ausência de Benefício/100 Hope Ramipril 17.8 14 3.8 96.2 APTC Aspirina 14 10 4 96 FTT Trombolíticos 11.5 9.6 1.9 98.1 4S Simvastatina 28 19 9 91 EPIC Abciximab 12.8 8.3 4.5 95.5 CURE Clopidogrel 11.5 9.3 2.2 97.8 Farmacogenética Alvos do medicamento Transportadores Farmacodinâmica Enzimas metabolisadoras Farmacocinética Variabilidade na eficácia ou toxicidade Farmagenômica Distribuição Absorção Excreção Farmacogenômica Afinidade do receptor pela droga Droga atuando em produtos gênicos Curr Probl Cardiol, May 2003 The concept of pharmacogenetics. Pharmacogenomics: Challenges and Opportunities - © 2006 American College of Physicians - Ann Intern Med. 2006;145:749-757. Diastolic blood pressure response to metoprolol in hypertensive patients is predicted by ADRB1 diplotype. The Pharmacogenetics Research Network: From SNP Discovery to Clinical Drug Response - VOLUME 81 NUMBER 3 - MARCH 2007 Alelos da apo e • apo e2 • apo e3 • apo e4 Kaplan-Meier em pctes com e sem o alelo apoe4 ~Proporção Vivo 1.00 Sem e4 N=312 0.95 0.90 e4-Portadores N=166 0.85 0.80 0 500 1000 1500 2000 2500 Dias após Randomização Tratamento com Placebo Curr Probl Cardiol, May 2003 Tratamento com simvastatina reduz mortalidade em • 13% em pacientes não apo e4 • 50% em pacientes apo e4 Kaplan-Meier em pctes com e sem o alelo apoe4 Proporção Vivo 1.00 Sem e4 N=301 e4-Portadores N=187 0.95 0.90 0.85 0.80 0 500 1000 1500 2000 2500 Dias após randomização Tratamento com Simvastatina Curr Probl Cardiol, May 2003 Tiopurina Metiltransferase • • • • • • Polimorfismo TPMT Metila mercaptopurina – reduz F Leucemia linfocítica aguda 10% intermediária – maior toxicidade 0.3% não tem TMPT – fatal Genotipagem essencial UDP-glucoronosiltransferase 1A1 • • • • Irinotecan – câncer de cólon, pulmão Forma ativa inativada por glucoronidação Aumento de 4x a toxicidade Genotipagem alelo UGT1a1*28 Gene da colinesterase plasmática • • • • • Apnéia prolongada após succinilcolina 1 em 187 em Valencia 1 em 3460 europeus 1 em 25 x 106 asiáticos Complicação facilmente tratada, não há necessidade de genotipagem Leucemia mielóide crônica • • • • • Translocação no cromossoma Filadelfia Alterou localização dos genes bcr e abl bcr-abl tirosina quinase fica ativa Imatinib bloqueia especificamente Imatinib 88% resposta positiva em pctes Câncer de mama • Herceptin – ab citotóxico contra Her-2/neu. • Her-2/neu aumentada em 25% pctes • Herceptina funciona somente nestes pacientes Substratos para citocromo P4502D6 • b-bloqueadores – alprenolol, carvedilol, propranolol • Anti-arrítmicos – flecainida, mexiletina, propafenona • Neurolépticos – haloperidol, clozapina, olanzapina, risperidona • Antidepresssivos – amitriptilina, clomipramina, paroxetina • Antieméticos – ondansetrona, tropisetrona • Outros – anfetamina, codeína, debrisoquina, dextrometorfano Inibidores do citocromo P4502D6 • Neurolépticos – clomipramina, levopromazina, haloperidol • Antidepressivos – fluoxetina, paroxetina, sertralina • Antieméticos - metoclopramida • Anti-histamínicos – clorfeniramina, cimetidina, clemastina, difenilhidramina • Outros – ritonavir, quinidina, amiodarona Genótipo do citocromo P4502D6 • Metabolizadores ultrarápidos • Metabolizadores rápidos • Metabolizadores lentos Genótipo do citocromo P4502D6 • Metabolizadores ultrarápidos – muito baixa em orientais (<<1%), baixa em europeus do norte (<1%), 7% em espanhóis, 29% em etíopes • Metabolizadores rápidos • Metabolizadores lentos – muito baixa em orientais Tratamento de náusea e vômito in quimioterapia - Tropisetron • 42 pacientes, 30% tiveram náusea e vômito • CitP4502D6 – maior frequência dos demais pacientes • Genotipagem recomendável – evitaria emese severa em 1/50 pacientes. A superfamília do citocromo P450 Isoenzima Substrato típico Comentários CYP1A CYP2A Teofilina Testosterona Induzida por tabagismo Induzida por tabagismo CYP2B CYP2C Numerosos Numerosos Induzido por fenobarbital Apresenta polimorfismo genético CYP2D Debrisoquina Apresenta polimorfismo genético CYP2E CYP3A Induzida por álcool Nitrosaminas Nifedipina/ciclosporina Induzida por carbamazepina CYP4 Ácidos graxos Induzida por clofibrato Diferenças Farmacogenéticas das Enzimas que metabolizam medicamentos Enzima Pseudocolinesterase plasmática Desidrogenase alcoólica CYP2C19 CYP2D6 CYP2C? Acetil-N-transferase Metiltransferase a Para caucasianos Incidência de deficiência ou metabolizadores lentosa 1 in 3000 Substratos típicos Suxametônio (succinilcolina) 5-10% (approx. 90% em Asiáticos) Etanol 5% (approx. 20% em Asiáticos) S-Mefenitoína, omeprazole 5 - 10% Debrisoquina, espartina, metoprolol, dextrometorfan Fenitoína Muito raro Isoniazida, hidralazina, Approx. 60% (approx. 5% em procainamida japoneses) 6-Mercaptopurina 0.5 % Cytochrome P-450 Ribbon model of CYP2C9 isozyme CYP3A 50% CYPD6 25% 5% 5% CYP2C9 15% Other CYP1A2 Netter’s Iluustrated Pharmacology – Chapter 1 – Fig. 1.30 BIOSSÍNTESE DO TXA2 Estímulo Fosfolipídeos Fosfolipase A2 Ácido araquidônico PGG2, PGH2 TX sintase TXA2 Major pathways leading to the formation of thienopyridine active metabolites P2Y12 inhibitors: differences in properties and mechanisms of action and potential consequences for clinical use. European Heart Journal (2009) 30, 1964–1977 Fármacos antiplaquetários Derivados da tienopiridina Ticlopidina Ticlopidina • inibição irreversível do receptor de P2Y12 de ADP • pró-droga – requer conversão a tiol por enzima do citocromo P450 hepático • rapidamente absorvida • T1/2 curta com longa duração de ação • início de ação lento (3-7 dias) Clopidogrel Major pathways leading to the formation of thienopyridine active metabolites Review: Acetyl-coenzyme A carboxylase: crucial metabolic enzyme and attractive target for drug discovery. CMLS, Cell. Mol. Life Sci. 62 (2005) 1784–1803. Fármacos antiplaquetários Clopidogrel - estreitamente relacionado com a ticlopidina - vantagem em relação à ticlopidina – maior tolerabilidade gastro-intestinal e menor risco de neutropenia e trombocitopenia - reduz taxa de AVC, IM - reduz morte de pacientes com AVC ou IM recentes - uso indicado após angioplastia (conjuntamente com o ácido acetilsalicílico) Variability in platelet aggregation between individuals in response to clopidogrel Review: Platelet Function Testing and Implications for Clinical Practice. J Cardiovasc Pharmacol Ther 2009; 14; 157. Impact of clopidogrel loading dose on level of response measured by inhibition of adenosine diphosphate (ADP)-induced platelet aggregation Review: Platelet Function Testing and Implications for Clinical Practice. J Cardiovasc Pharmacol Ther 2009; 14; 157. The ACAPULCO Study. Response to clopidogrel and prasugrel using 3 different definitions of response Review: Platelet Function Testing and Implications for Clinical Practice. J Cardiovasc Pharmacol Ther 2009; 14; 157. Significantly attenuated platelet inhibition by clopidogrel in carriers of the CYP2C19² allele as compared with the wild-type homozygote CYP2C19¹ Review: Platelet Function Testing and Implications for Clinical Practice. J Cardiovasc Pharmacol Ther 2009; 14; 157. INIBIDORES DE CITOCROMO P450 1A2 2B6 2C8 2C19 2C9 2D6 2E1 3A4,5,7 Cimetidina Fluoroquinolonas Fluvoxamina Ticlopidina Ticlopidina Gemfibrozila Montelukast Fluoxetina Fluvoxamina Amiodarona Fluconazol Isoniazida Amiodarona Disulfiram Inbidores de Protease: Indinavir Nelfinavir Ritonavir Cetoconazol Lansoprazol Omeprazol Ticlopidina Bupropriona Clorfeniramina Cimetidina Clomipramina Fluoxetina Haloperidol Metadona Paroxetina Quinidina Ritonavir Amiodarone Cimetidina Claritromicina Diltiazem Eritromicina Fluvoxamina Itraconazol Cetoconazol Verapamil *Risk of Rehospitalization for Patients Using Clopidogrel With a Proton Pump Inhibitor* Karen M. Stockl, PharmD; Lisa Le, MS; Armen Zakharyan, PhD; Ann S. M. Harada, PhD, MPH; Brian K. Solow, MD; Joseph E. Addiego, MD; Scott Ramsey, MD, PhD /Arch Intern Med./ 2010;170(8):704-710. •Background * Recent pharmacodynamic and retrospective clinical analyses have suggested that proton pump inhibitors (PPIs) may modify the antiplatelet effects of clopidogrel bisulfate. * Methods * We conducted a retrospective cohort study of persons enrolled in a multistate health insurance plan with commercial and Medicare clients to evaluate adverse clinical outcomes in patients using clopidogrel plus a PPI compared with clopidogrel alone. Patients who were discharged from the hospital after myocardial infarction (MI) or coronary stent placement and treated with clopidogrel plus a PPI (n = 1033) were matched 1:1 (using propensity scoring) with patients with similar cardiovascular risk factors treated with clopidogrel alone. Rehospitalizations for MI or coronary stent placement were evaluated for up to 360 days. A subanalysis was conducted to study the impact of pantoprazole sodium, the most used PPI. * Results * Patients who received clopidogrel plus a PPI had a 93% higher risk of rehospitalization for MI (adjusted hazard ratio, 1.93; 95% confidence interval, 1.05-3.54; /P/ = .03) and a 64% higher risk of rehospitalization for MI or coronary stent placement (1.64; 1.16-2.32; /P/ = .005) than did patients receiving clopidogrel alone. Increased risk of rehospitalization for MI or coronary stent placement was also observed for the subgroup of patients receiving clopidogrel plus pantoprazole (adjusted hazard ratio, 1.91; 95% confidence interval, 1.19-3.06; /P/ = .008). * Conclusions * Patients who received clopidogrel plus a PPI had a significantly higher risk of rehospitalization for MI or coronary stent placement than did patients receiving clopidogrel alone. Prospective clinical trials and laboratory analyses of biochemical interactions are warranted to further evaluate the potential impact of PPIs on the efficacy of clopidogrel. Limitations and challenges associated with vitamin K antagonists. INR international normalized ratio Novel anticoagulants and the future of anticoagulation. Thrombosis Research (2009) 123 Suppl. 4, S50–S55. After oral absorption, warfarin is transported to the liver where CYP1A1, CYP1A2, and CYP3A4 metabolize the R-enantiomer and CYP2C9 metabolizes the more potent S-enantiomer. Pharmacogenetics of warfarin: regulatory, scientific, and clinical Issues - J Thromb Thrombolysis (2008) 25:45–51 – fig 01 Vitamin K is responsible for the carboxylation or activation of clotting factors II, VII, IX, and X in the liver. Vitamin K reductase enzymes keep the vitamin in an active (reduced) state Each box contains the median weekly warfarin dose for the different 1173C/T genotype, and the bars represent the interquartile range. There was only one African American with the TT genotype. Warfarin Response and Vitamin K Epoxide Reductase Complex 1 in African Americans and Caucasians VOLUME 81 NUMBER 5 | MAY 2007 | www.nature.com/cpt Maintenance dose of warfarin by VKORC1 1173C/T polymorphism, stratified by race. Cytochrome P450 2C9 SNPs that are known to affect warfarin metabolism Pharmacogenetics of warfarin: regulatory, scientific, and clinical Issues - J Thromb Thrombolysis (2008) 25:45–51 – tab. 01 Cytochrome and Warfarin Antithrombotic management of patients with prosthetic heart valves: current evidence and future trends. Lancet 2009; 374: 565–76. Effect of VKORC1 haplotype on warfarin dose stratified by VKORC1 haplotype and CYP2C9 status: either wild type (WT) or CYP2C9*2 and/or CYP2C9*3 mutants (MUT) Primary cohort: UW (N = 185); Replication cohort: Wash U (N = 368) Pharmacogenetics of warfarin: regulatory, scientific, and clinical Issues - J Thromb Thrombolysis (2008) 25:45–51 – fig 02 Challenges in Pharmacogenomics Pharmacogenomics: Challenges and Opportunities - © 2006 American College of Physicians - Ann Intern Med. 2006;145:749-757. Examples of Associations between Drug Response and Genetic Variants* Pharmacogenomics: Challenges and Opportunities - © 2006 American College of Physicians - Ann Intern Med. 2006;145:749-757. Definitions of commonly used terms Pharmacogenomics: Bridging the gap between science and practice - J Am Pharm Assoc. 2010;50:e1–e17 Systematic approach to understanding polymorphisms Pharmacogenomics: Bridging the gap between science and practice - J Am Pharm Assoc. 2010;50:e1–e17 HLA: a pharmacogenomics success story - Pharmacogenomics (2010) 11(3), 277–281 Pharmacogenomic risk factors for adverse drug reactions MEDICAMENTOS QUE SÃO METABOLIZADOS POR ISOFORMAS DO CITOCROMO P450 1A2 2B6 Clozapina Bupropiona Ciclobenzaprina Ciclofosfamida Efavirez Metadona Imipramina Naproxeno Teofilina 2C8 2C19 2C9 Inibidores de Bomba de Próton: Omeprazole Lansoprazole Pantoprazole Rabeprazole AINEs: Diclofenaco Ibuprofeno Piroxicam Ciclofosfamida Progesterona Betabloqueadores: S-metoprolol Timolol Antidepressivos: Hipoglicemiantes orais: Tolbutamida Glipizida Anti-epilépticos: Diazepam Fenitoína Fenobarbital Amitriptilina Clomipramina 2D6 Antagonistas de Angiotensina II: Irbesartan Losartan Amitriptilina Clomipramina Desipramina Imipramina Paroxetina 2E1 Paracetamol Etanol 3A4,5,7 Antibióticos macrolídeos: Claritromicina, eritromicina, Anti-arrítmico: Quinidina Benzodiazepínicos: alprazolam, diazepam, midazolam, triazolam Imunomoduladores: Ciclosporina, Tacrolimus Antipsicóticos: Celecoxib Fluvastatina Naproxeno Fenitoína Sulfametoxazole Tamoxifeno Tolbutamida Warfarina Haloperidol Risperidona Codeína Dextrometorfano Flecainida Ondansetrona Tamoxifeno Tramadol Venlafaxina HIV inibidores de protease: indinavir, ritonavir, saquinavir Anti-histamínicos: astemizole, clorfeniramina Bloqueadores de canais de cãlcio: amlodipina, diltiazem, felodipina, nifedipina, nisoldipina, nitrendipina, verapamil Estatinas: atorvastatina, cerivastatina, lovastatina Bisórpma Gleevec, Haloperidol Metadona, Quinina Sildenafil Tamoxifeno Vincristina
Download