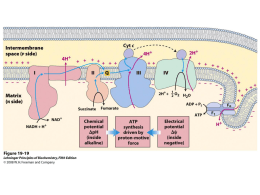
Experimental Neurology 196 (2005) 112 – 119 www.elsevier.com/locate/yexnr CoQ10 therapy attenuates amyloid h-peptide toxicity in brain mitochondria isolated from aged diabetic rats Paula I. Moreira a, Maria S. Santos a, Cristina Sena b, Elsa Nunes b, Raquel Seiça b, Catarina R. Oliveira c,* a Center for Neuroscience and Cell Biology, Department of Zoology-Faculty of Sciences and Technology, University of Coimbra, 3004-517 Coimbra, Portugal b Center for Neuroscience and Cell Biology, Institute of Physiology-Faculty of Medicine, University of Coimbra, 3004-517 Coimbra, Portugal c Center for Neuroscience and Cell Biology, Institute of Biochemistry-Faculty of Medicine, University of Coimbra, 3004-517 Coimbra, Portugal Received 26 April 2005; revised 12 July 2005; accepted 18 July 2005 Available online 29 August 2005 Abstract Using brain mitochondria isolated from 20-month-old diabetic Goto – Kakizaki rats, we evaluated the efficacy of CoQ10 treatment against mitochondrial dysfunction induced by Ah1 – 40. For that purpose, several mitochondrial parameters were evaluated: respiratory indexes (RCR and ADP/O ratio), transmembrane potential (DCm), repolarization lag phase, repolarization and ATP levels and the capacity of mitochondria to produce hydrogen peroxide. We observed that 4 AM Ah1 – 40 induced a significant decrease in the RCR and ATP content and a significant increase in hydrogen peroxide production. CoQ10 treatment attenuated the decrease in oxidative phosphorylation efficiency and avoided the increase in hydrogen peroxide production induced by the neurotoxic peptide. These results indicate that CoQ10 treatment counteracts brain mitochondrial alterations induced by Ah1 – 40 suggesting that CoQ10 therapy can help to avoid a drastic energy deficiency that characterizes diabetes and Alzheimer’s disease pathophysiology. D 2005 Elsevier Inc. All rights reserved. Keywords: Amyloid h-peptide; Brain; Coenzyme Q10; Diabetes; Mitochondria; Neuroprotection Introduction Type 2 diabetes accounts for about 90% of the existing cases of diabetes and is characterized by defects in both insulin action and secretion (Gavin et al., 1997). Many studies demonstrated that diabetes produces molecular, cellular, morphological and behavioral changes in the central nervous system (CNS) (Biessels et al., 2002). Diabetes is often associated with mitochondrial diseases characterized by defects in the mitochondrial genome (Gerbitz et al., 1995). Mitochondria play a central role in the development of type 2 diabetes by regulating energy balance and the generation of reactive oxygen species (ROS) (Wallace, 1999; Lowell and Shulman, 2005). * Corresponding author. Fax: +351 239 822776. E-mail address: [email protected] (C.R. Oliveira). 0014-4886/$ - see front matter D 2005 Elsevier Inc. All rights reserved. doi:10.1016/j.expneurol.2005.07.012 Defects in energy metabolism are a consistent feature of AD-affected brain. In Alzheimer’s disease (AD), a major imbalance between glucose and oxygen consumption has been found in the incipient stage, whereas in the advanced stage, both glucose and oxygen consumption are diminished (Hoyer, 1991). This could be a consequence of deviant insulin action or brain insulin receptor function, which can affect brain energy metabolism (Hoyer, 1991). These abnormalities in insulin metabolism may account for the pathological changes (formation of senile plaques and neurofibrillary tangles) found in Alzheimer’s disease (Frolich et al., 1998; Hoyer, 2002). Several lines of evidence suggest that amyloid deposition in the brain contributes to neuronal degeneration in AD (Selkoe, 2001) just as amyloid formation in the pancreas is believed to contribute to h-cell loss in type 2 diabetes (Höppener et al., 2000). Hoyer (1998) argues that in lateonset AD, a disturbance in the control of neuronal glucose P.I. Moreira et al. / Experimental Neurology 196 (2005) 112 – 119 metabolism consequent to impaired insulin signaling strongly resembles the pathophysiology of type 2 diabetes in nonneural tissue. Furthermore, several epidemiological studies have established that diabetes increases the risk of dementia in general (Hassing et al., 2004) and AD in particular (Leibson et al., 1997; Ott et al., 1999). The observation that oxidative stress is increased in AD and diabetes has generated the notion that antioxidants and other regulators of oxidative stress may protect against oxidative damage. Coenzyme Q is a potent antioxidant and free radical scavenger as well as membrane stabilizer (Beyer and Ernster, 1990). Besides its antioxidant properties, coenzyme Q has an important function in mitochondrial bioenergetics. It participates as a cofactor of dehydrogenases in the transport of electrons and protons as well as in ATP production (Mitchell, 1991; Crane and Navas, 1997). Several animal models are available for experimental investigation of type 2 diabetes. One of those models is the Goto –Kakizaki (GK) rat: a nonobese, spontaneously diabetic animal (Serradas et al., 1998) produced by selective breeding of Wistar rats and first characterized by Goto and Kakizaki (Goto and Kakizaki, 1981). Previous data from our laboratory have shown that diabetes-related mitochondrial dysfunction is exacerbated by aging and/or by the presence of the neurotoxic Ah peptides (Moreira et al., 2003). In this line, this study was aimed to evaluate the efficacy of coenzyme Q10 (CoQ10) treatment against the mitochondrial dysfunction induced by the neurotoxic agent Ah1 – 40. For this purpose, we used brain mitochondria isolated from 20-month-old GK rats and the following mitochondrial parameters were examined: respiratory indexes (RCR and ADP/O ratio), transmembrane potential, lag phase of repolarization, repolarization and ATP levels and the production of hydrogen peroxide. Studies in an aged animal model of type 2 diabetes may identify a key metabolic feature common to that disorder and late-onset AD. Materials and methods Materials Ah1 – 40 was obtained from Bachem AG (Bubendorf, Germany). Protease (Subtilisin, Carlsberg) type VIII, CoQ10 and soybean oil were obtained from Sigma (Portugal). Digitonin was obtained from Calbiochem. All the other chemicals were of the highest grade of purity commercially available. 113 access to water and powdered rodent chow (diet C.R.F. 20, Charles River, France). Glucose tolerance tests were used to select GK rats for study. GK rats were randomly divided into three groups: group 1: soybean oil (vehicle solution) (2 ml/kg i.p.), group 2: CoQ10 (20 mg/kg i.p.) and group 3: GK rats without treatment. Animals were injected each 48 h during 7 weeks. Experiments were conducted 24 h after the last injection. Adhering to procedures approved by the Institutional Animal Care and Use Committee, the animals were sacrificed by cervical displacement and decapitation. Biochemical analysis Blood glucose was determined immediately after animals sacrifice by a glucose oxidase reaction, using a glucometer (Glucometer-Elite, Bayer) and compatible reactive tests. Hemoglobin A1C (HbA1c) levels were determined through ionic change chromatographic assay (Abbott Imx Glicohemoglobin, Abbott Laboratories, Portugal). Levels of urinary 8-hydroxydeoxyguanosine (8-OHdG) were determined using a commercially available enzyme-linked immunosorbent assay (Bioxytech 8-OHdG-EIA Kit, Oxis Health Products, Portland, USA). Isolation of brain mitochondria Brain mitochondria were isolated from male Wistar and GK rats by the method of Rosenthal et al. (1987), with slight modifications, using 0.02% digitonin to free mitochondria from the synaptosomal fraction. In brief, a rat was decapitated, and the whole brain minus the cerebellum was rapidly removed, washed, minced and homogenized at 4-C in 10 ml of isolation medium (225 mM mannitol, 75 mM sucrose, 5 mM Hepes, 1 mM EGTA, 1 mg/ml bovine serum albumin, pH 7.4) containing 5 mg of the bacterial protease. Single brain homogenates were brought to 30 ml with the isolation medium and then centrifuged at 2000g for 3 min. The pellet, including the fluffy synaptosomal layer, was resuspended in 10 ml of the isolation medium containing 0.02% digitonin and centrifuged at 12,000g for 8 min. The brown mitochondrial pellet without the synaptosomal layer was then resuspended again in 10 ml of medium and recentrifuged at 12,000g for 10 min. The mitochondrial pellet was resuspended in 300 Al of resuspension medium (225 mM mannitol, 75 mM sucrose, 5 mM Hepes, pH 7.4). Mitochondrial protein was determined by the biuret method calibrated with bovine serum albumin (Gornall et al., 1949). Membrane potential (DWm) measurements Animals and experimental protocol Male GK and control Wistar rats with 20 months of age were housed in our animal colony (Laboratory Research Center, University Hospital, Coimbra, Portugal). They were maintained under controlled light and humidity with free The mitochondrial transmembrane potential was monitored by evaluating the transmembrane distribution of TPP+ (tetraphenylphosphonium) with a TPP+-selective electrode prepared according to Kamo et al. (1979) using a Ag/AgCl2 electrode as reference. 114 P.I. Moreira et al. / Experimental Neurology 196 (2005) 112 – 119 Reactions were carried out in a chamber with magnetic stirring in 1 ml of reaction medium (100 mM sucrose, 100 mM KCl, 2 mM KH2PO4, 5 mM Hepes, 10 AM EGTA, pH 7.4) supplemented with 3 AM TPP+. The experiments were started by adding 5 mM succinate to mitochondria in suspension at 0.8 mg protein/ml. After a steady-state distribution of TPP+ had been reached (ca. 2 min of recording), Ca2+ was added and DCm recorded. Membrane potential was estimated from the decrease of TPP+ concentration in the reaction medium as described elsewhere (Moreno and Madeira, 1991). Homogenates were incubated with 4 AM Ah1 – 40 for 5 min before succinate addition. were incubated at 37-C with 10 mM succinate in 1.5 ml of phosphate buffer, pH 7.4, containing 0.1 mM EGTA, 5 mM KH2PO4, 3 mM MgCl2, 145 mM KCl, 30 mM Hepes, 0.1 mM homovalinic acid and 6 U/ml horseradish peroxidase in the presence or absence of 4 AM Ah1 – 40. The incubation was stopped at 15 min with 0.5 ml of cold 2 M glycine buffer containing 25 mM EDTA and NaOH, pH 12. The fluorescence of supernatants was measured at 312 nm as excitation wavelength and 420 nm as emission wavelength. The rate of H2O2 production was calculated using a standard curve of H2O2. Statistical analysis Mitochondrial respiration Results are presented as mean T SEM of the indicated number of experiments. Statistical significance was determined using the one-way ANOVA test for multiple comparisons, followed by the post hoc Tukey –Kramer test. A P value < 0.05 was considered significant. Oxygen consumption of isolated mitochondria was monitored polarographically with a Clark oxygen electrode (Estabrook, 1967) connected to a suitable recorder in a 1 ml, thermostated, water-jacketed closed chamber, with magnetic stirring. The reactions were carried out at 30-C in 1 ml of the reaction medium with 0.8 mg protein. Homogenates were incubated with 4 AM Ah1 – 40 for 5 min before succinate addition. Results CoQ10 treatment decreases glycemia levels Analysis of ATP To confirm diabetes mellitus in GK rats glycemia, glycated hemoglobin, body weight and the urinary levels of 8-OHdG were determined (Table 1). The percentage of glycated hemoglobin (HbA1C), glycemia and levels of 8OHdG were significantly higher in GK rats (66.38% T 4.89, 158.75% T 10.52, 172.74% T 12.1, respectively) when compared with control animals. However, body weight was significantly lower in diabetic animals (49.54% T 2.18) when compared with control animals. CoQ10 as well as soybean oil (vehicle solution) induced a slight improvement in glycemia levels (17.45% T 1.01 and 13.05% T 2.83, respectively) when compared to GK rats without treatment. However, both CoQ10 and soybean oil did not induce any significant alteration in body weight, HbA1C and 8-OHdG levels when compared to GK rats without treatment (Table 1). At the end of the DCm experiments, each mitochondrial suspension was rapidly centrifuged at 14,000 rpm for 6 min with 0.3 M perchloric acid. The supernatants were neutralized with 10 M KOH in 5 M Tris and centrifuged at 14,000 rpm for 5 min. The resulting supernatants were assayed for ATP by separation in a reverse-phase high performance liquid chromatography. The chromatography apparatus was a Beckman-System Gold, consisting of a 126 Binary Pump Model and 166 Variable UV detector controlled by a computer. The detection wavelength was 254 nm, and the column was a Lichrospher 100 RP-18 (5 Am) from Merck. An isocratic elution with 100 mM phosphate buffer (KH2PO4) pH 6.5 and 1.0% methanol was performed with a flow rate of 1 ml/min. The required time for each analysis was 6 min. Measurement of H2O2 production CoQ10 avoids a drastic decrease in respiratory control ratio (RCR) induced by the amyloid b-peptide The rate of hydrogen peroxide (H2O2) production was measured fluorimetrically using a modification of the method described by Barja (1999). Briefly, mitochondria The RCR is defined as the ratio between the states 3 (consumption of oxygen in the presence of substrate and Table 1 Characterization of Wistar control and GK diabetic rats Wistar GK GK vehicle GK CoQ10 Glycemia (mg/dl) HbA1C (%) 114.9 T 297.3 T 258.5 T 245.4 T 5.01 8.34 7.87 7.52 28.1 16.1*** 7.6** 19.1** T T T T 0.08 0.33*** 0.06*** 0.35*** Body weight (g) 760.9 383.9 387.7 398.6 T T T T 28.0 11.4*** 3.32*** 9.03*** 8OHdG (ng/ml) 141.6 386.2 303.2 303.8 T T T T 18.8 35.9*** 49.9*** 60.3*** Data shown represent mean T SEM from 6 animals for each condition studied. ***P < 0.001; **P < 0.01, statistically significant when compared with Wistar control rats. P.I. Moreira et al. / Experimental Neurology 196 (2005) 112 – 119 ADP) and 4 (consumption of oxygen after ADP has been consumed) of respiration. At basal conditions, no significant alterations were induced by CoQ10 treatment (Fig. 1A). The presence of 4 AM Ah1 – 40 induced a significant decrease in all the conditions tested, however, less pronounced in diabetic animals treated with both CoQ10 (15.09% T 2.03) and soybean oil (17.12% T 1.01) than in GK rats without treatment (19.63% T 0.24), when compared to GK rats without treatment and in the absence of the neurotoxic peptide (Fig. 1A). ADP/O ratio, an indicator of oxidative phosphorylation efficiency, is expressed by the ratio between the amount of ADP added and the oxygen consumed during state 3 respiration. We did not observe any significant alteration in this respiratory parameter induced by CoQ10 treatment and/or the presence of 4 AM Ah1 – 40 (Fig. 1B). 115 CoQ10 treatment prevents the decrease in oxidative phosphorylation efficiency induced by amyloid b-peptide DCm is fundamental for the phenomenon of oxidative phosphorylation, the conversion of ADP to ATP via ATP synthase. Mitochondrial respiratory chain pumps H+ out of the mitochondrial matrix across the inner mitochondrial membrane. The H+ gradient establishes an electrochemical potential (Dp) resulting in a pH (DpH) and a voltage gradient (DCm) across the mitochondrial inner membrane. We observed that neither CoQ10 treatment nor Ah1 – 40 exposure induced any significant alteration in the DCm as well as in the repolarization lag phase (Table 2). In this study, repolarization lag phase is defined as the time required for mitochondria to phosphorylate the ADP added to the reaction medium. Concerning the repolarization level (capacity of mitochondria to re-establish the DCm, after ADP phosphorylation), we observed that the presence of Ah1 – 40 induced a significant decrease of this parameter in GK rats without treatment when compared with GK rats at basal conditions (9.55% T 0.97) as well as when compared with GK rats treated with CoQ10 and soybean oil (10.92% T 0.08 and 11.64% T 0.95, respectively) (Table 2). Mitochondria isolated from diabetic animals treated with soybean oil and CoQ10 did not suffer any significant alteration of this parameter when exposed to the neurotoxic peptide. At basal conditions, CoQ10 and soybean oil did not induce any significant alteration on ATP content of brain mitochondria. However, the presence of Ah1 – 40 induced a significant decrease of this parameter in mitochondria isolated from diabetic rats without treatment (10.65% T 3.7) when compared with GK rats at basal condition. However, CoQ10 treatment prevented the decrease in ATP levels induced by Ah1 – 40 (Table 2). CoQ10 treatment prevents the increase in hydrogen peroxide levels induced by amyloid b-peptide Fig. 1. Effect of CoQ10 treatment and h-amyloid exposure on mitochondrial respiratory indexes. (A) Respiratory control ratio (RCR), (B) ADP/O ratio. Freshly isolated brain mitochondria (0.6 mg) in 1 ml of the standard medium supplemented with 2 AM rotenone were energized with 5 mM succinate. Isolates were incubated with 4 AM Ah1 – 40 for 5 min, at 30-C, before mitochondria energization. #P < 0.05, statistically significant when compared to GK rats. $$P < 0.01; $P < 0.05 statistically significant when compared with GK rats treated with the vehicle solution. &&&P < 0.001; &&P < 0.01, statistically significant when compared with GK rats treated with CoQ10. Data shown represent mean T SEM from 6 animals for each condition studied. The production of H2O2 by mitochondria gives an indication of the propensy of mitochondria to originate and/or exacerbate oxidative stress. We observed that diabetic rats mitochondria exposed to Ah1 – 40 produced a significantly higher level of H2O2 when compared with brain mitochondria isolated from CoQ10 treated animals in the presence (127.15% T 2.5) or absence (83.68% T 4.4) of Ah1 – 40 indicating that CoQ treatment avoids the increase of H2O2 production (Fig. 2). Discussion Neuron viability and defense against neurodegenerative injury can be achieved by targeting mitochondrial function to reduce oxidative stress, increase mitochondrial defense mechanisms or promote energetic metabolism. In this study, we observed that GK rats submitted to CoQ10 treatment 116 P.I. Moreira et al. / Experimental Neurology 196 (2005) 112 – 119 Table 2 Effect of CoQ10 treatment and h-amyloid exposure on mitochondrial transmembrane potential (DCm), repolarization level, repolarization lag phase and ATP content of brain mitochondria isolated from diabetic rats DCm ( Wistar GK GK vehicle GK CoQ10 GK + Ah1 – 40 GK vehicle + Ah1 – 40 GK CoQ10 + Ah1 – 40 178.1 180.5 182.0 180.7 165.5 170.9 180.3 T T T T T T T mV) 3.09 3.35 2.87 2.89 3.58 3.19 3.21 Repolarization level ( 147.7 152.8 156.0 155.1 138.2 145.2 143.6 T T T T T T T 2.23 2.14 2.96 3.50 3.62#,*,$,&& 3.49 3.61 mV) Repolarization lag phase (min) 0.668 0.676 0.613 0.629 0.721 0.670 0.726 T T T T T T T 0.043 0.056 0.038 0.027 0.075 0.039 0.067 ATP content (nmol/mg) 318.0 309.8 296.1 293.2 276.8 231.5 294.2 T T T T T T T 14.72 18.85 16.81 12.08 7.40# 19.70* 12.28 Freshly isolated brain mitochondria (0.6 mg) in 1 ml of the reaction medium supplemented with 3 AM TPP+ and 2 AM rotenone were energized with 5 mM succinate. *P < 0.05 statistically significant when compared with Wistar rats. #P < 0.05 statistically significant when compared with GK rats. $P < 0.05 statistically significant when compared with GK rats treated with the vehicle solution. &&P < 0.01 statistically significant when compared with GK rats treated with CoQ10. Data shown represent mean T SEM from 6 animals for each condition studied. possess brain mitochondria more resistant to Ah1 – 40 neurotoxicity. The characterization of diabetes mellitus in GK rats was performed by determining glycemia, glycated hemoglobin (HbA1C), urinary levels of 8-OHdG and body weight. A significant increase in glycated hemoglobin, glycemia and 8-OHdG levels (DNA oxidation) was observed in GK rats when compared with control animals (Table 1). A considerable amount of evidence suggests that oxidative stress may play an important role in the pathogenesis and complications of diabetes (Baynes, 1991, 1995; Seghrouchni et al., 2002). Different mechanisms can contribute to the enhanced oxidative stress in diabetic patients, in particular in subjects with poor glycemic control and hypertriglyceridemia (Kitahara et al., 1980; Armstrong and Al-Awadi, 1991; Leinonen et al., 1997; Collins et al., 1998; Fig. 2. Effect of CoQ10 treatment and h-amyloid exposure on H2O2 production. Freshly isolated brain mitochondria were incubated at 0.2 mg protein/ml under standard conditions as described in Materials and methods. *P < 0.05 statistically significant when compared with Wistar rats. #P < 0.05 statistically significant when compared with GK rats. $$P < 0.01 statistically significant when compared with GK rats in the presence of 4 AM Ah1 – 40. Data shown represent mean T SEM from 6 animals for each condition studied. Hinokio et al., 1999). Increased urinary excretion and higher levels of 8-OHdG in mononuclear leukocyte DNA have been found in types 1 and 2 diabetic patients (Dandona et al., 1996; Leinonen et al., 1997; Hinokio et al., 1999). Studies with the comet assay have shown increased levels of DNA breakage in peripheral blood cells of diabetic patients with poor glycemic control, but not in patients with normal glycemia (Collins et al., 1998; Anderson et al., 1998). Furthermore, we observed that GK rats present a lower body weight when compared with control animals (Table 1). The pathogenesis of diabetes in the GK rat involves an impaired insulin secretion, insulin resistance, an abnormal glucose metabolism as well as an impaired ontogenetic development of pancreatic islet cells. However, in contrast to many other rodent models of type 2 diabetes, GK rats do not become obese and do not develop hyperlipidemia (for review see Janssen et al., 2004). Accumulating evidence suggests that mitochondrial dysfunction is intimately associated with diabetes and AD pathophysiology. Studies from our laboratory showed that Ah inhibits the respiratory chain complexes and reduces ATP levels in PC12 cells (Pereira et al., 1998, 1999). We also reported that Ah exacerbates the Ca2+-induced opening of the mitochondrial permeability transition in isolated brain mitochondria, without inducing the permeability per se (Moreira et al., 2001, 2002). In addition, we have demonstrated that a functional mitochondria is required for Ah-induced neurotoxicity, as investigated using U+ and U0 mitochondrial DNA depleted cells (Cardoso et al., 2001). Interestingly, several antioxidants (vitamin E, idebenone and reduced glutathione), melatonin and nicotine showed protective effects by maintaining the mitochondrial membrane potential, improving the activity of the respiratory complexes and the cellular energetic levels (Cardoso et al., 2001). Recently, Lustbader et al. (2004) reported that Ah interacts with Ah-binding dehydrogenase (ABAD) in mitochondria obtained from brains of AD patients and transgenic mice, which suggests that ABAD is a direct molecular link from Ah to mitochondrial toxicity. Furthermore, we found that type 2 diabetes-related mitochondrial dysfunction is exacerbated by aging and/or by the P.I. Moreira et al. / Experimental Neurology 196 (2005) 112 – 119 presence of the neurotoxic Ah peptides (Moreira et al., 2003). Recently, Lowell and Shulman (2005) discussed the emerging evidence supporting the potentially unifying hypothesis that the prominent features of type 2 diabetes are caused by mitochondrial dysfunction. In accordance with our previous results, we observed that the presence of 4 AM Ah1 – 40 induces a significant decrease in the RCR (Fig. 1A) and ATP content (Table 2) and a significant increase in H2O2 production (Fig. 2). Recently, Takuma et al. (2005) reported that neurons cultured from transgenic mice with targeted overexpression of a mutant form of amyloid precursor protein and ABAD display spontaneous S generation of H2O2 and superoxide anion (O2 ), and decreased ATP, as well as subsequent release of cytochrome c from mitochondria and induction of caspase-3like activity followed by DNA fragmentation and loss of cell viability. Coenzyme Q (CoQ) alterations have been suggested to be involved in diabetes (Jameson, 1991; McCarthy, 1999) and in neurodegenerative diseases such as Huntington’s disease (HD) (Koroshetz et al., 1997), Parkinson’s disease (PD) (Ebadi et al., 2001), Alzheimer’s disease (AD) (Edlund et al., 1992) and amyotrophic lateral sclerosis (Sohmiya et al., 2005). Under nonpathological processes, the capability of tissues to synthesize CoQ apparently decreases during aging (Kalen et al., 1989); however, it has been reported that CoQ biosynthesis can be affected by dietary supplementation (Kwong et al., 2002). Supplementation with CoQ10 or analogues has shown benefits in neurodegenerative processes such as PD (Sharma et al., 2004), HD (Beal and Shults, 2003) and AD (Gutzmann and Hadler, 1998), and also in mitochondrial disorders (Sobreira et al., 1997; Di Giovanni et al., 2001). In this study, we choose the intraperitoneal administration of CoQ10, instead of CoQ10 supplemented chow, because this experimental procedure allows us to control the exact amount of CoQ10 administered to each animal. Recently, Fernández-Ayala et al. (2005) reported that HL-60 cells incorporate exogenously added CoQ10 into mitochondria increasing complex I + III and complex II + III activities. Although, we did not observe any statistical difference in mitochondrial content of CoQ10 in the three experimental groups (data not shown), the improvement of mitochondrial function can be explained by the better performance of CoQ10 as mitochondrial electron carrier. The primary role of coenzyme Q is to transfer electrons between redox components of the electron transport chain, to create a proton gradient across the inner mitochondrial membrane and drive ATP formation (Ebadi et al., 2001). Besides its role in electron transfer reactions, CoQ10 is a powerful antioxidant that has been shown to be protective against oxidative stress (Singh et al., 1998; Hoppe et al., 1999; Tomasetti et al., 1999). In this line, McCarthy et al. (2004) reported that pre-incubation of SHSY-5Y cells with water-soluble CoQ10 inhibits ROS production induced by 117 paraquat, a nonselective herbicide. Pretreatment with CoQ10 also significantly reduced the number of apoptotic cells and DNA fragmentation. Furthermore, CoQ10 was able to inhibit mitochondrial ROS generation and inner mitochondrial depolarization induced by paraquat. Furthermore, it has been shown that supplementing the diet of rats with CoQ10 does not increase ROS production in mitochondria (Lass and Sohal, 2000; Kwong et al., 2002) but increases plasma membrane protection against oxidative stress (Gomez-Diaz et al., 2003), and extends life span (Quiles et al., 2004). In accordance, our results show that CoQ treatment avoids the increase in H2O2 production (Fig. 2) and the decrease in oxidative phosphorylation efficiency (Table 2) induced by Ah1 – 40. Recently, a CoQ10 binding site has been proposed to be located on the permeability transition pore where it may inhibit its opening and thus prevent collapse of mitochondrial membrane potential (Papucci et al., 2003). We observed that the effects of the vehicle solution (soybean oil) and CoQ10 were similar concerning glycemia (Table 1), RCR (Fig. 1) and repolarization levels (Table 2) suggesting that the effects of both components (soybean oil and CoQ10) are not synergistic nor potentiated since their coadministration did not increase the protection observed. The protective effect exerted by the soybean oil can be explained by the fact that it is a triglyceride derived from soybean that is rich in C-18 unsaturated components, tocopherols (specially g-tocopherol, a-tocopherol is present in modest amounts), ubiquinones and other antioxidants such as bioflavonoids and aromatic compounds (Cabrini et al., 2001; Lee et al., 2000). Several studies in animals and humans have shown that the consumption of soybean has beneficial effects in a variety of diseases including diabetes and obesity (Bhathena and Velasquez, 2002) and neurodegenerative disorders (Kim et al., 2000). In conclusion, our results show that CoQ10 treatment exerts a partial protection against Ah1 – 40-induced mitochondrial dysfunction. Given the importance of mitochondria as primary source of oxidative stress in AD and diabetes, the use of CoQ10 may be useful. However, the broad occurrence of both diseases, the nonregenerative nature of the CNS and the fact that AD diagnosis often does not occur until late in disease progression, suggest that the ideal antioxidant should be used as prophylactic treatment in aged population. Due to their low toxicity, low cost and their ability to target the earliest sources of oxidative stress, CoQ treatment alone or in combination with other antioxidants is particularly attractive. References Anderson, D., Yu, T.W., Wright, J., Ioannides, C., 1998. An examination of DNA strand breakage in the comet assay and antioxidant capacity in diabetic patients. Mutat. Res. 398, 151 – 161. Armstrong, D., Al-Awadi, F., 1991. Lipid peroxidation and retinopathy in streptozotocin induced diabetes. Free Radical Biol. Med. 11, 433 – 436. Barja, G., 1999. Mitochondrial oxygen radical generation and leak: sites of 118 P.I. Moreira et al. / Experimental Neurology 196 (2005) 112 – 119 production in states 4 and 3, organ specificity, and relation to aging and longevity. J. Bioenerg. Biomembr. 31, 347 – 366. Baynes, J.W., 1991. Role of oxidative stress in development of complications of diabetes. Diabetes 40, 405 – 412. Baynes, J.W., 1995. Reactive oxygen in the aetiology and complications of diabetes. In: Ioannides, C., Flatt, P.R. (Eds.), Drugs, Diet and Disease. Ellis Horwood, Hemel Hempstead. Beal, M.F., Shults, C.W., 2003. Effects of Coenzyme Q10 in Huntington’s disease and early Parkinson’s disease. BioFactors 9, 153 – 161. Beyer, R.F., Ernster, L., 1990. The antioxidant role of coenzyme Q. In: Lenaz, G., Barnabei, O., Battino, M. (Eds.), Highlights in Ubiquinone Research. Taylor and Francis, London, pp. 191 – 213. Bhathena, S.J., Velasquez, M.T., 2002. Beneficial role of dietary phytoestrogens in obesity and diabetes. Am. J. Clin. Nutr. 76, 1191 – 1201. Biessels, G.J., van der Heide, L.P., Kamal, A., 2002. Ageing and diabetes: implications for brain function. Eur. J. Pharmacol. 441, 1 – 14. Cabrini, L., Barzanti, V., Cipollone, M., Fiorentini, D., Grossi, G., Tolomelli, B., Zambonin, L., Landi, L., 2001. Antioxidants and total peroxyl radical-trapping ability of olive and seed oils. J. Agric. Food Chem. 49, 6026 – 6032. Cardoso, S.M., Santos, S., Swerdlow, R.H., Oliveira, C.R., 2001. Functional mitochondria are required for amyloid beta-mediated neurotoxicity. FASEB J. 15, 1439 – 1441. Collins, A.R., Raslova, K., Somorovska, M., Petrovska, H., Ondrusova, A., Vohnout, B., Fabry, R., Dusinska, M., 1998. DNA damage in diabetes: correlation with a clinical marker. Free Radical Biol. Med. 25, 373 – 377. Crane, F.L., Navas, P., 1997. The diversity of coenzyme Q function. Mol. Aspects Med. 18, S1 – S6. Dandona, P., Thusu, K., Cook, S., Snyder, B., Makowski, J., Armstrong, D., Nicotera, T., 1996. Oxidative damage to DNA in diabetes mellitus. Lancet 347, 444 – 445. Di Giovanni, S., Mirabella, M., Spinazzola, A., Crociani, P., Silvestri, G., Broccolini, A., Tonali, P., Di Mauro, S., Servidei, S., 2001. Coenzyme Q10 reverses pathological phenotype and reduces apoptosis in familial CoQ10 deficiency. Neurology 57, 515 – 518. Ebadi, M., Govitrapong, P., Sharma, S., Muralikrishnan, D., Shavali, S., Pellett, L., Schafer, R., Albano, C., Eken, J., 2001. Ubiquinone (coenzyme q10) and mitochondria in oxidative stress of parkinson’s disease. Biol. Signals Recept. 10, 224 – 253. Edlund, C., Soderberg, M., Kristensson, K., Dallner, G., 1992. Ubiquinone, dolichol, and cholesterol metabolism in aging and Alzheimer’s disease. Biochem. Cell Biol. 70, 422 – 428. Estabrook, R.E., 1967. Mitochondrial respiratory control and the polarographic measurement of ADP/O ratios. Methods Enzymol. 10, 41 – 47. Fernández-Ayala, D.J.M., López-Lluch, G., Garcı́a-Valdés, M., Arroyo, A., Navas, P., 2005. Specificity of coenzyme Q10 for a balanced function of respiratory chain and endogenous ubiquinone biosynthesis in human cells. Biochem. Biophys. Acta 1706, 174 – 183. Frolich, L., Blum-Degen, D., Bernstein, H.G., Engelsberger, S., Humrich, J., Laufer, S., Muschner, D., Thalheimer, A., Turk, A., Hoyer, S., Zochling, R., Boissl, K.W., Jellinger, K., Riederer, P., 1998. Brain insulin and insulin receptors in aging and sporadic Alzheimer’s disease. J. Neural Transm. 105, 423 – 438. Gavin, III JR., Alberti, K.G.M.M., Davidson, M.B., DeFronzo, R.A., Drash, A., Gabbe, S.G., Genuth, S., Harris, M.I., Kahn, R., Keen, H., Knowler, W.C., Lebovitz, H., Maclaren, N.K., Palmer, J.P., Raskin, P., Rizza, R.A., Stern, M.P., 1997. Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care 20, 1183 – 1197. Gerbitz, K.D., van den Ouweland, J.M., Maassen, J.A., Jaksch, M., 1995. Mitochondrial diabetes mellitus: a review. Biochim. Biophys. Acta 1271, 253 – 260. Gomez-Diaz, C., Buron, M.I., Alcain, F.J., Gonzalez-Ojeda, R., GonzalezReyes, J.A., Bello, R.I., Herman, M.D., Navas, P., Villalba, J.M., 2003. Effect of dietary coenzyme Q and fatty acids on the antioxidant status of rat tissues. Protoplasma 221, 11 – 17. Gornall, A.G., Bardawill, C.J., David, M.M., 1949. Determination of serum proteins by means of the biuret reaction. J. Biol. Chem. 177, 751 – 766. Goto, Y., Kakizaki, M., 1981. The spontaneous diabetic rat a model of noninsulin dependent diabetes mellitus. Proc. Jpn. Acad. 57, 381 – 384. Gutzmann, H., Hadler, D., 1998. Sustained efficacy and safety of idebenone in the treatment of Alzheimer’s disease: update on a 2-year double-blind multicentre study. J. Neurol. Transm. 54, 301 – 310. Hassing, L.B., Grant, M.D., Hofer, S.M., Pedersen, N.L., Nilsson, S.E., Berg, S., McClearn, G., 2004. Type 2 diabetes mellitus contributes to cognitive decline in old age: a longitudinal population-based study. J. Int. Neuropsychol. Soc. 10, 599 – 607. Hinokio, Y., Suzuki, S., Hirai, M., Chiba, M., Hirai, A., Toyota, T., 1999. Oxidative DNA damage in diabetes mellitus: its association with diabetic complications. Diabetologia 42, 995 – 998. Hoppe, U., Bergemann, J., Diembeck, W., Ennen, J., Gohla, S., Harris, I., Jacob, J., Kielholz, J., Mei, W., Pollet, D., Schachtschabel, D., Sauermann, G., Schreiner, V., Stab, F., Steckel, F., 1999. Coenzyme Q10, a cutaneous antioxidant and energizer. BioFactors 9, 371 – 378. Höppener, J.W., Ahrén, B., Lips, C.J., 2000. Islet amyloid and type 2 diabetes mellitus. N. Engl. J. Med. 343, 411 – 419. Hoyer, S., 1991. Abnormalities of glucose metabolism in Alzheimer’s disease. Ann. N. Y. Acad. Sci. 640, 53 – 58. Hoyer, S., 1998. Risk factors for Alzheimer’s disease during aging. Impacts of glucose/energy metabolism. J. Neural. Transm. 54, 187 – 194. Hoyer, S., 2002. The aging brain. Changes in the neuronal insulin/insulin receptor signal transduction cascade trigger late-onset sporadic Alzheimer disease (SAD). A mini-review. J. Neural. Transm. 109, 991 – 1002. Jameson, S., 1991. Coenzyme Q10 alpha-tocopherol, and free cholesterol levels in sera from diabetic patients. In: Folkers, K., Littarru, G., Yamagami, T. (Eds.), Biomedical and Clinical Aspects of Coenzyme Q. Elsevier Science, Amsterdam, pp. 151 – 158. Janssen, U., Vassiliadou, A., Riley, S.G., Phillips, A.O., Floege, J., 2004. The quest for a model of type II diabetes with nephropathy: the Goto Kakizaki rat. J. Nephrol. 17, 769 – 773. Kalen, A., Appelkvist, E.L., Dallner, G., 1989. Age-related changes in the lipid compositions of rat and human tissues. Lipids 24, 579 – 584. Kamo, N., Muratsugu, M., Hongoh, R., Kobatake, V., 1979. Membrane potential of mitochondria measured with an electrode sensitive to tetraphenylphosphonium and relationship between proton electrochemical potential and phosphorylation potential in steady state. J. Membr. Biol. 49, 105 – 121. Kim, H., Xia, H., Li, L., Gewin, J., 2000. Attenuation of neurodegeneration-relevant modifications of brain proteins by dietary soy. BioFactors 12, 243 – 250. Kitahara, M., Eyre, H.J., Lynch, R.E., Rallison, M.L., Hill, H.R., 1980. Metabolic activity of diabetics’ monocytes. Diabetes 29, 251 – 256. Koroshetz, W.J., Jenkins, B.G., Rosen, B.R., Beal, M.F., 1997. Energy metabolism defects in Huntington’s disease and effects of coenzyme Q10. Ann. Neurol. 41, 160 – 165. Kwong, L.K., Kamzalov, S., Rebrin, I., Bayne, A.C.V., Jana, C.K., Morris, P., Forster, M.J., Sohal, R.S., 2002. Effects of coenzyme Q(10) administration on its tissue concentrations, mitochondrial oxidant generation, and oxidative stress in the rat. Free Radical Biol. Med. 33, 627 – 638. Lass, A., Sohal, R.S., 2000. Effect of coenzyme Q(10) and alpha-tocopherol content of mitochondria on the production of superoxide anion radicals. FASEB J. 14, 87 – 94. Lee, K.G., Mitchell, A.E., Shibamoto, T., 2000. Determination of antioxidant properties of aroma extracts from various beans. J. Agric. Food Chem. 48, 4817 – 4820. Leibson, C.L., Rocca, W.A., Hanson, V.A., Cha, R., Kokmen, E., O’Brien, P.C., Palumbo, P.J., 1997. Risk of dementia among persons with diabetes mellitus: a population-based cohort study. Am. J. Epidemiol. 145, 301 – 308. Leinonen, J., Lehtimaki, T., Toyokuni, S., Okada, K., Tanaka, T., Hiai, H., Ochi, H., Laippala, P., Rantalaiho, V., Wirta, O., Pasternack, A., Alho, P.I. Moreira et al. / Experimental Neurology 196 (2005) 112 – 119 H., 1997. New biomarker evidence of oxidative DNA damage in patients with non-insulin-dependent diabetes mellitus. FEBS Lett. 417, 150 – 152. Lowell, B.B., Shulman, G.I., 2005. Mitochondrial dysfunction and type 2 diabetes. Science 307, 384 – 387. Lustbader, J.W., Cirilli, M., Lin, C., Xu, H.W., Takuma, K., Wang, N., Caspersen, C., Chen, X., Pollak, S., Chaney, M., Trinchese, F., Liu, S., Gunn-Moore, F., Lue, L.F., Walker, D.G., Kuppusamy, P., Zewier, Z.L., Arancio, O., Stern, D., Yan, S.S., Wu, H., 2004. ABAD directly links Ah to mitochondrial toxicity in Alzheimer’s disease. Science 304, 448 – 452. McCarthy, M.F., 1999. Can correction of sub-optimal coenzyme Q status improve b-cell function in type II diabetes? Med. Hypotheses 52, 368 – 397. McCarthy, S., Somayajulu, M., Sikorska, M., Borowy-Borowski, H., Pandey, S., 2004. Paraquat induces oxidative stress and neuronal cell death; neuroprotection by water-soluble coenzyme Q10. Toxicol. Appl. Pharmacol. 201, 21 – 31. Mitchell, P., 1991. The vital protonmotive role of coenzyme Q. In: Folkers, K., Littarru, G.P., Yamagami, T. (Eds.), Biochemical and Clinical Aspects of Coenzyme Q. Elsevier Science Publisher, Amsterdam, pp. 3 – 10. Moreira, P.I., Santos, M.S., Moreno, A., Oliveira, C., 2001. Amyloid betapeptide promotes permeability transition pore in brain mitochondria. Biosci. Rep. 21, 789 – 800. Moreira, P.I., Santos, M.S., Moreno, A., Rego, A.C., Oliveira, C., 2002. Effect of amyloid beta-peptide on permeability transition pore: a comparative study. J. Neurosci. Res. 69, 257 – 267. Moreira, P.I., Santos, M.S., Moreno, A.M., Seiça, R., Oliveira, C.R., 2003. Increased vulnerability of brain mitochondria in diabetic (Goto – Kakizaki) rats with aging and amyloid-beta exposure. Diabetes 52, 1449 – 1456. Moreno, A.J.M., Madeira, V.M.C., 1991. Mitochondrial bioenergetics as affected by DTT. Biochem. Biophys. Acta 1060, 166 – 174. Ott, A., Stolk, R.P., van Harskamp, F., Pols, H.A., Hofman, A., Breteler, M.M., 1999. Diabetes mellitus and the risk of dementia: the Rotterdam study. Neurology 53, 1937 – 1942. Papucci, L., Schiavone, N., Witort, E., Donnini, M., Lapucci, A., Empestini, A., Formigli, L., Orlandini, S.Z., Orlandini, G., Carella, G., Brancto, R., Capaccioli, S., 2003. Coenzyme Q10 prevents apoptosis by inhibiting mitochondrial depolarization independently of its free radical scavenging property. J. Biol. Chem. 278, 28220 – 28228. Pereira, C., Santos, M.S., Oliveira, C., 1998. Mitochondrial function 119 impairment induced by amyloid beta-peptide on PC12 cells. NeuroReport 9, 1749 – 1755. Pereira, C., Santos, M.S., Oliveira, C., 1999. Involvement of oxidative stress on the impairment of energy metabolism induced by A beta peptides on PC12 cells: protection by antioxidants. Neurobiol. Dis. 6, 209 – 219. Quiles, J.L., Ochoa, J.J., Huertas, J.R., Mataix, J., 2004. Coenzyme Q supplementation protects from age-related DNA double-strand breaks and increases lifespan in rats fed on a PUFA-rich diet. Exp. Gerontol. 39, 189 – 194. Rosenthal, R.E., Hamud, F., Fiskum, G., Varghese, P.J., Sharpe, S., 1987. Cerebral ischemia and reperfusion: prevention of brain mitochondrial injury by lidoflazine. J. Cereb. Blood Flow Metab. 7, 752 – 758. Selkoe, D.J., 2001. Alzheimer’s disease: genes, proteins, and therapy. Physiol. Rev. 81, 741 – 766. Seghrouchni, I., Drai, J., Bannier, E., Rivière, J., Calmard,, Garcia, I., Orgiazzi, J., Revol, A., 2002. Oxidative stress parameters in type I, type II and insuline treatment efficiency. Clin. Chim. Acta 321, 89 – 96. Serradas, P., Gangnerau, M.N., Giroix, M.H., Saulnier, C., Portha, B., 1998. Impaired pancreatic beta cell function in the fetal GK rat. Impact of diabetic inheritance. J. Clin. Invest. 101, 899 – 904. Sharma, S., Kheradpezhou, M., Shavali, S., El Refaey, H., Eken, J., Hagen, C., Ebadi, M., 2004. Neuroprotective actions of coenzyme Q10 in Parkinson’s disease. Methods Enzymol. 382, 488 – 509. Singh, R.B., Wander, G.S., Rastogi, A., Shukla, P.K., Mittal, A., Sharma, J.P., Mehrotra, S.K., Kapoor, R., Chopra, R.K., 1998. Randomized, double-blind placebo-controlled trial of coenzyme Q10 in patients with acute myocardial infarction. Cardiovasc. Drugs Ther. 12, 347 – 353. Sobreira, C., Hirano, M., Shanske, S., Keller, R.K., Haller, R.G., Davidson, E., Santorelli, F.M., Miranda, A.F., Bonilla, E., Mojon, D.S., Barreira, A.A., King, M.P., DiMauro, S., 1997. Mitochondrial encephalomyopathy with coenzyme Q10 deficiency. Neurology 48, 1238 – 1243. Sohmiya, M., Tanaka, M., Suzuki, Y., Tanino, Y., Okamoto, K., Yamamoto, Y., 2005. An increase of oxidized coenzyme Q-10 occurs in the plasma of sporadic ALS patients. J. Neurol. Sci. 228, 49 – 53. Takuma, K., Yao, J., Huang, J., Xu, H., Chen, X., Luddy, J., Trillat, A.C., Stern, D.M., Arancio, O., Yan, S.S., 2005. ABAD enhances Abeta-induced cell stress via mitochondrial dysfunction. FASEB J. 19, 597 – 598. Tomasetti, M., Littarru, G.P., Stocker, R., Alleva, R., 1999. Coenzyme Q10 enrichment decreases oxidative DNA damage in human lymphocytes. Free Radical Biol. Med. 27, 1027 – 1032. Wallace, D.C., 1999. Mitochondrial diseases in man and mouse. Science 283, 1482 – 1488.
Baixar