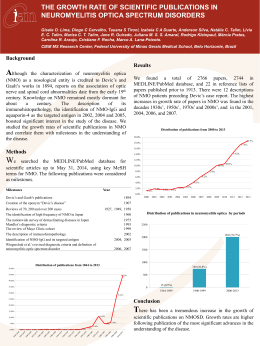
Escola Superior de Ciências da Saúde Clube de revista: Associação entre defeitos cardíacos congênitos e pequeno para a idade gestacional Internos: Eduardo Campos Guilherme Aroeira Jorge Alberto Coordenação: Paulo R. Margotto www.paulomargotto.com.br Introdução • Prevalência: 8-11/1000 nascidos vivos • EUA: ~32000-44000 Cardiopatias congênitas (CHDs)/ano • Elevados custos (cirurgias;hospitalizações) • Fatores prognósticos: complexidade da lesão cardíaca, peso ao nascer, graus de maturidade pulmonar e de prematuridade Introdução • Pós-correção/paliação cirúrgica: limitação do crescimento – Desordens metabólicas – Ventilação mecânica prolongada – Alto risco de infecções – Hospitalizações prolongadas Introdução • Revisão bibliográfica – Associação positiva entre CHDs e PIG/Baixo peso ao nascer (risco ~1,8-3,6) – Ausência de ajuste dos fatores maternos e fetais determinantes do crescimento – Etiologia multifatorial (PIGxCHDs) Objetivo Investigar a associação entre CHDs e RN-PIG em uma grande amostra populacional ajustando os fatores maternos e fetais envolvidos Materiais e métodos • Seleção da amostra – Nascidos entre outubro de 1997 e dezembro de 2002 e cadastrados no National Birth Defects Prevention Study (NBDPS) – Registros de vigilância (8 estados) Materiais e métodos • Seleção de casos – Criança sem doenças genéticas – CHDs: <1 ano; Ecocardiograma,cirúrgico,cateterismo ou autópsia – Mãe fluente em inglês ou espanhol – Criança não foi colocada para adoção ou cuidados adotivos Materiais e métodos • Seleção de casos – Gestações únicas – Sem doenças extracardíacas Materiais e métodos • Seleção controles – Crianças saudáveis nascidas no mesmo período e nos mesmos estados – Selecionadas através das certidões de nascimento ou registros de alta Materiais e métodos • ~ 482000 nascidos/ano no período • 18% das mães dos casos e 21% das mães dos controles recusaram-se a participar do NBDPS Materiais e métodos • Classificação das CHDs – Lesões de grandes vasos – Defeitos septais – Lesões obstrutivas direita – Lesões obstrutivas esquerdas Materiais e métodos • CHDs excluídas – Dupla saída de ventrículo direito (VD) – Lesões cardíacas com três ou mais defeitos – Defeito venoso pulmonar parcial ou total Materiais e métodos • Variáveis maternas e infantis: – – – – – – – – – – – – Idade Raça/etnia Nível sócio-econômico Ganho de peso gestacional Paridade Diabetes Mellitus prévia Hipertensão Arterial Infecções (CMV,Rubeóla etc...) Tabagismo Etilismo Drogas Ilícitas Sexo da criança Materiais e métodos • Parâmetros de crescimento: – PIG: Peso de nascimento < que percentil 10 – Idade gestacional: exame clínico/DPP Materiais e métodos • Análise estatística: – Comparação entre CHDs e controles: MannWhitney/Wilcoxon rank sum test – Ajuste de variáveis: regressão linear, Odds Ratios e IC de 95% Resultados Discussão • Relação CHDs x PIGs – Crianças com CHDs apresentam maior risco de prematuridade e de serem PIG – Concordância com a literatura internacional • Relação Controles x PIGs – Discordância com a literatura internacional Discussão • Etiologia: CHDs e PIGs – Fatores de risco comuns – Fatores de risco independentes – CHDsPIGs Discussão • Repercussões pré e pós-natais do estudo – Nutrição adequada – Monitorização cuidadosa do crescimento fetal e neonatal – Manejo dependente do tipo de lesão cardíaca Discussão • Limitações do estudo – Dificuldade em classificar os prematuros Discussão • Novos estudos buscando avaliar relações etiológicas PIGsxCHDs – Implementar medidas pré e pós-natais • Diagnóstico precoce • Monitorização cuidadosa as Conclusão • Crianças com cardiopatias congênitas apresentam um risco duas vezes maior, aproximadamente, de serem PIGs. Pigs com CHDs tem suas condutas clínicas, resposta terapêutica e prognóstico neonatal afetados.Embora a etiologia do retardo do crescimento entre crianças com CHDs seja incerto, novos estudos podem descobrir uma patogênese comum ou uma relação causal entre PIG e CHD. ABSTRACT: • OBJECTIVES. Infants with congenital heart defects may experience inhibited growth • • • • • during fetal life. In a large case-control study, we addressed the hypothesis that infants with congenital heart defects are more likely to be small for gestational age than infants without congenital heart defects after controlling for selected maternal and infant characteristics. METHODS. Using data from population-based birth defect registries, the National Birth Defects Prevention Study enrolled infants with nonsyndromic congenital heart defects (case subjects) and infants without congenital heart defects or any other birth defect (control subjects). Small for gestational age was defined as birth weight below the 10th percentile for gestational age and gender. Association between congenital heart defects and small for gestational age was examined by conditional logistic regression adjusting for maternal covariates related to fetal growth. RESULTS. Live-born singleton infants with congenital heart defects (case subjects, n = 3395) and live-born singleton infants with no birth defect (control subjects, n = 3924) were included in this study. Case subjects had lower birth weights compared with control subjects. Small for gestational age was observed among 15.2% of case subjects and among only 7.8% of control subjects. Congenital heart defect infants were significantly more likely to be small for gestational age than control infants. CONCLUSIONS. Infants with congenital heart defects are approximately twice as likely to be small for gestational age as control subjects. Small for gestational age status may affect clinical management decisions, therapeutic response, and prognosis of neonates with congenital heart defects. Although the etiology of growth retardation among infants with congenital heart defects is uncertain, further exploration may uncover a common pathogenesis or causal relationship between congenital heart defects and small for gestational age. Key Words: small for gestational age • cardiac disease • congenital anomalies Abbreviations: CHD—congenital heart defect • NBDPS—National Birth Defects Prevention Study • OR—odds ratio • CI—confidence interval Referências do artigo: • Boneva RS, Botto LD, Moore CA, Yang Q, Correa A, Erickson JD. Mortality associated • • • • • • • • • with congenital heart defects in the United States: trends and racial disparities, 1979– 1997. Circulation. 2001;103 :2376 –2381[Abstract/Free Full Text] Cleves MA, Ghaffar S, Zhao W, Mosley BS, Hobbs CA. First-year survival of infants born with congenital heart defects in Arkansas (1993–1998): a survival analysis using registry data. Birth Defects Res. Part A Clin Mol Teratol. 2003;67 :662 –668[CrossRef] Tilford JM, Robbins JM, Hobbs CA. Improving estimates of caregiver time cost and family impact associated with birth defects. Teratology. 2001;64(suppl 1) :S37 –S41 Waitzman NJ, Romano PS, Scheffler RM. Estimates of the economic costs of birth defects. Inquiry. 1994;31 :188 –205[ISI][Medline] Ades A, Johnson BA, Berger S. Management of low birth weight infants with congenital heart disease. Clin Perinatol. 2005;32 :999 –xi[CrossRef][ISI][Medline] Peterson RE, Wetzel GT. Growth failure in congenital heart disease: where are we now? Curr Opin Cardiol. 2004;19 :81 –83[CrossRef][ISI][Medline] Castaneda AR, Jonas RA, Mayer JE Jr, Hanley FL. Cardiac Surgery of the Neonate and Infant. Philadelphia, PA: Elsevier; 2004 Bove T, Francois K, DeGroote K, et al. Outcome analysis of major cardiac operations in low weight neonates. Ann Thorac Surg. 2004;78 :181 –187[Abstract/Free Full Text] Rossi AF, Seiden HS, Sadeghi AM, et al. The outcome of cardiac operations in infants weighing two kilograms or less. J Thorac Cardiovasc Surg. 1998;116 :28 – 35[Abstract/Free Full Text] Rosenthal GL, Wilson PD, Permutt T, Boughman JA, Ferencz C. Birth weight and cardiovascular malformations: a population-based study. The Baltimore-Washington Infant Study. Am J Epidemiol. 1991;133 :1273 –1281[Abstract/Free Full Text] • Khoury MJ, Erickson JD, Cordero JF, McCarthy BJ. Congenital malformations and intrauterine • • • • • • • • • growth retardation: a population study. Pediatrics. 1988;82 :83 –90[Abstract/Free Full Text] Kramer HH, Trampisch HJ, Rammos S, Giese A. Birth weight of children with congenital heart disease. Eur J Pediatr. 1990;149 :752 –757[CrossRef][ISI][Medline] Levin DL, Stranger P, Kitterman JA, Heymann MA. Congenital heart disease in low birth weight infants. Circulation. 1975;52 :500 –503[Abstract/Free Full Text] Cedergren MI, Kallen BA. Obstetric outcome of 6346 pregnancies with infants affected by congenital heart defects. Eur J Obstet Gynecol Reprod Biol. 2006;125 :211 – 216[CrossRef][ISI][Medline] Jacobs EG, Leung MP, Karlberg J. Birthweight distribution in southern Chinese infants with symptomatic congenital heart disease. J Paediatr Child Health. 2003;39 :191 – 196[ISI][Medline] Ferencz C, Loffredo CA, Correa A, Wilson PD. Genetic and Environmental Risk Factors of Major Cardiovascular Malformations: The Baltimore-Washington Infant Study 1981–1989. Armonk, NY: Futura Publishing Co, Inc; 1997 Dejin-Karlsson E, Hanson BS, Ostegren PO, Sjoberg WO, Marsal K. Does passive smoking in early pregnancy increase the risk of small-for-gestational-age infants? Am J Public Health. 1998;88 :1523 –1527[Abstract/Free Full Text] Infante-Rivard C, Weinberg CR, Guiguet M. Xenobiotic-metabolizing genes and small-forgestational-age births: interaction with maternal smoking. Epidemiology. 2006;17 :38 – 46[CrossRef][ISI][Medline] Salihu HM, Shumpert MN, Aliyu MH, Kirby RS, Alexander GR. Smoking-associated fetal morbidity among older gravidas: a population study. Acta Obstet Gynecol Scand. 2005;84 :329 –334[CrossRef][ISI][Medline] Mitchell EA, Thompson JA, Robinson E, et al. Smoking, nicotine and tar and risk of small for gestational age babies. Acta Paediatr. 2002;91 :323 –328[CrossRef][ISI][Medline] • Chiolero A, Bovet P, Paccaud F. Association between maternal smoking and low birth weight in • • • • • • • • • • Switzerland: the EDEN study. Swiss Med Wkly. 2005;135 :525 –530[ISI][Medline] Hobbs CA, James SJ, Jernigan S, et al. Congenital heart defects, maternal homocysteine, smoking, and the 677 C>T polymorphism in the methylenetetrahydrofolate reductase gene: evaluating gene-environment interactions. Am J Obstet Gynecol. 2006;194 :218 – 224[CrossRef][ISI][Medline] Woods SE, Raju U. Maternal smoking and the risk of congenital birth defects: a cohort study. J Am Board Fam Pract. 2001;14 :330 –334[Medline] Kallen K. Maternal smoking and congenital heart defects. Eur J Epidemiol. 1999;15 :731 – 737[CrossRef][ISI][Medline] Hobbs CA, Malik S, Zhao, W, James SJ, Melnyk S, Cleves MA. Maternal homocysteine and congenital heart defects. J Am Coll Cardiol. 2006;47 :683 –685[Free Full Text] Yajnik CS, Deshpande SS, Panchanadiker AV, et al. Maternal total homocysteine concentration and neonatal size in India. Asia Pac J Clin Nutr. 2005;14 :179 –181[ISI][Medline] Hobbs CA, Cleves MA, Melnyk S, Zhao W, James SJ. Congenital heart defects and abnormal maternal biomarkers of methionine and homocysteine metabolism. Am J Clin Nutr. 2005;81 :147 –153[Abstract/Free Full Text] Leiva MC, Tolosa JE, Binotto CN, et al. Fetal cardiac development and hemodynamics in the first trimester. Ultrasound Obstet Gynecol. 1999;14 :169 –174[CrossRef][ISI][Medline] Clapp JF, III. The clinical significance of asymmetric intrauterine growth retardation. Pediatr Ann. 1996;25 :223 –227[ISI][Medline] Yoon PW, Rasmussen SA, Lynberg MC, et al. The National Birth Defects Prevention Study. Public Health Rep. 2001;116(suppl 1) :32 –40 Lin A, Botto L, Ghaffar S, Cosper C, Correa A. The National Birth Defects Prevention Study. Classification of cardiovascular malformations in the National Birth Defects Prevention Study [abstract]. Am J Hum Genet. • Cogswell ME, Yip R. The influence of fetal and maternal factors on the distribution of • • • • • • • • birth weight. Semin Perinatol. 1995;19 :222 –240[CrossRef][ISI][Medline] Martikainen MA. Effects of intrauterine growth retardation and its subtypes on the development of the preterm infant. Early Hum Dev. 1992;28 :7 – 17[CrossRef][ISI][Medline] Ashworth A. Effects of intrauterine growth retardation on mortality and morbidity in infants and young children. Eur J Clin Nutr. 1998;52(suppl 1) :S34– S41[CrossRef] Alexander GR, Kogan M, Bader D, Carlo W, Allen M, Mor J. US birth weight/gestational age-specific neonatal mortality: 1995–1997 rates for whites, Hispanics, and blacks. Pediatrics. 2003;111 (1). Available at: www.pediatrics.org/cgi/content/full/111/1/e61 Zhang J, Bowes WA Jr. Birth-weight-for-gestational-age patterns by race, sex, and parity in the United States population. Obstet Gynecol. 1995;86 :200 –208[Abstract] Alexander GR, Himes JH, Kaufman RB, Mor J, Kogan M. A United States national reference for fetal growth. Obstet Gynecol. 1996;87 :163 –168[Abstract] Clausson B, Cnattingius S, Axelsson O. Preterm and term births of small for gestational age infants: a population-based study of risk factors among nulliparous women. Br J Obstet Gynaecol. 1998;105 :1011 –1017[ISI][Medline] Tanner K, Sabrine N, Wren C. Cardiovascular malformations among preterm infants. Pediatrics. 2005;116 (6). Available at: www.pediatrics.org/cgi/content/full/116/6/e833 Snijders RJ, Abbas A, Melby O, Ireland RM, Nicolaides KH. Fetal plasma erythropoietin concentration in severe growth retardation. Am J Obstet Gynecol. 1993;168 :615 – 619[ISI][Medline] • Villar J, Merialdi M, Gulmezoglu AM, et al. Characteristics of randomized controlled • • • • • • trials included in systematic reviews of nutritional interventions reporting maternal morbidity, mortality, preterm delivery, intrauterine growth restriction and small for gestational age and birth weight outcomes. J Nutr. 2003;133 :1632S – 1639S[Free Full Text] Hobbins J. Morphometry of fetal growth. Acta Paediatr. 1997;423(suppl) :165 –168 Soothill PW, Bobrow CS, Holmes R. Small for gestational age is not a diagnosis. Ultrasound Obstet Gynecol. 1999;13 :225 –228[CrossRef][ISI][Medline] Schuurmans FM, Pulles-Heintzberger CF, Gerver WJ, Kester AD, Forget PP. Long-term growth of children with congenital heart disease: a retrospective study. Acta Paediatr. 1998;87 :1250 –1255[CrossRef][ISI][Medline] Chatelain P. Children born with intra-uterine growth retardation (IUGR) or small for gestational age (SGA): long term growth and metabolic consequences. Endocr Regul. 2000;34 :33 –36[Medline] Strauss RS, Dietz WH. Effects of intrauterine growth retardation in premature infants on early childhood growth. J Pediatr. 1997;130 :95 –102[CrossRef][ISI][Medline] Albertsson-Wikland K, Karlberg J. Postnatal growth of children born small for gestational age. Acta Paediatr. 1997;423(suppl) :193 –195 Ddo Eduardo Ddo Jorge Obrigado. Ddo Guilherme
Baixar