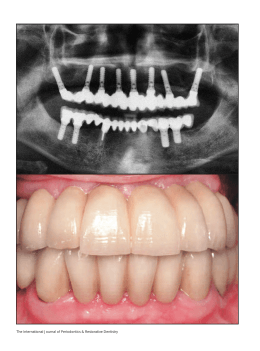
ORIGINAL ARTICLE Short Implant to Support Maxillary Restorations: Bone Stress Analysis Using Regular and Switching Platform Nivaldo Antônio de Carvalho, DDS, Erika Oliveira de Almeida, DDS, MS, Eduardo Passos Rocha, DDS, MS, PhD,* Amı́lcar Chagas Freitas Jr, DDS, MS, Rodolfo Bruniera Anchieta, DDS, MS, and Sidney Kina, DDS, MSÞ Purpose: The aim of this study was to evaluate stress distribution on peri-implant bone simulating the influence of implants with different lengths on regular and switching platforms in the anterior maxilla by means of three-dimensional finite element analysis. Materials and Methods: Four mathematical models of a central incisor supported by an external hexagon implant (diameter, 5.0 mm) were created, varying the length (15.0 mm for long implants [L] and 7.0 mm for short implants [S]) and the diameter of the abutment platform (5.0 mm for regular models [R] and 4.1 mm for switching models [S]). The models were created using the Mimics 11.11 (Materialise) and SolidWorks 2010 (Inovart) software. Numerical analysis was performed using ANSYS Workbench 10.0 (Swanson Analysis System). Oblique forces (100 N) were applied to the palatine surface of the central incisor. The bone/ implant interface was considered perfectly integrated. Maximum (Rmax) and minimum (Rmin) principal stress values were obtained. Results: For the cortical bone, the highest stress values (Rmax) were observed in the SR (73.7 MPa) followed by LR (65.1 MPa), SS (63.6 MPa), and LS (54.2 MPa). For the trabecular bone, the highest stress values (Rmax) were observed in the SS (8.87 MPa) followed by the SR (8.32 MPa), LR (7.49 MPa), and LS (7.08 MPa). Conclusions: The influence of switching platform was more evident for the cortical bone in comparison with the trabecular bone for the short and long implants. The long implants showed lower What Is This Box? A QR Code is a matrix barcode readable by QR scanners, mobile phones with cameras, and smartphones. The QR Code links to Supplemental Digital Content from this article. From the *Department of Dental Materials and Prosthodontics, Araçatuba Dental School, UNESP - Univ. Estadual Paulista; and †Post Graduate Center, São Leopoldo Mandic School Campinas, São Paulo, Brazil. Received December 15, 2010. Accepted for publication March 21, 2011. Address correspondence and reprint requests to Erika Oliveira de Almeida, DDS, MS, UNESP - Departamento de Materiais Odontológicos e Prótese, R. José Bonifácio, 1193, Araçatuba - SP, CEP 16015-050, Brazil; E-mail: [email protected] This study was supported by the Sao Paulo Research Foundation (FAPESP - Brazil, no. 2008/00209-9). The authors report no conflicts of interest. Copyright * 2012 by Mutaz B. Habal, MD ISSN: 1049-2275 DOI: 10.1097/SCS.0b013e31824dbab7 The Journal of Craniofacial Surgery stress values in comparison to the short implants, mainly when the switching platform was used. Key Words: Bone biology, implantology, osseointegration, prosthodontics (J Craniofac Surg 2012;23: 00Y00) A lthough high long-term success rates with osseointegrated implants for the treatment of completely or partially edentulous patients have been reported,1Y3 implant failure, marginal bone loss, and patient discomfort still occur.4Y9 Bone loss usually begins at the crestal area of the cortical bone and can progress toward the apical region, jeopardizing the longevity of the implant and prosthesis.8 It is suggested that optimization of an implant may favor the mechanical environment for bone maintenance.3 One interesting proposal suggests that a so-called platform switching protocol could ensure better bone levels, at least in the short term.10 According to this principle, the abutment/implant joint is moved to the center of the implant and keeps far from the periimplant bone, which is maintained away from the inflammatory cells.11,12 Consequently, if this concept is proven to be predictable, it would certainly impact the aesthetic outcome of implants placed in the aesthetic zone and should be tested.11Y13 The maxilla may present insufficient bone quantity for insertion of long implants, which is a prosthetic-surgical challenge owing to reduced bone quality and quantity usually represented by bone types III and IV.14 In these conditions, the placement of short implants has been introduced as an alternative treatment strategy to deviate from advanced surgical techniques.15Y17 Clinical studies have demonstrated that a short implant may be a viable long-term solution for regions with limited bone height,18Y20 although the risk seems to increase if the crown-to-implant ratio exceeds the guidelines established for natural teeth (1:1).21 Numerous publications have addressed the issue of implant length as a predictor of implant survival.22Y28 These studies have produced conflicting results. Some studies report high failure rates with short implants,22Y24 whereas other studies report high survival rates.20,25Y28 Considering the need for additional studies to evaluate stress distribution with short implants and its association with switching platform, the aim of this study was to evaluate the influence of switching platform in short implants in the anterior region of maxilla by means of the three-dimensional finite element analysis. MATERIALS AND METHODS After approval by the human ethics committee (process no. 2008/01845) and signing of the informed consent, a tomographic & Volume 23, Number 3, May 2012 Copyright © 2012 Mutaz B. Habal, MD. Unauthorized reproduction of this article is prohibited. 1 The Journal of Craniofacial Surgery de Carvalho et al & Volume 23, Number 3, May 2012 TABLE 1. Materials Properties Used in the Model Material FIGURE 1. Models with short implants and long implants. examination of the maxilla of a patient was conducted to obtain tomographic images in DICOM format. Four mathematical models representing the anterior segment of the maxilla were fabricated using Mimics 11,11 (Materialise, Leuven, Belgium) and Solid Works 2010 (Inovart, São Paulo, Brazil) software. All models were restored with a crown cemented on the abutment, varying the implant length (7.0 and 15.0 mm) and the platform diameter (4.1 and 5.0 mm), simulating 2 regular situations (short regular model [SR] and long regular model [LR]) and 2 switching situations (short switching model [SS] and long switching model [LS]; Fig. 1). The external hexagon implants SIN (Sistema de Implante, SP, Brazil) Revolution (5.0 15.0 and 5.0 7.0 mm) were restored with a crown IPS e-max Press (Ivoclar Vivadent, Schaan, Liechtenstein) cemented on the abutment (4.1 and 5.0 mm in diameter) with the cement Variolink II (Ivoclar Vivadent), 0.05 mm in thickness. Then, the assembly was inserted in the anterior segment of the maxilla with cortical and trabecular bone corresponding to the region of the right central incisor (Figs. 2A, B). The crown presented 13.07 mm in height, 8.8 mm in mesiodistal width, and 7.1 mm buccal-lingual width. After fabrication, the models were transferred to the finite element software Ansys Workbench 10.0 (Swanson Analysis, Inc, Houston, PA) to determine the regions and generate the finite element mesh. The mechanical properties of the structures were based on the specific literature (Table 1).29,30 All materials were considered isotropic, homogeneous, and linearly elastic. The bone/implant interface was considered as perfectly integrated.31,32 One oblique loading (45 degrees) was applied on the palatine surface of the crown of the right central incisor (100 N; Fig. 3A).33 The fixed support was determined in the 3 Cartesian axes (x = y = z = 0) to characterize the boundary condition (Fig. 3B). Parabolic tetrahedral elements of 0.8 mm in dimension were used for the mesh (Fig. 2C). The refinement of the mesh was established through convergence analysis (6%).29 The models presented the number of elements ranging from 144,882 to 154,622 and the number of nodes ranging from 230,600 to 242,353. For analysis of the results, the maximum (Rmax) and minimum (Rmin) principal stress values for the cortical and trabecular bone were obtained. According to Dejak and Mlotkowsk,34 these Cortical bone Trabecular bone (type III) Implant Abutment and screw Variolink II IPS e-max Press Elastic Poisson Modulus (MPa) Ratio 13.800 1.600 110.000 100.000 8.300 95.000 0.26 0.3 0.35 0.35 0.3 0.3 References Huang et al. (2008) Tada et al. (2003) Huang et al. (2008) Huang et al. (2008) Manufacturer’s specifications Manufacturer’s specifications analyses criteria are appropriate for predicting failures in nonductile materials. RESULTS For the cortical bone, the maximum (Rmax) principal stress was highest in SR (73.7 MPa) followed by LR (65.1 MPa), SS (63.6 MPa), and LS (54.2 MPa; Fig. 6). The influence of switching platform was evident for the short and long implants. In the short switching model (SS), the Rmax decreased 13.7% in comparison to the short regular model (SR), whereas in the long switching model (LS), the Rmax decreased 16.74% in comparison to the long regular model (LR). The increase in implant length showed a decrease of 11.6% in the Rmax for the short regular model (SR) in comparison to the long regular model (LR) and of 14.7% for the short switching model (SS) in comparison to the long switching model (LS). The minimum (Rmin) principal stress was highest in SR (1.66 MPa) and the other models exhibited similar values of Rmin (0.48 MPa for LS, j0.32 MPa for LR, and 0.20 for SS; Fig. 4). For the trabecular bone, the maximum (Rmax) principal stress was highest in SS (8.87 MPa) followed by SR (8.32 MPa), LR (7.49 MPa), and LS (7.08 MPa; Fig. 5). The influence of switching platform was more evident for cortical bone in comparison to the trabecular bone. In the short regular model (SR), the Rmax decreased 6.2% in comparison to the short switching model (SS), whereas in the long switching model (LS), the Rmax decreased 5.4% in comparison to the long regular model (LR). The influence of the implant length was more evident for trabecular bone of the switching models in comparison to the cortical models. The increase in implant length showed a decrease of 9.9% in the Rmax for the short regular model (SR) in comparison to the long regular model (LR) and of 20.1% for the short switching model (SS) in comparison to the long switching model (LS). The minimum (Rmin) principal stress was highest in SR (1.66 MPa) and the others models presented similar values of Rmin (0.48 MPa for LS, j0.32 MPa for LR, and 0.20 for SS; Fig. 5). For all models (SR, LR, SS, and LS), the maximum principal stress (Rmax) was concentrated on the lingual region of the cortical bone near the platform (Fig. 6). DISCUSSION The results of the current study demonstrated that the use of switching platform reduced the stress in the peri-implant bone, FIGURE 2. A, Representative complete model with cortical and trabecular bone. B, Invisible model to show the components. C, Finite element mesh of the model. 2 FIGURE 3. A, Loading. B, Fixed support conditions. * 2012 Mutaz B. Habal, MD Copyright © 2012 Mutaz B. Habal, MD. Unauthorized reproduction of this article is prohibited. The Journal of Craniofacial Surgery & Volume 23, Number 3, May 2012 Stress Distribution on Peri-Implant Bone FIGURE 6. Rmax for the cortical bone in SR, LR, SS, and LS. FIGURE 4. Rmax and Rmin (MPa) for cortical bone in SR, LR, SS, and LS. mainly in the cortical bone that exhibited a decrease in maximum principal stress values (Rmax) of 13.7% for the short implants and 16.74% for the long implants. These results are in agreement with Hsu et al35 who reported that models with switching platform exhibited a decrease in stress values nearly 10% in comparison to the models with regular platform. These findings might be explained by the biologic width formed near the implant/abutment interface, which may be caused by the microgap located at the edge of the interface. For the platform switching protocol, the biologic width extends horizontally from the abutment to the edge of the collar of the implant and the remainder extends apically to this region, which should facilitate bone preservation.36 This observation provides direct evidence that the biologic process resulting in the formation of the biologic dimension and position of hard and soft tissues around a dental implant has a great capacity to influence and direct the bone remodeling process than does the ability of a bone loading implant surface to resist the resorptive process of crestal bone remodeling that results from the biologic attempt to create adequate spaces for soft tissue attachment to the implants.10 Similar results were confirmed by the retrospective study of Prosper et al37 when observed that the switching platform reduced the bone loss for both immediate loading and conventional surgical protocol with 2 steps. Calvo-Guirado et al38 radiographically observed reduced bone loss for cases with switching platform and stated that bone maintenance may result from alteration in the biologic process. Romanos and Nentwig39 suggested that the reduced bone loss generated by switching platform depends on the primary stability of the implant after surgery, interarch occlusal stability, and controlled diet during osseointegration. However, other studies36,40,41 found similar bone loss for both switching and regular platforms. This may result from the insertion of implants immediately after exodontia in all these studies with immediate loading, which may have caused similar bone loss for all groups. Chaushu et al42 and Maló et al43 reported lower success rates for implant inserted immediately after exodontia (75%) in comparison to the implants inserted not immediately (100%). In the present study, the stress was concentrated on the lingual region of the cortical bone. The same region was found by Hsu et al35 in experimental and FE models, especially under lateral loading. The current study found that a long implant and a switching platform provided biomechanical benefits for the delay-loaded implants. However, the decrease in the stress value for the trabecular bone was higher when the implant length was evaluated for the models with switching platform, with a 20.1% decrease in maximum principal stress (Rmax) from model SS to model LS. The decrease in crestal bone stress induced by the increase in the implant length in the maxilla was confirmed by Otate et al,44 who found that short implants presented statistically significant differences, with early loss of implant in comparison to the long implant. Moreover, other authors45 believe that, for long-term evaluation, the implant length could be more important than the diameter is because, before oral cavity exposure and loading, vertical osseous loss is present, and it can be close to 0.2 mm/y; in the future, the implant may lose important contact between the bone and the implant surface. Although a linear behavior was established between the structures in the present study, it can be suggested that the switching platform or long implants improve stress distribution in the periimplant maxillary bone. Additional studies are required to conduct an anisotropic evaluation of the properties of cortical and medullary bone using friction coefficients to simulate an immediate loading considering the influence of the switching platform in short implants in the maxilla. In addition, longitudinal clinical studies and animal studies should be conducted to complement the findings of the present study. CONCLUSIONS According to the methodology used, it was concluded that: 1. the influence of the switching platform was more evident in the cortical bone in comparison to the medullary bone, 2. the switching platform reduced the maximum principal stress (Rmax) of the short and long implants, and 3. the long implant presented a lower value of maximum principal stress (Rmax) than the short implant did, mainly when the switching platform was associated. REFERENCES FIGURE 5. Rmax and Rmin (MPa) for trabecullar bone in SR, LR, SS, and LS. 1. Kirsch A, Mentag P. The TMZ endosseous two phase implant systems: a complete oral rehabilitation treatment concept. J Oral Implantol 1986;12:576Y589 2. Eckert SE, Parein A, Myshin HL, et al. Validation of dental implant systems through a review of literature supplied by systems manufacturers. J Prosthet Dent 1997;77:271Y279 3. Qian L, Todo M, Matsushita Y, et al. Effects of implant diameter, insertion depth, and loading angle on stress/strain fields in implant/jawbone systems: finite element analysis. Int J Oral Maxillofac Implants 2009;24:877Y866 * 2012 Mutaz B. Habal, MD Copyright © 2012 Mutaz B. Habal, MD. Unauthorized reproduction of this article is prohibited. 3 de Carvalho et al The Journal of Craniofacial Surgery 4. Ibbott CG. In vivo fracture of a basket-type osseointegrating dental implant: a case report. Int J Oral Maxillofac Implants 1989;4:255Y256 5. Friberg B, Jemt T, Lekholm U. Early failure in 4641 consecutively placed Brånemark dental implants: a study from stage I surgery to the connection of completed prosthesis. Int J Oral Maxillofac Implants 1991;6:142Y146 6. Adell R, Eriksson B, Lekholm M, et al. A long term follow-up study of osseointegrated implants in the treatment of totally edentulous jaws. Int J Oral Maxillofac Implants 1990;5:347Y359 7. Frost HM. Skeletal Structural Adaptations to Mechanical Usage (SATMU): refining Wolff’s law: the bone remodeling problem. Anat Rec 1990;226:403Y419 8. Isidor F. Loss of osseointegration caused by occlusal load of oral implants: a clinical and radiographic study in monkeys. Clin Oral Implants Res 1996;7:143Y152 9. Oh TJ, Yoon J, Misch CE, et al. The causes of early implant bone loss: myth or science? J Periodontol 2002;73:322Y333 10. Lazzara RJ, Porter SS. Platform switching: a new concept in implant dentistry for controlling postrestorative crestal bone levels. Int J Periodontics Restorative Dent 2006;26:9Y17 11. Cappiello M, Luongo R, Di lorio D, et al. Evaluation of peri-implant bone loss around platform-switching implants. Int J Periodontics Restorative Dent 2008;28:347Y355 12. Canullo L, Fedele GR, Iannello G, et al. Platform switching and marginal bone-level alterations: the results of a randomized-controlled trial. Clin Oral Implants Res 2010;21:115Y121 13. Maeda Y, Miura J, Taki I, et al. Biomechanical analysis on platform switching: in there any biomechanical rationale? Clin Oral Implants Res 2007;18:581Y584 14. Capelli M, Zuffetti F, Del Fabbro M, et al. Immediate rehabilitation of the completely edentulous jaw with fixed prosthesis supported by either upright or tilted implants: a multicenter clinical study. Int J Oral Maxillofac Implant 2007;22:639Y644 15. Hagi D, Deporter DA, Pilliar RM, et al. A targeted review of study outcomes with short (G or = 7 mm) endosseous dental implants placed in partially edentulous patients. J Periodontol 2004;75:798Y804 16. das Neves FD, Fones D, Bernardes SR, et al. Short implantsVan analysis of longitudinal studies. Int J Oral Maxillofac Implants 2006;21:86Y93 17. Renouard F, Nisand D. Impact of implant length and diameter on survival rates. Clin Oral Implants Res 2006;17:35Y51 18. Deporter DA, Todescan R, Watson PA, et al. Use of the Endopore dental implants to restore single teeth in the maxilla: protocol and early results. Int J Oral Maxillofac Implants 1998;13:263Y272 19. Gunne J, Astrand P, Lindh T, et al. Tooth implant supported fixed partial dentures: a ten year report. Int J Prosthodont 1999;12:216Y221 20. Tawil G, Younan R. Clinical evaluation of short, machined-surface implants followed for 12 to 92 months. Int J Oral Maxillofac Implants 2003;18:894Y901 21. Schulte J, Flores AM, Weed M. Crown-to-implant ratios of single tooth implant-supported restorations. J Prosthet Dent 2007;98:1Y5 22. Bahat O. Treatment planning and placement of dental implants in the posterior maxillae: report on 732 consecutive Nobelpharma implants. Int J Oral Maxillofac Implants 1993;8:151Y161 23. Snauwaert K, Duyck J, van Steenberghe D, et al. Time dependent failure rate and marginal bone loss of implant supported prosthesis: a 15 year follow-up study. Clin Oral Investig 2000;4:13Y20 24. Pierrisnard L, Renouard F, Renault P, et al. Influence of implant length and cortical anchorage on implant stress distribution. Clin Implant Dent Relat Res 2003;5:254Y262 25. Feldman S, Boitel N, Weng D, et al. Five-year survival distributions of short-length (10 mm or less) machined-surface and Osseostite implants. Clin Implant Dent Relat Res 2004;6:16Y23 26. Renouard F, Nisand D. Short implants in the severely resorbed maxilla: a 2-year retrospective clinical study. Clin Implant Dent Relat Res 2005;7:S104YS110 27. Rokni S, Todescan R, Watson P, et al. An assessment of crown-to-root 4 28. 29. 30. 31. 32. 33. 34. 35. 36. 37. 38. 39. 40. 41. 42. 43. 44. 45. & Volume 23, Number 3, May 2012 ratios with short sintered porous-surface implants supporting prosthesis in partially edentulous patient. Int J Oral Maxillofac Implants 2005;20:69Y76 Gentile MA, Chuang SK, Dodson TB. Survival estimates and risk factors for failure with 6 5.7 mm implants. Int J Oral Maxillofac Implants 2005;20:930Y937 Huang H-L, Hsu J-T, Fuh L-J, et al. Bone stress and interfacial sliding analysis of implant design on an immediately loaded maxillary implant: a non linear finite element study. J Dent 2008;36:409Y417 Tada S, Stegaroiu R, Kitamura E, et al. Influence of implant design and bone quality on stress/strain distribution in bone around implants: a 3-dimensional finite element analysis. Int J Oral Maxillofac Implants 2003;18:357Y368 Asmussen E, Peutzfeldt A, Sahafi A. Finite element analysis of stresses in endodontically treated, dowel-restored teeth. J Prosthet Dent 2005;94:321Y329 Sorrentino R, Aversa R, Ferro V, et al. Three-dimensional finite element analysis of strain and stress distributions in endodontically treated maxillary central incisors restored with different post, core and crown materials. Dental Mater 2007;23:983Y993 Baggi L, Cappelloni I, Girolamo M, et al. The influence of implant diameter and length on stress distribution of osseointegrated implants related to crestal bone geometry: a three-dimensional finite element analysis. J Prosthet Dent 2008;100:422Y431 Dejak B, Mlotkowski A. Three-dimensional finite element analysis of strength and adhesion of composite resin versus ceramic inlays in molars. J Prosthet Dent 2008;99:131Y140 Hsu J-T, Fuh L-J, Lin D-J, et al. Bone strain and interfacial sliding analysis of platform switching and implant diameter on an immediately loaded implant: experimental and three-dimensional finite element analysis. J Peridontol 2009;80:1125Y1132 Canullo L, Rasperini G. Preservation of peri-implant soft and hard tissues using platform switching of implants placed in immediate extraction sockets: a proof-of-concept study with 12-to-36-month follow-up. Int J Maxillofac Implants 2007;22:995Y1000 Prosper L, Redaelli S, Pasi M, et al. A randomized prospective multicenter trial evaluating the platform-switching technique for the prevention of postrestorative crestal bone loss. Int J Oral Maxillofac Implants 2009;24:299Y308 Calvo-Guirado JL, Ortiz-Ruiz AJ, López Marı́ L, et al. Immediate maxillary restoration of single-tooth implants using platform switching for crestal bone preservation: a 12-month study. Int J Oral Maxillofac Implants 2009;24:275Y281 Romanos GE, Nentwig G-H. Immediate functional loading in the maxilla using implants with platform switching: five-year results. Int J Maxillofac Implants 2009;24:1106Y1112 Crespi R, Capparè P, Gherlone E. Radiographic evaluation of bone levels around platform-switched and nonYplatform-switched implants used in an immediate loading protocol. Int J Oral Maxillofac Implants 2009;24:920Y926 Degidi M, Iezzi G, Scarano A, et al. Immediately loaded titanium implant with a tissue-stabilizing/maintaining design (‘beyond platform switch’) retrieved from man after 4 weeks: a histological and histomorphometrical evaluation. A case report. Clin Oral Implants Res 2009;19:276Y282 Chaushu G, Chaushu S, Tzohar A, et al. Immediate loading of single-tooth implants: immediate versus non-immediate implantation. A clinical report. Int J Oral Maxillofac Implants 2001;16:267Y272 Maló P, Rangert B, Dvarsater L. Immediate function of Brånemark implants in the esthetic zone: a retrospective clinical study with 6 months to 4 years of follow-up. Clin Imp Dent Relat Res 2000;2:138Y146 Otate S, Lyrio MCN, Moraes M, et al. Influence of diameter and length of implant on early dental implant failure. J Oral Maxillofac Surg 2010;68:414Y419 Spiekermann H, Jansen VK, Richter EJ. A 10-year follow-up study of IMZ and TPS implants in the edentulous mandible using bar-retained overdentures. Int J Oral Maxillofac Implants 1995;10:231Y243 * 2012 Mutaz B. Habal, MD Copyright © 2012 Mutaz B. Habal, MD. Unauthorized reproduction of this article is prohibited.
Download