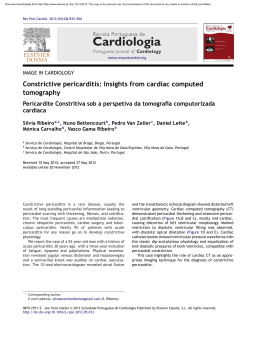
www.arquivosonline.com.br Sociedade Brasileira de Cardiologia • ISSN-0066-782X • Volume 104, Nº 6, June 2015 50.0% 45.0% 40.0% 35.0% 30.0% 30.3% 25.0% 20.4% 20.0% 14.6% 15.0% 10.8% 10.0% 12.4% 5.0% 0.0% Ischemic DCM* Hypertensive Chagas Valvular 10.3% 0.4% 0.8% QT† Myocarditis Others Figure 1 – Distribution of etiologies of heart failure in the BREATHE registry. * DCM: dilated cardiomyopathy; † QT: secondary to chemotherapy. page 436 Editorial Heart Rate Variability Correlates to Functional Aerobic Impairment in Distance Psychotherapy – New Reality Hemodialysis Patients Original Articles Review Article I Brazilian Registry of Heart Failure - Clinical Aspects, Care Quality Reverse Cardiac Remodeling: A Marker of Better Prognosis in and Hospitalization Outcomes Heart Failure Depression as a Clinical Determinant of Dependence and Low Quality Letter to the Editor of Life in Elderly Patients with Cardiovascular Disease An Issue Waiting to be Clarified: Effects of the QT Prolonging Drugs on Assessment of Autonomic Function by Phase Rectification of RR- Tp-e Interval Interval Histogram Analysis in Chagas Disease Post-Acute Coronary Syndrome Alcohol Abuse: Prospective Evaluation Eletronic Pages in the ERICO Study APOE and LDLR Gene Polymorphisms and Dyslipidemia Tracking. Rio de Janeiro Study Circulatory and Ventilatory Power: Characterization in Patients with Coronary Artery Disease Clinicoradiological Session Case 5/2015 – Late Outcome of Corrected Aortopulmonary Window in A 23-Year-Old Female Patient Who Underwent Surgery in Childhood Case Report Blood Pressure and Hemodynamic Adaptations after a Training Acute Myocardial Infarction and Severe Prosthetic Dysfunction after Program in Young Individuals with Down Syndrome Bentall Procedure A JOURNAL OF SOCIEDADE BRASILEIRA DE CARDIOLOGIA - Published since 1948 Contents Editorial Distance Psychotherapy – New Reality Protásio L. da Luz, Mayra L. Gagliani, Bellkiss W. Romano .....................................................................................................................................................................page 431 Original Articles Heart Failure I Brazilian Registry of Heart Failure - Clinical Aspects, Care Quality and Hospitalization Outcomes Denilson Campos de Albuquerque, João David de Souza Neto, Fernando Bacal, Luiz Eduardo Paim Rohde, Sabrina Bernardez-Pereira, Otavio Berwanger, Dirceu Rodrigues Almeida, Investigadores Estudo BREATHE .....................................................................................................................................................................page 433 Cardiogeriatrics Depression as a Clinical Determinant of Dependence and Low Quality of Life in Elderly Patients with Cardiovascular Disease Giselle Helena de Paula Rodrigues, Otavio Celso Eluf Gebara, Catia Cilene da Silva Gerbi, Humberto Pierri, Mauricio Wajngarten .....................................................................................................................................................................page 443 Chagas Disease Assessment of Autonomic Function by Phase Rectification of RR-Interval Histogram Analysis in Chagas Disease Olivassé Nasario-Junior, Paulo Roberto Benchimol-Barbosa, Roberto Coury Pedrosa, Jurandir Nadal .....................................................................................................................................................................page 450 Epidemiology Post-Acute Coronary Syndrome Alcohol Abuse: Prospective Evaluation in the ERICO Study Abner Morilha, Samuel Karagulian, Paulo A. Lotufo, Itamar S. Santos, Isabela M. Benseñor, Alessandra C. Goulart .....................................................................................................................................................................page 457 APOE and LDLR Gene Polymorphisms and Dyslipidemia Tracking. Rio de Janeiro Study Rossana Ghessa Andrade de Freitas, Erika Maria Gonçalves Campana, Roberto Pozzan, Andréa Araujo Brandão, Ayrton Pires Brandão, Maria Eliane Campos Magalhães, Dayse Aparecida da Silva .....................................................................................................................................................................page 468 Ergospirometry Circulatory and Ventilatory Power: Characterization in Patients with Coronary Artery Disease Viviane Castello-Simões, Vinicius Minatel, Marlus Karsten, Rodrigo Polaquini Simões, Natália Maria Perseguini, Juliana Cristina Milan, Ross Arena, Laura Maria Tomazi Neves, Audrey Borghi-Silva, Aparecida Maria Catai .....................................................................................................................................................................page 476 Arquivos Brasileiros de Cardiologia - Volume 104, Nº 6, June 2015 Exercising Blood Pressure and Hemodynamic Adaptations after a Training Program in Young Individuals with Down Syndrome Bruna Barboza Seron, Karla Fabiana Goessler, Everaldo Lambert Modesto, Eloise Werle Almeida, Márcia Greguol .....................................................................................................................................................................page 487 Other Diagnostic Tests (not involving imaging) Heart Rate Variability Correlates to Functional Aerobic Impairment in Hemodialysis Patients Maria Angela Magalhães de Queiroz Carreira, André Barros Nogueira, Felipe Montes Pena, Marcio Galindo Kiuchi, Ronaldo Campos Rodrigues, Rodrigo da Rocha Rodrigues, Jorge Paulo Strogoff de Matos, Jocemir Ronaldo Lugon .....................................................................................................................................................................page 493 Review Article Reverse Cardiac Remodeling: A Marker of Better Prognosis in Heart Failure José Rosino de Araújo Rocha Reis Filho, Juliano Novaes Cardoso, Cristina Martins dos Reis Cardoso, Antonio Carlos Pereira-Barretto .....................................................................................................................................................................page 502 Letter to the Editor An Issue Waiting to be Clarified: Effects of the QT Prolonging Drugs on Tp-e Interval Omer Yiginer, Mehmet Dogan, Emrah Erdal .....................................................................................................................................................................page 507 Arquivos Brasileiros de Cardiologia - Volume 104, Nº 6, June 2015 Arquivos Brasileiros de Cardiologia - Eletronic Pages Clinicoradiological Session Case 5/2015 – Late Outcome of Corrected Aortopulmonary Window in A 23-Year-Old Female Patient Who Underwent Surgery in Childhood Edmar Atik .................................................................................................................................................................. page e55 Case Report Acute Myocardial Infarction and Severe Prosthetic Dysfunction after Bentall Procedure Viviane Tiemi Hotta, Pedro Gabriel de Melo Barros, Paulo Sampaio Gutierrez, Angela Cristina Pasiani Bolonhez, Wilson Mathias, Ricardo Ribeiro Dias .................................................................................................................................................................. page e58 * Indicate manuscripts only in the electronic version. To view them, visit: http://www.arquivosonline.com.br/2015/english/10406/edicaoatual.asp Arquivos Brasileiros de Cardiologia - Volume 104, Nº 6, June 2015 www.arquivosonline.com.br A JOURNAL OF SOCIEDADE BRASILEIRA DE CARDIOLOGIA - Published since 1948 Scientific Director Maria da Consolação Vieira Moreira Interventionist Cardiology Pedro A. Lemos Chief Editor Luiz Felipe P. Moreira Pediatric/Congenital Cardiology Antonio Augusto Lopes Associated Editors Arrhythmias/Pacemaker Mauricio Scanavacca Clinical Cardiology José Augusto Barreto-Filho Non-Invasive Diagnostic Methods Carlos E. Rochitte Surgical Cardiology Paulo Roberto B. Evora Basic or Experimental Research Leonardo A. M. Zornoff Epidemiology/Statistics Lucia Campos Pellanda Arterial Hypertension Paulo Cesar B. V. Jardim Ergometrics, Exercise and Cardiac Rehabilitation Ricardo Stein First Editor (1948-1953) † Jairo Ramos Editorial Board Brazil Aguinaldo Figueiredo de Freitas Junior (GO) Alfredo José Mansur (SP) Aloir Queiroz de Araújo Sobrinho (ES) Amanda G. M. R. Sousa (SP) Ana Clara Tude Rodrigues (SP) André Labrunie (PR) Andrei Sposito (SP) Angelo A. V. de Paola (SP) Antonio Augusto Barbosa Lopes (SP) Antonio Carlos C. Carvalho (SP) Antônio Carlos Palandri Chagas (SP) Antonio Carlos Pereira Barretto (SP) Antonio Cláudio L. Nóbrega (RJ) Antonio de Padua Mansur (SP) Ari Timerman (SP) Armênio Costa Guimarães (BA) Ayrton Pires Brandão (RJ) Beatriz Matsubara (SP) Brivaldo Markman Filho (PE) Bruno Caramelli (SP) Carisi A. Polanczyk (RS) Carlos Eduardo Rochitte (SP) Carlos Eduardo Suaide Silva (SP) Carlos Vicente Serrano Júnior (SP) Celso Amodeo (SP) Charles Mady (SP) Claudio Gil Soares de Araujo (RJ) Cláudio Tinoco Mesquita (RJ) Cleonice Carvalho C. Mota (MG) Clerio Francisco de Azevedo Filho (RJ) Dalton Bertolim Précoma (PR) Dário C. Sobral Filho (PE) Décio Mion Junior (SP) Denilson Campos de Albuquerque (RJ) Djair Brindeiro Filho (PE) Domingo M. Braile (SP) Edmar Atik (SP) Emilio Hideyuki Moriguchi (RS) Enio Buffolo (SP) Eulógio E. Martinez Filho (SP) Evandro Tinoco Mesquita (RJ) Expedito E. Ribeiro da Silva (SP) Fábio Vilas-Boas (BA) Fernando Bacal (SP) Flávio D. Fuchs (RS) Francisco Antonio Helfenstein Fonseca (SP) Gilson Soares Feitosa (BA) Glaucia Maria M. de Oliveira (RJ) Hans Fernando R. Dohmann (RJ) Humberto Villacorta Junior (RJ) Ínes Lessa (BA) Iran Castro (RS) Jarbas Jakson Dinkhuysen (SP) João Pimenta (SP) Jorge Ilha Guimarães (RS) José Antonio Franchini Ramires (SP) José Augusto Soares Barreto Filho (SE) José Carlos Nicolau (SP) José Lázaro de Andrade (SP) José Péricles Esteves (BA) Leonardo A. M. Zornoff (SP) Leopoldo Soares Piegas (SP) Lucia Campos Pellanda (RS) Luís Eduardo Rohde (RS) Luís Cláudio Lemos Correia (BA) Luiz A. Machado César (SP) Luiz Alberto Piva e Mattos (SP) Marcia Melo Barbosa (MG) Maria da Consolação Moreira (MG) Mario S. S. de Azeredo Coutinho (SC) Maurício I. Scanavacca (SP) Max Grinberg (SP) Michel Batlouni (SP) Murilo Foppa (RS) Nadine O. Clausell (RS) Orlando Campos Filho (SP) Otávio Rizzi Coelho (SP) Otoni Moreira Gomes (MG) Paulo Andrade Lotufo (SP) Paulo Cesar B. V. Jardim (GO) Paulo J. F. Tucci (SP) Paulo R. A. Caramori (RS) Paulo Roberto B. Évora (SP) Paulo Roberto S. Brofman (PR) Pedro A. Lemos (SP) Protásio Lemos da Luz (SP) Reinaldo B. Bestetti (SP) Renato A. K. Kalil (RS) Ricardo Stein (RS) Salvador Rassi (GO) Sandra da Silva Mattos (PE) Sandra Fuchs (RS) Sergio Timerman (SP) Silvio Henrique Barberato (PR) Tales de Carvalho (SC) Vera D. Aiello (SP) Walter José Gomes (SP) Weimar K. S. B. de Souza (GO) William Azem Chalela (SP) Wilson Mathias Junior (SP) Exterior Adelino F. Leite-Moreira (Portugal) Alan Maisel (USA) Aldo P. Maggioni (Italy) Cândida Fonseca (Portugal) Fausto Pinto (Portugal) Hugo Grancelli (Argentina) James de Lemos (USA) João A. Lima (USA) John G. F. Cleland (England) Maria Pilar Tornos (Spain) Pedro Brugada (Belgium) Peter A. McCullough (USA) Peter Libby (USA) Piero Anversa (Italy) Sociedade Brasileira de Cardiologia President Angelo Amato V. de Paola Special Advisor to the Presidency Fábio Sândoli de Brito SBC/MG - Odilon Gariglio Alvarenga de Freitas Vice-President Sergio Tavares Montenegro Adjunct Coordination SBC/MS - Mércule Pedro Paulista Cavalcante SBC Newsletter Editor Nabil Ghorayeb e Fernando Antonio Lucchese SBC/MT - Julio César De Oliveira Continuing Education Coordination Estêvão Lanna Figueiredo SBC/NNE - Jose Itamar Abreu Costa President-Elect Marcus Vinícius Bolívar Malachias Financial Director Jacob Atié Scientific Director Maria da Consolação Vieira Moreira Administrative Director Emilio Cesar Zilli Assistance Quality Director Pedro Ferreira de Albuquerque Communication Director Maurício Batista Nunes Norms and Guidelines Coordination Luiz Carlos Bodanese Governmental Integration Coordination Edna Maria Marques de Oliveira Regional Integration Coordination José Luis Aziz Presidents of State and Regional Brazilian Societies of Cardiology SBC/AL - Carlos Alberto Ramos Macias Information Technology Director José Carlos Moura Jorge SBC/AM - Simão Gonçalves Maduro Government Liaison Director Luiz César Nazário Scala SBC/BA - Mario de Seixas Rocha Director of State and Regional Affairs Abrahão Afiune Neto SBC/CE - Ana Lucia de Sá Leitão Ramos Cardiovascular Health Promotion Director - SBC/Funcor Carlos Costa Magalhães Department Director Especializados - Jorge Eduardo Assef Research Director Fernanda Marciano Consolim Colombo Chief Editor of the Brazilian Archives of Cardiology Luiz Felipe P. Moreira SBC/CO - Frederico Somaio Neto SBC/PA - Luiz Alberto Rolla Maneschy SBC/PB - Helman Campos Martins SBC/PE - Catarina Vasconcelos Cavalcanti SBC/PI - João Francisco de Sousa SBC/PR - Osni Moreira Filho SBC/RJ - Olga Ferreira de Souza SBC/RN - Rui Alberto de Faria Filho SBC/RS - Carisi Anne Polanczyk SBC/DF - Wagner Pires de Oliveira Junior SBC/SC - Marcos Venício Garcia Joaquim SBC/ES - Marcio Augusto Silva SBC/SE - Fabio Serra Silveira SBC/GO - Thiago de Souza Veiga Jardim SBC/SP - Francisco Antonio Helfenstein Fonseca SBC/MA - Nilton Santana de Oliveira SBC/TO - Hueverson Junqueira Neves Presidents of the Specialized Departaments and Study Groups SBC/DA - José Rocha Faria Neto SBCCV - Marcelo Matos Cascado GECC - Mauricio Wanjgarten SBC/DECAGE - Josmar de Castro Alves SBHCI - Helio Roque Figueira GEPREC - Glaucia Maria Moraes de Oliveira SBC/DCC - José Carlos Nicolau SBC/DEIC - Dirceu Rodrigues Almeida SBC/DCM - Maria Alayde Mendonça da Silva Grupo de Estudos de Cardiologia Hospitalar Evandro Tinoco Mesquita GERTC - Clerio Francisco de Azevedo Filho SBC/DCC/CP - Isabel Cristina Britto Guimarães SBC/DIC - Arnaldo Rabischoffsky SBC/DERC - Nabil Ghorayeb GAPO - Danielle Menosi Gualandro GEECG - Joel Alves Pinho Filho Grupo de Estudos de Cardio-Oncologia Roberto Kalil Filho GEEC - Cláudio José Fuganti GECIP - Gisela Martina Bohns Meyer SBC/DFCVR - Ricardo Adala Benfati GEECABE - Mario Sergio S. de Azeredo Coutinho SBC/DHA - Luiz Aparecido Bortolotto GECETI - Gilson Soares Feitosa Filho GECN - Ronaldo de Souza Leão Lima SOBRAC - Luiz Pereira de Magalhães GEMCA - Alvaro Avezum Junior GERCPM - Artur Haddad Herdy GECESP - Ricardo Stein Arquivos Brasileiros de Cardiologia Volume 104, Nº 6, June 2015 Indexing: ISI (Thomson Scientific), Cumulated Index Medicus (NLM), SCOPUS, MEDLINE, EMBASE, LILACS, SciELO, PubMed Address: Av. Marechal Câmara, 160 - 3º andar - Sala 330 20020-907 • Centro • Rio de Janeiro, RJ • Brasil Phone.: (21) 3478-2700 E-mail: [email protected] www.arquivosonline.com.br SciELO: www.scielo.br Commercial Department Phone: (11) 3411-5500 Graphic Design and Diagramming SBC - Internal Design Department E-mail: [email protected] Print IMOS Editora e Gráfica Editorial Production Circulation 1.500 copies SBC - Internal Publication Department Affiliated at the Brazilian Medical Association The ads showed in this issue are of the sole responsibility of advertisers, as well as the concepts expressed in signed articles are of the sole responsibility of their authors and do not necessarily reflect the views of SBC. This material is for exclusive distribution to the medical profession. The Brazilian Archives of Cardiology are not responsible for unauthorized access to its contents and that is not in agreement with the determination in compliance with the Collegiate Board Resolution (DRC) N. 96/08 of the National Sanitary Surveillance Agency (ANVISA), which updates the technical regulation on Drug Publicity, Advertising, Promotion and Information. According to Article 27 of the insignia, "the advertisement or publicity of prescription drugs should be restricted solely and exclusively to health professionals qualified to prescribe or dispense such products (...)". To ensure universal access, the scientific content of the journal is still available for full and free access to all interested parties at: www.arquivosonline.com.br. SUPPORT Back to the Cover Editorial Distance Psychotherapy – New Reality Protásio L. da Luz, Mayra L. Gagliani, Bellkiss W. Romano Instituto do Coração do HC – FMUSP, São Paulo, SP – Brazil High technology progresses fast in the medical area. The most recent advance is the “big data” study, in which multiple technologies are applied to populations in order to incorporate genetic data, biological markers and imaging, to assess risks and predict the occurrence of clinical phenomena. That is a global, multidisciplinary and multinational view, which supports and helps the implementation of preventive actions. Psychology practice in Brazil, however, still resists to this modernity. Face-to-face psychotherapy is the only modality of treatment accepted by the Brazilian Federal Council of Psychology. However, distance counseling, via Internet or mobile phone, has been increasingly used in the USA, Europe and Oceania. Epstein et al. 1 have reported the increasing use of “e-therapy”, as well as the exponential growth of related publications. In New Zealand, Gibson et al.2 have reported the experience of adolescents with mobile phone therapy. Eight aspects were identified by adolescents as advantageous: privacy, autonomy, control, anonymity, easy access, personalization, individualization of language, and connection. The importance of these new methodologies relates to the prevalence and incidence of emotional problems worldwide. For example, depression will be the most common non-fatal disease of the 21st century3, and an important cause of work disability and loss of quality of life, in addition to being the third cause of suicide among North-American young adults. An extensive review published in the Journal of the American College of Cardiology by Rozansky4 in 2014 showed that a number of factors, such as sleep disorders, anxiety, several forms of stress at home and in the workplace, lack of purpose in life, anger and inability to face challenges, are significantly associated with cardiovascular diseases, as well as with cardiac and all-cause mortality. Those associations depend on unhealthy life habits, such as sedentary lifestyle and smoking, and activation of the sympathetic nervous system, which trigger pathophysiological mechanisms that cause cardiovascular diseases5. Thus, there is a biologically plausible mechanistic connection of emotional and behavioral problems with organic Keywords Psychotherapy; Social Networking; Internet / utilization; Internet / trends; Computer Communication Networks. Mailing Adrress: Protásio Lemos da Luz • Incor - FMUSP - Avenida Dr. Enéas de Carvalho Aguiar, n° 44, 5 andar BlocoII - sala 08. Postal Code 05403-000, São Paulo, SP - Brazil E-mail: [email protected] Manuscript received April 29, 2015; revised manuscript May 06, 2015; accepted May 06, 2015. DOI: 10.5935/abc.20150067 431 cardiovascular disease. If, on the one hand, the understanding of the pathophysiological mechanisms belongs to the cellular and molecular biology domains, on the other, when attempting to change behaviors, physicians need the professional help of psychologists. In addition, prevention is precisely one of the pillars in the eradication of chronic non-communicable diseases, such as atherosclerosis, diabetes and hypertension, which are the major causes of mortality causes in the modern world. The fundamental requirements in the preventive strategy are changes in lifestyle, such as smoking cessation, exercise practice and the adoption of healthy diets. This is the point where the two sciences meet. Moreover, physicians often fail to recognize emotional problems, both the primary ones and those associated with organic diseases. Several psychological treatments are misused, and the number of cases treated is insufficient, barely reaching 50%3. On the other hand, the economic burden of depression and dementia is astronomical 6,7. In the USA, the cost of depression, mainly related to absenteeism and poor work performance, has reached U$53 billion in one year. Regarding dementia, Hurd et al.7 have estimated individual costs between U$42,000 and 56,000/person/year, and between U$ 157 billion and 250 billion/year in the USA. In Brazil, such costs are unknown, but most likely high as well. Given that scenario, the following measures are imperative: a.to identify psychological factors, as well as primary conditions, in organic diseases; b. to adopt global health care, which are patient and not only disease oriented; c. to incorporate different methodologies of treatment, such as new drugs and new behavioral treatment forms; d. to improve the treatment of mental illness. Concerning “distance psychotherapy”, we believe that the brazilian law needs to be changed and adapted to the new times. Not disregarding the classic face-to-face therapy, distance counseling should not only be allowed, but encouraged in special situations covered by appropriate legislation. In Brazil, distance psychotherapy is currently allowed in the research only and encourages debate on efficiency and safety, privacy, ethical and legal questions, and other aspects8. For example, one therapeutic process could begin with a few initial interviews, followed by distance treatment and face-toface interviews at intervals. This would benefit patients living far away from large centers, where modern therapeutic techniques, such as cognitive behavioral therapy, are not available. Such alternatives would certainly contribute to the preventive processes so heartedly championed by modern medicine. Both psychologists and their formal representatives should pursue this inevitable update. Luz et al. Distance psychotherapy – New reality Editorial References 1. Epstein R. Distance therapy comes of age. Scientific American Mind May/June 2011. [Cited in 2015 Jan 10]. Available from: http://www. scientificamerican.com/mind 5. 2. Gibson K, Cartwright C. Young people´s experiences of mobile phone text counselling: Balancing connection and control. Children and youth services review. 2014;43:96-104. 6. Wang PS, Simon G, Kessler RC. The economic burden of depression and the cost-effectiveness of treatment. Int J Methods Psychiatr Res. 2003;12(1):22-33. 3. The National Alliance on Mentall Illness, 2013. [Cited in 2015 Jan 10]. Available from: http://www.nami.org 7. Hurd MD, Martorell P, Delavande A, Mullen KJ, Langa KM. Monetary costs of dementia in the United States. N Engl J Med. 2013;368(14):1326-34. 4. 8. Rozanski A. Behavioral cardiology: current advances and future directions. J Am Coll Cardiol. 2014;64 (1):100-10. Luz PL, Nishiyama M, Chagas AC. Drugs and lifestyle for the treatment and prevention of coronary artery disease: comparative analysis of the scientific basis. Braz J Med Biol Res. 2011;44(10):973-91. Pieta MA, Gomes WB. Psicoterapia pela internet: viável ou inviável? Psicol cienc prof. 2014;34(1):18-31. Arq Bras Cardiol. 2015; 104(6):431-432 432 Back to the Cover Original Article I Brazilian Registry of Heart Failure - Clinical Aspects, Care Quality and Hospitalization Outcomes Denilson Campos de Albuquerque1, João David de Souza Neto2, Fernando Bacal3, Luiz Eduardo Paim Rohde4, Sabrina Bernardez-Pereira5, Otavio Berwanger5, Dirceu Rodrigues Almeida6, Investigadores Estudo BREATHE Universidade do Estado do Rio de Janeiro (UERJ)1, Rio de Janeiro, RJ; Hospital de Messejana2, Fortaleza, CE; Instituto do Coração (InCor) do Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo3, São Paulo, SP; Hospital de Clínicas de Porto Alegre4, Porto Alegre, RS; Instituto de Pesquisa, Hospital do Coração5, São Paulo, SP; Universidade Federal de São Paulo, UNIFESP6, São Paulo, SP; Sociedade Brasileira de Cardiologia - Departamento de Insuficiência Cardíaca (DEIC) - Brazil Abstract Background: Heart failure (HF) is one of the leading causes of hospitalization in adults in Brazil. However, most of the available data is limited to unicenter registries. The BREATHE registry is the first to include a large sample of hospitalized patients with decompensated HF from different regions in Brazil. Objective: Describe the clinical characteristics, treatment and prognosis of hospitalized patients admitted with acute HF. Methods: Observational registry study with longitudinal follow-up. The eligibility criteria included patients older than 18 years with a definitive diagnosis of HF, admitted to public or private hospitals. Assessed outcomes included the causes of decompensation, use of medications, care quality indicators, hemodynamic profile and intrahospital events. Results: A total of 1,263 patients (64 ± 16 years, 60% women) were included from 51 centers from different regions in Brazil. The most common comorbidities were hypertension (70.8%), dyslipidemia (36.7%) and diabetes (34%). Around 40% of the patients had normal left ventricular systolic function and most were admitted with a wet-warm clinical-hemodynamic profile. Vasodilators and intravenous inotropes were used in less than 15% of the studied cohort. Care quality indicators based on hospital discharge recommendations were reached in less than 65% of the patients. Intrahospital mortality affected 12.6% of all patients included. Conclusion: The BREATHE study demonstrated the high intrahospital mortality of patients admitted with acute HF in Brazil, in addition to the low rate of prescription of drugs based on evidence. (Arq Bras Cardiol. 2015; 104(6):433-442) Keywords: Heart Failure/mortality; Epidemiology; Hospitalization; Inappropriate Prescribing. Introduction Heart failure (HF) has been pointed to as an important public health problem and regarded as a new epidemic with high mortality and morbidity, in spite of the advances in current therapeutics. Updated data from the American Heart Association (AHA) estimated a prevalence of 5.1 million individuals with HF in the United States alone between 2007 and 2012. Projections show that the prevalence of HF will increase 46% between 2012 and 2030, resulting in more than 8 million individuals above the age of 18 years with HF1. The rising prevalence is probably due to the increase in life expectancy, since HF affects predominantly older age groups2. HF is the leading cause of hospitalization, based on data available from about 50% of the population in South America3. The most comprehensive portrait of the situation Mailing Address: Denilson Campos de Albuquerque • Rua Voluntários da Pátria 445, 1402. Postal Code 22270000, Rio de Janeiro, RJ – Brazil E-mail: [email protected] Manuscript received November 10, 2014; revised manuscript January 7, 2015; accepted January 7, 2015. DOI: 10.5935/abc.20150031 433 of hospitalizations for HF in Brazil can be obtained through analyses of DATA-SUS records, with the inherent limitations of a database of an administrative nature. Data show that in 2012 alone there were 26,694 deaths in Brazil due to HF. Of 1,137,572 admissions due to circulatory diseases in that same year, around 21% were due to HF4. The burden becomes even more significant when we consider that almost 50% of all hospitalized patients with this diagnosis are readmitted within 90 days after hospital discharge, and that hospital readmission is one of the main risk factors for death in this syndrome5,6. Several studies have focused on identifying the factors associated with frequent readmissions7,8. Those usually described in the international literature are inadequate therapy, lack of adherence to treatment, social isolation, or worsening cardiac function. However, in approximately 30-40% of the cases it is not possible to identify the cause of clinical decompensation9. Data on morbidity and consequent costs associated with decompensated HF are undeniable all over the world. In Brazil, there are only a few studies comprehensively and prospectively assessing the demographic, clinical and prognostic characteristics of patients who are admitted with a clinical diagnosis of HF. Isolated initiatives suggest the existence of significant regional differences in several characteristics of patients who are admitted Albuquerque et al. BREATHE: Characteristics, Indicators and Outcomes Original Article with HF in Brazil, but these comparisons are methodologically limited by often divergent guidelines and inclusion criteria10-12. Thus, the establishment of a national registry which incorporates a group of public and private hospitals from different Brazilian regions can portray more accurately which patients are admitted with a diagnosis of HF, how these patients are treated in their institutions and what are their short- and long-term prognoses. The BREATHE study is the first national and multicenter registry of acute HF that includes all regions of the country, involving 51 public and private hospitals in 21 cities in Brazil. The aim of this analysis is to describe the clinical features, treatment and prognosis of hospitalized patients admitted with acute HF in Brazil. Methods Delineation Cross-sectional, observational study (registry) with longitudinal follow-up. Hospital Selection The public and private hospitals that participated in the Registry of Decompensated Heart Failure of the Department of Heart Failure of the Brazilian Society of Cardiology were chosen by the research committee. A fixed number of institutions was allocated for each one of the five regions of the country, and the number of patients per region was defined based on the absolute number of hospitalizations by region in the year 2004 according to the IBGE (Supplement II). Inclusion and Exclusion Criteria The methods of BREATHE, as well as its inclusion and exclusion criteria, have been previously described13. Patients older than 18 years, admitted to public or private hospitals with a definitive clinical profile of HF confirmed by the Boston criteria were considered eligible for the study14. Those patients undergoing myocardial revascularization procedures (coronary angioplasty or surgery) in the last month of the selection and who presented signs of HF secondary to sepsis were excluded from the study. Definitions of the Study: a) Clinical and Hemodynamic Profile: The clinical and hemodynamic profile was defined according to the classification of Stevenson15, in four hemodynamic profiles according to the findings on physical examination of pulmonary congestion and peripheral perfusion. Patients with acute HF are generally in one of the following subgroups: 1) presence of pulmonary congestion without signs of hypoperfusion (wet and warm); 2) presence of pulmonary congestion associated with hypoperfusion (wet and cold); and 3) hypoperfusion without pulmonary congestion (dry and cold). b) HF Treatment Targets Doses: Target doses for the treatment of acute HF, for purposes of evaluation of the data from this study, were the same as those recommended by the II Guideline of Acute Heart Failure of the Brazilian Society of Cardiology16. c) Causes of HF Decompensation: The main causes of decompensation analyzed included infection, decompensation from acute valvular disease, poor adherence to drug therapy, excessive sodium intake in the last week, arrhythmias and pulmonary embolism. The classification was determined by the clinical judgment of the local investigator according to the patient’s report. Follow-up For the present analysis, in addition to hospital admission data, data were collected during hospitalization until the date of medical discharge or intrahospital death. Outcomes of Interest The primary outcome of this study was the all-cause intrahospital mortality. Secondary outcomes included the proportion of patients who received interventions with proven benefit demonstrated by care quality indicators (use of angiotensin converting enzyme inhibitors [ACEi] / angiotensin II receptor blockers [ARB] and use of beta‑blockers), readmissions due to HF and cardiovascular mortality. Ethical Aspects The protocol was approved by the Research Ethics Committee (Comitê de Ética em Pesquisa, CEP) of the Hospital do Coração de São Paulo, SP (HCor) on February 1st, 2011, under the registration number 144/2011, and following that, each participating center also had their protocols approved by their own CEPs. All patients signed a Free and Informed Consent Form and the clinical study was conducted in accordance with the principles of the current revision of the Declaration of Helsinki. Data Management The management of the data was performed using the EDC (Electronic Data Capture) system. Medical charts were transcribed by Web-charts, sent to the central coordinating center, and incorporated into a database for validation. Quality control of the data of the study occurred mainly by central checking in search of possible inconsistencies (data without biological plausibility) or incomplete data, and was reported to the participating centers for confirmation and/or correction. The Department of Heart Failure of the Brazilian Society of Cardiology was responsible for the management of the data of the study. Sample Size The first phase of the Brazilian Registry of Decompensated HF predicted the evaluation of 1,200 admissions to the public and private network in different regions of Brazil. This sample size was determined to represent the largest Brazilian prospective study of decompensated HF, involving all regions of the country, allowing identification of regional differences in intrahospital mortality. Arq Bras Cardiol. 2015; 104(6):433-442 434 Albuquerque et al. BREATHE: Characteristics, Indicators and Outcomes Original Article Statistical Analysis Continuous variables were described as medians (interquartile range) or means (standard deviation) according to the distribution of the variable, and the categorical variables as absolute and relative frequencies. Normality was evaluated with the visual inspection of histograms and application of the Shapiro-Wilks test of normality. Age distribution was compared among regions according to a model of analysis of variance (ANOVA) and the relationship between etiology and region was determined by the chi-square test. The software SAS 9.3 (Statistical Analysis System, Cary, NC) was used for statistical analysis of the data17. Results Between February 2011 and December 2012, 1,263 patients were included in 51 centers from different Brazilian regions (2 centers in the Northern region [164 patients], 13 centers in the Northeast [209 patients], 5 centers in the Midwest [66 patients], 33 centers in the Southeast [652 patients] and 5 centers in the South [172 patients]). Two patients were excluded from the analysis for meeting exclusion criteria. The flow diagram can be found in Supplement II. The average age of the patients was 64 ± 16 years, with 73.1% above the age of 75 years and 60% women. Most patients were self-reportedly white (59%), admitted to the public network/Unified Health System (Sistema Único de Saúde, SUS; 64.8%) and from the South/Southeast regions (65.2%). Slightly over half of the patients included had left ventricular systolic dysfunction (58.7%), and the vast majority (70.8%) was hypertensive. Table 1 shows the baseline characteristics of the studied sample, including demographics and prior medical history. The average age distribution by region showed a statistically significant difference with the inclusion of patients of more advanced age in the Southeastern and Southern regions and younger patients in the Northern region (66 ± 15 years versus 59 ± 17 years, p = 0.019). Table 4 lists the main procedures performed during hospitalization, as well as the mortality rate during hospitalization. The sum of the deaths in the first 24 hours (17 patients) and after this period (140 patients) totaled 12.6% of the studied cohort. Valve replacement prevailed among the procedures during hospitalization, occurring in 156 patients. For the treatment of acute HF during hospitalization the use of loop diuretics prevailed (89.8%), followed by beta‑blockers (57.1%). The use of intravenous vasodilators (6.6%) and inotropic agents (13.6%) represented a small portion of the therapy in this population (Figure 3). According to the indicators of the Joint Commission on Accreditation of Healthcare Organizations (JCAHO), 63.7% of the patients received guidelines on hospital discharge about the correct use of medications, whereas only 34.9% and 16.2% were advised about the diet to be followed at home and prescription of physical activity, respectively (Figure 4). Discussion The main findings of this analysis of the study BREATHE are: 1) baseline characteristics show a populational profile of predominantly elderly patients, mainly in the Southern and Southeastern regions of Brazil; 2) poor drug adherence was the factor most frequently associated with Table 1 – Baseline characteristics of the cohort Variables BREATHE (n = 1,261) Age (mean+/-SD*) 64.1 ± 15.9 Male gender (%) 40.0 Prior acute myocardial infarction (%) 26.6 Hypertension (%) 70.8 The hypertensive and ischemic etiologies prevailed in the studied population, affecting 30.1% and 20.3% of the patients, respectively. Around 11% of the patients had a diagnosis of Chagas disease (Figure 1). Dyslipidemia (%) 36.7 Prior stroke /TIA§ (%)† 12.6 Atrial fibrillation (%) 27.3 In the analysis of the etiologies by region, patients from the South, Southeast and Northeast showed a predominance of the ischemic etiology (33.6%, 32.6%, and 31.9%, respectively). In patients in the Northern region the hypertensive etiology (37.2%) predominated, while among patients in the Northern region the Chagasic etiology predominated (42.4%) (Table 2). Depression (%)† The main causes of HF decompensation were poor adherence to medication (30%), followed by infections (23%) and inadequate control of water and sodium intake (9%), as shown in Table 3. Sodium (mean+/-SD) As for the clinical and hemodynamic profile on hospital admission, the prevalence was for the wet-warm profile, totaling 67.4% of the cases, whereas the wet-cold 435 and dry‑cold profiles accounted for 17.8% and 5.2%, respectively (Figure 2). Arq Bras Cardiol. 2015; 104(6):433-442 13.5 Occlusive peripheral arterial disease (%) † 10.8 Chronic renal failure (%)† 24.1 Diabetes mellitus (%) † 34.0 Chronic obstructive pulmonary disease (%) 12.7 Left ventricular ejection fraction (average/-+/-SD) Creatinine (mean+/-SD) BNP (median (IQR¶)) 38.8 ± 16.5 137 ± 16 1.7 ± 4.8 1,075 (518; 1,890) * SD: standard deviation; †Values calculated on a total of 1,255 patients with complete information; §TIA: transient ischemic attack; BNP: brain natriuretic peptide; ¶IQR: interquartile range. Back to the Cover Albuquerque et al. BREATHE: Characteristics, Indicators and Outcomes Original Article 50.0% 45.0% 40.0% 35.0% 30.0% 30.3% 25.0% 20.4% 20.0% 14.6% 15.0% 12.4% 10.8% 10.0% 10.3% 5.0% 0.0% Ischemic DCM* Hypertensive 0.4% 0.8% QT† Myocarditis Valvular Chagas Others Figure 1 – Distribution of etiologies of heart failure in the BREATHE registry. * DCM: dilated cardiomyopathy; † QT: secondary to chemotherapy. Table 2 – Distribution of etiologies according to Brazilian regions Etiology South Southeast Midwest Northeast North Total n % n % n % n % n % n % Ischemic 58 33.6 213 32.6 15 22.8 67 31.9 27 16.5 380 30 Idiopathic dilated cardiomyopathy 12 7 93 14.3 4 6.1 41 19.6 33 20.1 183 14.5 Hypertensive 56 32.6 98 15 7 10.6 34 16.3 61 37.2 256 20.3 Chagas disease 4 2.3 80 12.3 28 42.4 13 6.2 11 6.7 136 10.8 Valvular disease 24 14 80 12.3 2 3 30 14.4 20 12.2 156 12.4 Secondary to chemotherapeutic agents 1 0.6 2 0.3 0 0 2 1 0 0 5 0.4 Myocarditis 2 1.2 5 0.8 2 3 1 0.5 0 0 10 0.8 Others 15 8.7 74 11.3 8 12.1 20 9.6 12 7.3 129 10.2 Missing 0 0 7 1.1 0 0 1 0.5 0 0 8 0.6 172 100 652 100 66 100 209 100 164 100 1,263 100 Total decompensation; 3) the prescription of drugs, mainly vasodilators, according to current evidence was below the expected rate for this population; and 4) high intrahospital mortality rate. drug adherence leads to increased morbidity, mortality and costs 18. In addition to that, advanced age is a risk factor for poor adherence which increases even more with polypharmacy, increasing the likelihood of adverse events. Patients with advanced age accounted for an important segment of the sample studied in BREATHE and predominated in the South and Southeast regions, where the ischemic etiology was also more prevalent. Studies about drug adherence demonstrate highly variable rates of adherence among patients with HF. A study reported adherence rates of 79% for ACEi/ARB, 65% for beta-blockers and 56% for spironolactone after five years from the first hospitalization for HF19. In contrast, the noncompliance rate based on pill count was much lower Among patients with chronic diseases, approximately 50% do not take medications as prescribed. This poor Arq Bras Cardiol. 2015; 104(6):433-442 436 Albuquerque et al. BREATHE: Characteristics, Indicators and Outcomes Original Article Table 3 – Distribution of causes of heart failure decompensation Table 4 – Events and procedures during hospitalization % (n = 1,250) Events/procedures % (n/total) Infection 22.7 Intrahospital mortality 12.6 (1,57/1,245) Poor medication adherence 29.9 Coronary artery bypass grafting 0.7 (9/197) Increased ingestion of sodium and water * 8.9 Valve replacement 12.4 (156/197) Acute valvular disease 6.6 Heart transplantation 1.2 (15/197) Cardiac arrhythmia 12.5 Coronary angioplasty 1.5 (19/197) Pulmonary embolism 0.4 Implantable defibrillator/Resynchronizer 1.2 (15/197) Others 32.4 Cardiac pacemaker 1.7 (22/197) Decompensation cause *Total with complete information 1,242 patients. * Of the total, only 197 patients had procedures performed during hospitalization. 100.0% 90.0% 80.0% 67.4% 70.0% 60.0% 50.0% 40.0% 30.0% 20.0% 10.0% 0.0% 17.8% 9.6% Dry-warm 5.2% wet-warm Wet-cold Dry-cold Figure 2 – Hemodynamic profile on hospital admission. in the CHARM study, in which 11% of the patients took less than 80% of the prescribed pills20. Adherence is associated with several factors and should not be regarded as the sole responsibility of the patient. The BREATHE study pointed out that only slightly more than 50% of the patients received guidelines for correctly taking the medications, and only 43.5% were advised about the recognition of worsening of symptoms and future appointments. Preliminary evidence shows that around 35% of the inpatients with acute HF receive appropriate instructions on hospital discharge, with academic centers showing worse performance in this indicator of the JCAHO21. Of still greater relevance and impact on the prescription of medication on discharge is the medication introduced during the hospital phase. This analysis demonstrates that there are still considerable gaps in the treatment of acute HF in Brazil. 437 Arq Bras Cardiol. 2015; 104(6):433-442 The treatment frequently does not follow current published guidelines, which may contribute to the high morbidity, mortality and economic cost of this syndrome16. The IMPROVE-HF study showed that the addition of each evidence-based therapy was associated with a decreased risk of mortality in 24 months, with incremental benefit. This strong positive association between the use of evidence-based therapies and improved risk-adjusted survival reached a plateau after 4‑5 therapies included in the therapeutic armamentarium of the patient with HF22. Despite the fact that the clinical hemodynamic profile wet‑warm was the most common in the present study, only 6.6% of the population received intravenous vasodilators, whereas 42.2% of the patients received ACEi during the hospital phase. Around 18% of the patients showed a wet‑cold profile on hospital admission, but only 13.6% received Albuquerque et al. BREATHE: Characteristics, Indicators and Outcomes Original Article 100.0% 89.9% 90.0% 80.0% 70.0% 57.1% 60.0% 50.0% 40.0% 30.0% 23.5% 20.0% 10.0% 0.0% 46.2% 42.2% 13.6% 6.6% Intravenous vasodilator Inotropes ACEi* Loop Diuretics ARB† Betablocker Aldosterone Antagonist Figure 3 – Medications administered during the hospital stay. * ACEi: angiotensin converting enzyme inhibitor; †ARB: angiotensin II receptor blocker. 100.0% 90.0% 80.0% 67.3% 70.0% 60.0% 50.0% 40.0% 44.2% 34.9% 30.0% 16.2% 20.0% 10.0% 10.0% 0.0% Diet Medications Use Physical Activity Symptom Worsening Quit Smoking† Figure 4 – Guidelines on hospital discharge according to the indicators of care quality during hospitalization for heart failure (according to the JCAHO*). * Joint Commission on Accreditation of Healthcare Organization. † Applicable to smokers inotropes. Beta‑blockers were prescribed to only 57.1% of the studied sample. In contrast, loop diuretics were prescribed to approximately 90% of the patients. Results from the analysis of the ADHERE registry suggest that starting vasodilator therapy in the emergency department correlates with shorter hospital stays and fewer transfers to the intensive care unit, as well as higher percentages of asymptomatic patients at hospital discharge23. Additionally, there was a substantial improvement in the survival rate of patients receiving intravenous vasodilators (nitroglycerin or nesiritide), compared with those who received intravenous inotropes (dobutamine Arq Bras Cardiol. 2015; 104(6):433-442 438 Albuquerque et al. BREATHE: Characteristics, Indicators and Outcomes Original Article or milrinone)24. However, it is possible that patients requiring inotropic therapy have a more advanced form of HF than patients who receive vasodilators. Analysis of the Euro Heart Survey clearly showed that patients included in randomized clinical trials are a highly selected group and that only a small proportion of the patients in this registry would be eligible. However, beta-blockers and ACEi were prescribed for less than half of the eligible patients and the doses used were below those which have proven to be effective. Therefore, the lack of similarity between patients with HF in clinical practice and those in clinical trials does not adequately explain the underutilization of the therapy25. Intrahospital treatment invariably has a direct impact on clinical events during hospitalization. The prognosis of HF is reserved and directly related to the loss of functional capacity. Data from the Framingham study showed a median survival rate after diagnosis of 1.7 years for men and 3.2 years for women. The high mortality, morbidity and impairment of quality of life related to HF affects primarily the elderly. Although we may observe a consistent and significant survival benefit in patients with HF with use of aggressive pharmacological strategies, the annual mortality of this disease remains high26-31. The CONSENSUS (Cooperative North Scandinavian Enalapril Survival Study)32 and PROMISE (Prospective Randomized Milrinone Survival Evaluation)33 studies, for example, identified a high proportion of patients with annual mortality exceeding 30%. In more recent studies, the mortality of patients with functional class III-IV after 1 year of optimized treatment, including the routine use of ACEi and beta-blockers, was approximately 10-15%34. Although these values are encouraging, such mortality rates are also similar to those observed in many neoplastic diseases. As for intrahospital mortality, it affects between 3% to 4% of the patients admitted for acute HF in prior studies35, whereas the mortality rate in the BREATHE registry exceeds in two times the rates from American and European registries. In the ADHERE study, intrahospital mortality was 4.0%, and the average hospital stay was 4.3 days36. Similar to the American registry, the Euro Heart Survey presented an overall intrahospital mortality rate of 3.8%, with 90.1% due to a cardiovascular cause. Higher mortality rates were observed in the presence of cardiogenic shock37. Some limitations inherent to the design of BREATHE should be considered in the interpretation of its results. The diagnosis of acute HF was based only on the Boston criteria and the date of onset of symptoms was not defined, therefore it was not possible to differentiate new acute HF from exacerbation of chronic HF. Consequently, since the population is heterogeneous, the analysis of treatment and prognosis will require appropriate adjustment. In addition, the number of missing data was elevated due to some variables whose completion was not mandatory, interfering with the results found. Conclusion BREATHE is the first Brazilian registry of acute HF and its results point to the high rate of intrahospital mortality related to low rates of evidence-based therapy prescribed during hospitalization, as well as low percentage of medical guidelines on hospital discharge of patients hospitalized for acute HF in different regions of Brazil. New strategies must be adopted to ensure improvement in the quality of hospital care of this disease. Author contributions Conception and design of the research: Albuquerque DC, Souza-Neto JD, Bacal F, Rohde LEP. Acquisition of data: researchers BREATHE, Albuquerque DC, Souza-Neto JD, Rohde LEP, Bernardez- Pereira S, Almeida DR. Analysis and interpretation of the data: Albuquerque DC, Rohde LEP, Bernardez-Pereira S, Berwanger O. Statistical analysis: Bernardez-Pereira S. Obtaining financing: Albuquerque DC. Writing of the manuscript: Albuquerque DC, Souza-Neto JD, Bacal F, Rohde LEP, Bernardez-Pereira S, Almeida DR. Critical revision of the manuscript for intellectual content: Albuquerque DC, Souza- Neto JD, Bacal F, Rohde LEP, Bernardez-Pereira S, Berwanger O, Almeida DR. Potential Conflict of Interest No potential conflict of interest relevant to this article was reported. Sources of Funding This study was funded by Departamento de Insuficiência Cardíaca da Sociedade Brasileira de Cardiologia. Study Association This study is not associated with any thesis or dissertation work. Supplement I – Distribution of the BREATHE patients by region (planned versus included) Major Regions Brazil 439 Hospitalization in health establishments in the year of 2004 Total IBGE Total BREATHE referred Total BREATHE Included 23,252,613 (100%) 1,200 1,263 North 1,746,554 (8%) 96 164 Northeast 5,254,978 (23%) 276 209 Southeast 10,794,799 (46%) 552 652 South 3,671,762 (16%) 192 172 Midwest 1,784,520 (8%) 96 66 Arq Bras Cardiol. 2015; 104(6):433-442 Albuquerque et al. BREATHE: Characteristics, Indicators and Outcomes Original Article Included (n = 1263) Excluded. Presence of exclusion criteria (n = 2) Analyzed (n = 1261) Without information at hospital discharge (n = 18) Complete follow-up (n = 1245) Supplement II – Flow diagram of the BREATHE study. List of participants BREATHE Hospital de Clínicas Gaspar Viana: Helder José Lima Reis; Hospital de Base FAMERP: Paulo Roberto Nogueira; Hospital do Coração: Ricardo Pavanello; Hospital São Lucas – PUCRS: Luiz Claudio Danzmann; Hospital de Messejana: João David de Souza Neto; Instituto Dante Pazzanese: Elizabete Silva dos Santos; Hospital de Clínicas de Porto Alegre: Luis Eduardo Paim Rohde; InCor SP: Mucio Tavares de Oliveira Filho; Real Hospital Português: Silvia Marinho Martins; Hospital Universitário Clementino Fraga Filho: Marcelo Iorio Garcia; Hospital Total Cor: Antonio Baruzzi; Hospital Universitário Prof. Alberto Antunes: Maria Alayde Mendonça da Silva; Hospital Barra D’Or: Ricardo Gusmão; Hospital do Coração de Goiás: Aguinaldo Figueiredo de Freitas Júnior; Hospital Vera Cruz: Fernando Carvalho Neuenschwander; Hospital Universitário de Londrina: Manoel Fernandes Canesin; Hospital Copa D’or: Denilson Campos de Albuquerque; Hospital das Clínicas da Universidade Federal de Goiás: Salvador Rassi; Instituto Cardiopulmonar: Eduardo Darzé; Santa Casa de Votuporanga: Mauro Esteves Hernandes; Hospital Universitário Pedro Ernesto: Ricardo Mourilhe Rocha; São Lucas Médico Hospitalar: Antonio Carlos Sobral Sousa; Hospital Universitário Presidente Dutra-HUUFMA: Jose Albuquerque de Figueiredo Neto; Centro de Pesquisa da Clínica Médica e Cardiologia da UNIFESP: Renato D. Lopes; Unidade de Insuficiência Cardíaca – InCor: Edimar Alcides Bocchi; Hospital Quinta Dor: Jacqueline Sampaio; Hospital Lifecenter: Estêvão Lanna Figueiredo; Xeno Diagnósticos Dante Pazzanese: Abilio Augusto Fragata Filho; Fundação Bahiana de Cardiologia: Alvaro Rabelo Alves Júnior; Instituto de Cardiologia do Distrito Federal: Carlos V. Nascimento; Hospital Auxiliar do Cotoxó: Antonio Carlos Pereira-Barretto; Fundação Beneficência Hospital de Cirurgia/ Hospital do Coração: Fabio Serra Silveira; Hospital Santa Izabel: Gilson Soares Feitosa; Hospital Regional Hans Dieter Schmidt: Conrado Roberto Hoffmann Filho; Hospital Univ. Antonio Pedro – UFF: Humberto Villacorta Júnior; Hospital Universitário São Jose: Sidney Araújo; Hospital das Clínicas de Botucatu UNESP Botucatu: Beatriz Bojikian Matsubara; Hospital Santa Paula: Otávio Gebara; Casa de Saúde São José: Gustavo Luiz Gouvea de Almeida; Hospital das Clínicas da UFMG: Maria da Consolação Vieira Moreira; Hospital Madre Tereza: Roberto Luiz Marino; São Bernardo Apart Hospital: João Miguel de Malta Dantas; Instituto Nacional de Cardiologia: Marcelo Imbroinise Bittencourt; Hospital da Cidade: Marcelo Silveira Teixeira; Hospital Rios Dor: Elias Pimentel Gouvea; Hospital das Clínicas de Ribeirão Preto/ USP-FMRP: Marcus Vinícius Simões; Santa Casa de São Paulo: Renato Jorge Alves; Hospital Espanhol: Fabio Villas-Boas; Unidade de Miocardiopatia InCor: Charles Mady; Hospital Escola Alvaro Alvim: Felipe Montes Pena; Hospital Univ. João de Barros Barreto – UFPA: Eduardo Costa. Arq Bras Cardiol. 2015; 104(6):433-442 440 Albuquerque et al. BREATHE: Characteristics, Indicators and Outcomes Original Article References 1. Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, et al; American Heart Association Statistics Committee and Stroke Statistics Subcommittee.Heart disease and stroke statistics--2014 update: a report from the American Heart Association. Circulation. 2014;129(3):e28-e292. 20. Granger BB, Swedberg K, Ekman I, Granger CB, Olofsson B, McMurray JJ, et al ; CHARM Investigators. Adherence to candesartan and placebo and outcomes in chronic heart failure in the CHARM programme: double-blind, randomised, controlled clinical trial. Lancet. 2005;366(9502):2005-11. 2. 21. Fonarow GC, Yancy CW, Heywood JT; ADHERE Scientific Advisory Committee, Study Group, and Investigators. Adherence to heart failure quality-of-care indicators in US hospitals: analysis of the ADHERE Registry. Arch Intern Med. 2005;165(13):1469-77. 3. Heidenreich PA, Albert NM, Allen LA, Bluemke DA, Butler J, Fonarow GC, et al; American Heart Association Advocacy Coordinating Committee; Council on Arteriosclerosis, Thrombosis and Vascular Biology; Council on Cardiovascular Radiology and Intervention; Council on Clinical Cardiology; Council on Epidemiology and Prevention; Stroke Council. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail. 2013;6(3):606-19. Bocchi EA. Heart failure in South America. Curr Cardiol Rev. 2013;9(2):147-56. 4. Ministério da Saúde. Datasus: mortalidade - 1996 a 2012, pela CID-10 – Brasil [Internet]. Brasília (DF); 2008. [citado em 2014 dez 03]. Disponível em: http://tabnet.datasus.gov.br/cgi/deftohtm.exe?sim/cnv/obt10uf.def 5. Roger VL. Epidemiology of heart failure. Circ Res.2013;113(6):646-59. 6. Solomon SD, Dobson J, Pocock S, Skali H, McMurray JJ, Granger CB, et al. Candesartan in heart failure: assessment of reduction in mortality and morbidity (CHARM) investigators. Influence of nonfatal hospitalization for heart failure on subsequent mortality in patients with chronic heart failure. Circulation. 2007; 116(113):182-7. 7. Chin MH, Goldman L. Correlates of early hospital readmission or death in patients with congestive heart failure. Am J Cardiol .1997;79(12):1640-4. 8. Chin MH, Goldman L. Correlates of major complication or death in patients admitted to the hospital with congestive heart failure. Arch Intern Med. 1996;156(16):1814-20. 9. Chin MH, Goldman L. Factors contributing to the hospitalization of patients with congestive heart failure. Am J Public Heath.1997;87(4):643-8. 10. Stewart S, Blue L, Capewell S, Horowitz JD, McMurray JJ. Poles apart, but are they the same? A comparative study of Australia and Scottish patients with chronic heart failure. Eur J Heart Fail. 2001;3(2):249-55. 11. Tavares L, Silva GP, Pereira SB, Souza G, Pozam R, Coutinho S, et al. Análise ecocardiográfica e etiológica dos pacientes internados por insuficiência cardíaca na cidade de Niterói. Arq Bras Cardiol. 2002;79(supl.4):35. 12. Tavares L, Silva GP, Pereira SB, Souza G, Pozam R, Victer H, et al. Comorbidades e fatores de descompensação dos pacientes internados por insuficiência cardíaca descompesada na cidade de Niterói. Arq Brás Cardiol. 2002;79(supl.4):35 13. Investigadores do BREATHE. Racionalidade e métodos - estudo BREATHE – I Registro brasileiro de insuficiência cardíaca. Arq Bras Cardiol. 2013;100(5):390-4. 14. Carlson KJ, Lee DC, Goroll AH, Leahy M, Johnson RA. An analysis of physicians’ reasons for prescribing long-term digitalistherapy in outpatients. J Chronic Dis. 1985;38(9):733-9. 23. Peacock WF, Fonarow GC, Emerman CL, Mills RM, Wynne J; ADHERE Scientific Advisory Committee and Investigators; Adhere Study Group. Impact of early initiation of intravenous therapy for acute decompensated heart failure on outcomes in ADHERE. Cardiology. 2007;107(1):44-51. 24. Abraham WT, Adams KF, Fonarow GC, Costanzo MR, Berkowitz RL, LeJemtel TH, et al; ADHERE Scientific Advisory Committee and Investigators; ADHERE Study Group.In-hospital mortality in patients with acute decompensated heart failure requiring intravenous vasoactive medications: an analysis from the Acute Decompensated Heart Failure National Registry (ADHERE). J Am Coll Cardiol. 2005;46(1):57-64. 25. Lenzen MJ, Boersma E, Reimer WJ, Balk AH, Komajda M, Swedberg K, et al. Under-utilization of evidence-based drug treatment in patients with heart failure is only partially explained by dissimilarity to patients enrolled in landmark trials: a report from the Euro Heart Survey on Heart Failure. Eur Heart J. 2005;26(24):2706-13. 26. Richembacher PR, Trindade PT, Haywood GA, Vagelos RH, Schroeder JS, Willson K, et al. Transplant candidates with severe left ventricular dysfunction managed with medical treatment: characteristics and survival. J Am Coll Cardiol. 1996;27(5):1192-7. 27. McKee PA, Castelli WP, McNamara PM, Kannel WB. The natural history of congestive heart failure: the Framingham study. N Engl J Med. 1971;285(26):1441-6. 28. Franciosa JA, Willen M, Ziesche S, Cohn JN. Survival in men with severe chronic left ventricular failure to either coronary heart disease or idiopathic dilated cardiomyopathy. Am J Cardiol .1983;51(5):831-6. 29. Cohn JN, Archibald DG, Ziesche S, Franciosa JA, Harston WE, Tristani FE, et al.Effect of vasodilatador therapy on mortality in chronic congestive heart failure: results of a Veterans Administration Cooperative Study. N Engl J Med. 1986;314(24):1547-52. 30. The SOLVD Investigators. Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. N Engl J Med. 1991;325(5):293-302. 15. Stevenson LW, Perloff JK. The limited reliability of physical signs for estimating hemodynamics in chronic heart failure. JAMA.1989;261(6):884-8. 31. Pfeffer MA, Braunwald E, Moyé LA, Basta L, Brown EJ Jr, Cuddy TE, et al. Effect of captopril on mortality in patients with left ventricular dysfunction after myocardial infarction: results of the Survival and Ventricular Enlargement Trial. N Engl J Med. 1992;327(10):669-77. 16. Montera MW, Almeida RA, Tinoco EM, Rocha RM, Moura LZ, Réa-Neto A, et al., Sociedade Brasileira de Cardiologia. II Diretriz brasileira de insuficiência cardíaca aguda. Arq Bras Cardiol.2009;93(3 supl.3):1-65. 32. The CONSENSUS Trial Study Group. Effects of enalapril on mortality in severe congestive heart failure (CONSENSUS). N Engl J Med. 1987;316(23):1429-35. 17. Common Statistical Methods for Clinical Research with SAS Examples (3rd ed.) by Glenn A. Walker and Jack Shostak.; Cary, NC: SAS Institute, 2010. 33. Massie B, Bourassa M, DiBianco R, Hess M, Konstam M, Likoff M,et al. for The Amrinone Multicenter Study Group: long term oral administration of amrinone for congestive heart failure: lack of efficacy in a multicenter controlled trial. Circulation. 1985;71(5):963-71. 18. Brown MT, Bussell JK. Medication adherence: WHO cares? Mayo Clin Proc. 2011;86(4):304-14. 19. Gislason GH, Rasmussen JN, Abildstrom SZ, Schramm TK, Hansen ML, Buch P, et al. Persistent use of evidence-based pharmacotherapy in heart failure is associated with improved outcomes. Circulation.2007;116(7):737-44. 441 22. Fonarow GC, Albert NM, Curtis AB, Gheorghiade M, Liu Y, Mehra MR, et al. Incremental reduction in risk of death associated with use of guidelinerecommended therapies in patients with heart failure: a nested case-control analysis of IMPROVE HF. J Am Heart Assoc. 2012;1(1):16-26. Arq Bras Cardiol. 2015; 104(6):433-442 34. Packer M1, Fowler MB, Roecker EB, Coats AJ, Katus HA, Krum H, et al. Effect of carvedilol on survival in severe chronic heart failure: results of the carvedilol prospective randomized cumulative survival (COPERNICUS) study. N Engl J Med. 2001;344(22):1651-8. Albuquerque et al. BREATHE: Characteristics, Indicators and Outcomes Original Article 35. Francis GS. Acute heart failure: patient management of a growing epidemic. Am Heart Hosp J. 2004;2(4 Suppl 1):10–4. Decompensated Heart Failure National Registry (ADHERE). Am Heart J. 2005;149(2):209-16. 36. Adams KF Jr, Fonarow GC, Emerman CL, LeJemtel TH, Costanzo MR, Abraham WT, et al; ADHERE Scientific Advisory Committee and Investigators.Characteristics and outcomes of patients hospitalized for heart failure in the United States: rationale, design, and preliminary observations from the first 100,000 cases in the Acute 37. Maggioni AP, Dahlström U, Filippatos G, Chioncel O, Crespo Leiro M, Drozdz J, et al; Heart Failure Association of the European Society of Cardiology (HFA). EURObservational Research Programme: regional differences and 1-year follow-up results of the Heart Failure Pilot Survey (ESC-HF Pilot). Eur J Heart Fail. 2013;15(7):808-17. Arq Bras Cardiol. 2015; 104(6):433-442 442 Back to the Cover Original Article Depression as a Clinical Determinant of Dependence and Low Quality of Life in Elderly Patients with Cardiovascular Disease Giselle Helena de Paula Rodrigues, Otavio Celso Eluf Gebara, Catia Cilene da Silva Gerbi, Humberto Pierri, Mauricio Wajngarten Instituto do Coração de São Paulo - INCOR/HC-FMUSP, São Paulo, SP – Brazil Abstract Background: The aging process promotes a progressive increase in chronic-degenerative diseases. The effect of these diseases on the functional capacity has been well recognized. Another health parameter concerns “quality of life related to health”. Among the elderly population, cardiovascular diseases stand out due to the epidemiological and clinical impact. Usually, these diseases have been associated with others. This set of problems may compromise both independence and quality of life in elderly patients who seek cardiologic treatment. These health parameters have not been well contemplated by cardiologists. Objective: Evaluating, among the elderly population with cardiovascular disease, which are the most relevant clinical determinants regarding dependence and quality of life. Methods: This group was randomly and consecutively selected and four questionnaires were applied: HAQ, SF-36, PRIME-MD e Mini Mental State. Results: The study included 1,020 elderly patients, 63.3% women. The group had been between 60 and 97 years-old (mean: 75.56 ± 6.62 years-old). 61.4% were independent or mild dependence. The quality of life total score was high (HAQ: 88.66 ± 2.68). 87.8% of patients had a SF-36 total score ≥ 66. In the multivariate analysis, the association between diagnoses and high degrees of dependence was significant only for previous stroke (p = 0.014), obesity (p < 0.001), lack of physical activity (p = 0.016), osteoarthritis (p < 0.001), cognitive impairment (p < 0.001), and major depression (p < 0.001). Analyzing the quality of life, major depression and physical illness for depression was significantly associated with all domains of the SF-36. Conclusion: Among an elderly outpatient cardiology population, dependence and quality of life clinical determinants are not cardiovascular comorbidities, especially the depression. (Arq Bras Cardiol. 2015; 104(6):443-449) Keywords: Depression; Aged; Cardiovascular Diseases; Frail Elderly; Quality of Life. Introduction With an aging population, the prevalence of chronic diseases has progressively increased1. The impact of these diseases on functional capacity, which corresponds to the capacity and independence to perform certain daily tasks, has been recognized2. Another health parameter with a relatively recent evolution is the concept of “quality of life” (QoL) or, preferably, “healthrelated quality of life” (HRQoL), which emphasizes the impact of health status on the individual’s quality of life. It derives from individuals’ experience regarding their health problems, comprising several domains not always prioritized by health professionals and has important implications for the assessment of the effects of therapeutic interventions. Mailing Address: Giselle Helena de Paula Rodrigues • Rua Ministro Godoi, 1186, apto.12, Perdizes. Postal Code 05015-001, São Paulo, SP – Brazil E-mail: [email protected]; [email protected] Manuscript received July 25, 2014; revised manuscript October 17, 2014; accepted October 30, 2014. DOI: 10.5935/abc.20150034 443 Thus, the evaluation of these health parameters has emerged as an important part of the clinical examination in this population, making health teams start aiming at functional status improvement and well-being, in addition to the survival of elderly patients3. In the elderly population, cardiovascular diseases stand out due to their high epidemiological and clinical impact. They are usually associated with other diseases, including neuropsychiatric ones, which may have mutual influence. One example is the association between systemic arterial hypertension (SAH), cognitive decline and depression, physiopathologically expressed by anatomical and functional abnormalities of cerebral circulation4-6. Another interesting association was found between major depression and cardiovascular disease, also explained by changes in microcirculation, which deserves further investigation7. Obviously, this set of problems can impair independence and quality of life of elderly individuals seeking cardiologic treatment. In this sense, the role of neuropsychiatric conditions has been emphasized, as expressed by the aphorism that “there is no health without mental health”8. According to the last IBGE (Brazilian Institute of Geography and Statistics) census in 2010, there was a significant change in the Brazilian scenario of disease distribution, Rodrigues et al. Depression in elderly patients with cardiovascular diseases Original Article when compared to that of 1990. Ischemic heart diseases occupied the 1st position in 2010 in terms of prevalence, whereas depression, the 6th position. Differently from what was observed in 1990, when they occupied the 4th and the 10th positions, respectively9. Another very interesting fact is that currently, life expectancy in Brazil is 74.1 years. Of this total, only 63.8 years are lived in good health status9. Based on these findings, we verify the importance of adequate investigation of quality of health and depression in patients in all health care levels. Clinical trials such as the Improving Mood-Promoting Access to Collaborative Treatment (IMPACT)10 and the Coronary Psychosocial Evaluation Studies (COPES)11 showed not only the health benefits of individuals systematically evaluated for depression in primary care, but also reduced costs with future medical care. Although some studies show the impact of chronicdegenerative diseases on elderly independence, especially dementia and other chronic neurological diseases12, these health parameters have been relatively disregarded by cardiologists, both in research and in clinical practice13,14. Researches tend to exclude elderly patients with comorbidities 15 , in addition to rarely considering independence and QoL as outcomes. Consequently, with few exceptions 16, these studies fail to reflect the “real world”, which has influence on Guidelines, education and clinical practice. The objective of this study is to evaluate, in a population of elderly patients from a cardiology outpatient clinic of a referral hospital, whether the most relevant clinical determinants of dependency and QoL are cardiovascular diseases or other highly prevalent comorbidities in this group, such as depression. Method Clinical evaluation was made by a single physician in accordance with data from patients’ medical records. In parallel to the clinical evaluation, the patients were assessed by a single psychologist who applied a set of four questionnaires validated internationally and in Brazil: Health Assessment Questionnaire (HAQ) 17 Short-Form Health Survey (SF-36)18, New Procedure for Diagnosing mental Disorders in Primary Care (PRIME-MD) 19 and Mini‑mental State Examination (MMSE)20. All diseases were classified as present or absent. According to degree of dependence, the group was divided in two: • Independent and with mild dependence: HAQ score from 0 to 1.4; • Moderate and severe dependence: HAQ scores from 1.5 and 3.0. Quality of life was assessed according to SF-36. Based on the mean scores, the group was divided into two: above and below the mean. Patients with cognitive impairment that could interfere with the final result of this analysis were excluded from the calculations. The population was then divided into tertiles of the SF-36 score: score between 0 and 33; > 33 and 66; and those with scores > 66. All subjects with MMSE < 18 were considered as possible dementia cases. Sample Size Calculation and Statistical Analysis For this study, considering the chances of the above listed events, according to the statistical inference theory and taking into account that the confidence interval at the level of (1-Ω)%, where Ω is 5%, we obtained an estimated sample size of 870 patients. We chose to increase this sample to 1,020 patients (approximately 25% more), to ensure that the analysis of association strength of multiple assessed diagnoses would be possible and to minimize the chance of a statistical beta error. Population The studied individuals originated from the Geriatric Cardiology Unit of Instituto do Coração, Hospital das Clínicas of the School of Medicine of Universidade de São Paulo (InCor – HC/FMUSP), and the study was approved by the Research Ethics Committee of this institution. The elderly participants were randomly selected, until a total sample of 1,020 individuals was achieved. Exclusion criteria Patients that had cognitive impairment, i.e., score < 18 at the Mini-Mental State Examination (MMSE) were not considered for the calculation of their QoL, as they had some difficulty in answering the QoL questionnaire questions (SF-36). Methodology This is an epidemiological, observational and crosssectional study, lasting approximately three years for the selection of all individuals. Statistical Analysis Pearson’s chi-square test was used to test the significance of associations between cardiovascular diseases and other comorbidities with HAQ, while Student’s t test was used to assess the association between cardiovascular diseases and other comorbidities with each of the 8 domains of the SF-36. Uni- and multivariate tests were applied to study the possible associations between the analyzed variables and patients’ QoL. To verify the strength of these associations, the odds ratio was calculated for each of these variables in relation to the degree of dependence and QoL. In order to evaluate which, among the analyzed variables, were significantly and independently associated with the degrees of dependence (HAQ) and QoL, a stepwise multivariate logistic regression model was developed, which included the statistically significant associations in the univariate analyses. Significance level was set at 5% (p ≤ 0.05) in the statistical tests and the Statistical Analysis Software (SAS Institute Inc., NC, USA) was employed. Arq Bras Cardiol. 2015; 104(6):443-449 444 Rodrigues et al. Depression in elderly patients with cardiovascular diseases Original Article Results Demographic and clinical characteristics of the study population The study included 1,020 individuals aged 60 years or older, of which 646 were women and 374 men. Age ranged from 60 to 97 years (mean: 75.56 years / SD: 6.62 years) and 17.74% were aged between 60 and 69 years; 55% between 70 and 79 years; 25.88% between 80 and 89 years and 1:37% between 90 and 97 years. Caucasians were 74.9% of the total sample, with the other individuals being classified as African-descendants (9.5%), Asian-descendants (2.0%) and Mixed-race (13.5%). The following were the most prevalent cardiovascular diseases: heart failure (HF), coronary artery disease (CAD) and atrial fibrillation (AF), followed by acute myocardial infarction (AMI) and previous cerebrovascular accident (CVA). Other comorbidities that showed high prevalence in the group were: lack of regular physical activity, systemic arterial hypertension (SAH) and dyslipidemia (DLP), in addition to obesity, diabetes mellitus (DM), smoking, osteoarthritis (OA), chronic obstructive pulmonary disease (COPD), chronic renal failure (CRF), cognitive impairment and depression (Table 1). It is noteworthy that 57.1% of the study population had depression (major or minor). Of these patients, 37% had depression due to physical illness. When analyzing quality of life, it is verified that the total QoL score was high and no patient had a SF-36 score < 33. Most of the patients (87.7%) had a total SF-36 score > 66 (Table 3). Association between Diagnoses and Degrees of Dependence At the multivariate analysis, the association between diagnoses and high degrees of dependence was significant only for previous CVA (p = 0.014), obesity (p < 0.001), lack of physical activity (p = 0.016), osteoarthritis (p < 0.001), cognitive impairment (p < 0.001) and major depression (p < 0.001) (Table 4). Association between Diagnoses and Quality of Life When the multivariate analysis is performed, the variables below are the ones that best explain a lower quality of life in each of its domains (Table 5). Table 2 – Degrees of dependence according to HAQ Dependence (HAQ) Number of patients (n) Frequency (%) < 1.5 624 61.2 ≥ 1.5 396 38.8 HAQ: Health Assessment Questionnaire. Additionally, most of the population (61.4%) showed to be independent or slightly dependent (Table 2). Table 3 – Quality of life of the Population, according to SF-36 Table 1 – Prevalence of the most common diagnoses in the population Diagnoses Number of patients (n) Frequency (%) SAH 882 86.5 DLP 492 48.2 COPD 95 9.31 Obesity 279 27.4 DM 267 26.2 Cognitive deficit 118 11.6 CRF 100 9.8 HF 338 33.2 CAD 331 32.5 AF 215 21.2 AMI 136 13.3 Stroke 85 8.3 Major Depression 472 46.3 Minor Depression 111 10.8 Depression Phys.Dis. 378 37.0 Absence of. physical activity 990 96.9 Smoking 65 6.4 SAH: hypertension; DLP: dyslipidemia; COPD: chronic obstructive pulmonary disease; DM: diabetes; CRF: chronic renal failure; HF: heart failure; CAD: oronary artery disease; AF: atrial fibrillation; AMI: acute myocardial infarction. 445 Arq Bras Cardiol. 2015; 104(6):443-449 SF-36 (total score) Number of patients (n) Frequency (%) 33 – 66 110 12.2 ≥ 66 792 87.8 Table 4 – Multivariate analysis between diagnoses and high degrees of dependence Diagnoses Stroke Odds ratio 1.97 95%CI LI LS 1.15 3.37 p 0.014 HF 1.25 0.89 1.75 0.203 SAH 1.60 0.99 2.59 0.053 DM 1.21 0.82 1.77 0.336 Obesity 2.24 1.59 3.15 < 0.001 Physical Inactivity 0.08 0.01 0.62 0.016 OA 1.64 1.14 2.37 0.008 Cognitive deficit 3.17 2.02 4.98 < 0.001 Major Depression 2.76 1.86 4.10 < 0.001 Minor Depression 1.14 0.65 1.99 0.642 Depression Phys. Dis. 1.31 0.90 1.89 0.160 HF: heart failure; SAH: hypertension; DM: diabetes; OA: osteoarthritis. Rodrigues et al. Depression in elderly patients with cardiovascular diseases Original Article Thus, the following were significantly associated with lower degrees of quality of life, according to the following domains of the SF-36 at the multivariate analysis: • Limitation for physical activities due to health problems (D1): HF, CAD, AMI, lack of physical activity, hypertension, obesity, OA, major depression and depression due to physical illness; • Limitation for social activities due to physical and emotional problems (D2): HF, AF, lack of physical activity, OA, and major depression and depression due to physical illness; • Limitation of daily activities due to physical changes (D3): AF, lack of physical activity, SAH, obesity, OA, and major depression and depression due to physical illness; • Pain (D4): SAH, COPD, major depression and depression due to physical illness; • Less vitality (D7): CAD, DLP, major depression and depression due to physical illness; • Worse perception of one’s health (D8): CRF, major depression and depression due to physical illness. Discussion Among the elderly patients studied, depression showed high prevalence, with great impact on the independence and QoL of these individuals. This fact is surprising, as we are analyzing a group of individuals with multiple comorbidities, apparently more significant than the depression. Recently, three major challenges were identified by physicians interested in improving care for their elderly patients with multiple comorbidities: 1.Difficulty in applying the guidelines and need to individualize according to the patients’ reality; • Worse general mental health - stress and well-being - (D5): COPD, major depression, minor depression and depression due to physical illness; 2.Difficulty in choosing one of the strategies: prioritize certain clinical entities, treat diseases individually, considering the risk of each of them or start treatment before adverse effects occur; • Limitation in basic activities due to emotional problems (D6): HF, CVA, DLP, and major depression and depression due to physical illness; Table 5 – Multivariate analysis between diagnosis and low degrees of quality of life D1 D2 D3 OR p OR p HF 1.89 0.0057 1.56 0.0089 CAD 1.81 0.0092 6.77 < 0.001 AF Physical Inactivity SAH 2.21 0.0014 Obesity 1.65 0.0486 OA 2.14 0.0072 D4 OR p 1.59 0.0110 2.03 0.0001 3.19 0.0048 4.78 0.0001 1.75 0.0085 2.04 0.0012 1.60 0.0146 COPD OR p 1.70 0.0073 1.88 0.0143 Major depression 3.05 < 0.0001 3.49 < 0.0001 2.31 < 0.0001 2.22 < 0.0001 Depression Phys. Dis. 2.83 0.0008 1.76 0.0052 2.12 < 0.0001 1.80 0.0007 D5 OR D6 p D7 OR p 2.08 0.0006 Stroke 1.90 0.0159 DLP 1.39 0.0206 HF CAD COPD 2.05 D8 OR p 1.52 0.0046 1.53 0.0023 OR p 1.98 0.0044 0.0229 CRF Major Depression 5.44 < 0.0001 Minor depression 1.91 0.0138 Depression Phys.Dis. 1.66 0.0309 3.16 < 0.0001 2.77 < 0.0001 6.08 < 0.0001 2.11 < 0.0001 1.43 0.0259 2.41 0.0001 HF: heart failure; CAD: coronary artery disease; AF: atrial fibrillation; SAH: hypertension; OA: osteoarthritis; COPD: chronic obstructive pulmonary disease; DLP: dyslipidemia; CRF: chronic renal failure. Arq Bras Cardiol. 2015; 104(6):443-449 446 Rodrigues et al. Depression in elderly patients with cardiovascular diseases Original Article 3. The conflict between physicians’ preferences and those of their patients21. The results of this study can help minimize these challenges and improve elderly care, as the reduction of dependence and QoL improvement are the fundamental objectives in patient care22. Additionally, it is known that there is a strong association between depression in the elderly and factors that increase mortality rates 23,24, such as poor adherence to medical treatment or lack of self-care25 for conditions such as diabetes, cardiovascular disease, smoking, sedentary life style 26, cognitive decline27 and dependence28. Thus, it is essential not only to perform the assessment of these factors, but mainly of the correlation between them. In this population, it is noteworthy the very high frequency of depression: almost half with major depression, 11% with minor depression and 37% of cases related to physical illness. The number of depressed individuals exceeds the expected, when compared to studies related to the topic29,30. However, several factors may influence the variation in the prevalence of depression, such as different diagnostic methods and sociodemographic characteristics. Studies show that women and individuals with lower education have more criteria for the diagnosis of depression31, whereas among the elderly, these criteria are less often identified, possibly because depression in this population is underdiagnosed or underreported32. Moreover, population studies have shown that the greatest risk factors for mental illness are not only chronic diseases, but also the socioeconomic differences and the difficulty in access to general and mental health31. Considering this is a population consisting exclusively of elderly cardiac patients, the high rate of depression could be explained by the known association between depression and cardiovascular disease. It is known that the presence of major depression may increase the risk of cardiovascular disease due to microcirculation abnormalities, although genetic factors also seem to be involved in this mechanism8. Recent epidemiological data showed a similar profile also among the very elderly, older than 85 years. It is remarkable that, in addition to several comorbidities and the fact that most are females, these elderly reported having good health quality and low degree of dependence33. In this study, the degree of dependence was low for more than half of patients. However, despite being able to attend the outpatient clinic, almost 40% showed high or moderate dependence (HAQ ≥ 1.5). Overall, the QoL score using the SF-36 was high, and no patient had scores below 33 and almost 90% had scores over 66. However, the score of the emotional domain was less than 65 in 55% of individuals, anticipating a great influence of depression on quality of life. When we analyzed the associations between different diagnoses and the patients’ degree of dependence, we verified a significant association for cardiovascular diagnoses of previous CVA, obesity and lack of regular physical activity, and for non-cardiovascular diagnoses of osteoarthritis, cognitive deficit and major depression (Table 2). 447 Arq Bras Cardiol. 2015; 104(6):443-449 It is relatively simple to explain higher levels of dependence for patients with previous CVA, osteoarthritis, cognitive deficit and major depressive disorder. On the other hand, lack of regular physical activity and obesity could be the consequences of dependence itself, justifying the observed association. It is noteworthy, however, the fact that dependence was more associated with non-cardiovascular comorbidities than with the diagnoses of cardiovascular diseases and risk factors. The lack of association between dependence and heart failure, although the latter was diagnosed in 33% of the sample and is a condition related to increased morbidity, can be explained by the compensation status and lower clinical impact at the time the study was performed. It should also be considered that the patients were able to come to the outpatient clinic and could represent a group of patients submitted to a lower degree of clinical impact. The same justification can be used for the lack of association with chronic obstructive pulmonary disease. When analyzing the associations between clinical diagnoses and the quality of life of individuals, we observed that most of the conditions were significantly associated with some of the SF-36 domains. However, the significant association between major depression and physical illness with all domains of the SF-36 should be especially noted, which does not occur with cardiovascular diagnoses. Similarly to what was observed regarding dependence, we emphasize the poor association between cardiovascular diagnoses and quality of life, whereas the diagnosis of depressive disorder showed a strong association. With the improvement of the assessment and intervention on the “modifiable” factors associated with an increased risk of disability 33, there has been a tendency toward the reduction of the degree of functional limitation and disability34. However, this parameter has been little studied in cardiology. Regarding quality of life, only recently there has been a wider application of tools to assess it in the cardiology setting35-37. This study shows that non-cardiovascular comorbidities, especially depressive disorders, have greater impact than cardiovascular disease and dependence on the quality of life of elderly individuals attending a cardiology clinic. This scenario highlights the importance of knowing the profile of elderly patients and including an effective geriatric assessment, integrating a broad assessment for possible functional loss and quality of life to the traditional clinical history38,39. In 2008, the American Heart Association (AHA) had already emphasized this necessity. In an important publication, the AHA supported that screening tests for depression should be applied to all patients with cardiovascular disease in all care settings: inpatient, outpatient or cardiovascular rehabilitation centers. The opportunity to diagnose and treat these patients should not be missed, as it can promote major improvements to patient health40. Thus, the adequacy of care services and education programs, as well as the training of professionals involved in elderly care becomes necessary. Rodrigues et al. Depression in elderly patients with cardiovascular diseases Original Article This study has some limitations. As this is an observational cross-sectional study, with only one assessment in time for all variables, the observed associations may not fully represent the reality of this population. Another limitation of this study refers to the source of the assessed patients, which is a n outpatient clinic of a high-complexity hospital, thus resulting in the selection bias of a more severely-ill population, which prevents the generalization of our findings to other groups. Moreover, only patients who were able to come to the outpatient clinic were assessed, probably excluding totally dependent and bedridden patients. Conclusion In a population of elderly patients treated in a cardiology outpatient clinic of a referral hospital, the most relevant clinical determinants of impairment dependence and quality of life are non-cardiovascular comorbidities, mainly depression. Author contributions Conception and design of the research:Rodrigues GHP, Gebara OCE, Pierri H, Wajngarten M. Acquisition of data: Rodrigues GHP, Gerbi CCS. Analysis and interpretation of the data: Rodrigues GHP, Gebara OCE, Wajngarten M. Statistical analysis: Rodrigues GHP, Gebara OCE. Writing of the manuscript: Rodrigues GHP, Wajngarten M. Critical revision of the manuscript for intellectual content: Gebara OCE, Pierri H, Wajngarten M. Potential Conflict of Interest No potential conflict of interest relevant to this article was reported. Sources of Funding There were no external funding sources for this study. Study Association This article is part of the thesis of Doctoral submitted by Giselle Helena de Paula Rodrigues, from Universidade de São Paulo - FMUSP/INCOR-SP. References 1. Najjar SS, Scuteri A, Lakatta EG. Arterial aging: is it an immutable cardiovascular risk factor? Hypertension. 2005;46(3):454-62. and persistent depressive symptoms: coronary psychosocial evaluation studies randomized controlled trial. Arch Intern Med. 2010;170(7):600-8. 2. Forette F. Preventing dependency: the longevity challenge. Bull Acad Natl Med. 2009;193(2):455-68. 12. Sousa RM, Ferri CP, Acosta D, Albanese E, Guerra M, Huang Y, et al. Contribution of chronic diseases to disability in elderly people in countries with low and middle incomes: a 10/66 Dementia Research Group population-based survey. Lancet. 2009;374(9704):1821-30. 3. Paixão Jr CM, Reichenheim ME. Uma revisão sobre instrumentos de avaliação do estado funcional do idoso. Cad Saúde Pública. 2005;21(1):7-19. 4. Alves TC, Rays J, Fráguas R Jr, Wajngarten M, Meneghetti JC, Prando S, et al. Localized cerebral blood flow reductions in patients with heart failure: a study using 99mTc-HMPAO SPECT. J Neuroimaging. 2005;15(2):150-6. 5. de Toledo Ferraz Alves TC, Ferreira LK, Wajngarten M, Busatto GF.J Cardiac disorders as risk factors for Alzheimer’s disease. Alzheimer Dis. 2010;20(3):749-63. 6. Alves TC, Rays J, Fráguas R Jr, Wajngarten M, Telles RM, Duran FL, et al. Association between major depressive symptoms in heart failure and impaired regional cerebral blood flow in the medial temporal region: a study using 99m Tc-HMPAO single photon emission computerized tomography (SPECT). Psychol Med. 2006;36(5):597-608. 7. Vaccarino V, Votaw J, Faber T, Veledar E, Murrah NV, Jones LR, et al. Major depression and coronary flow reserve detected by positron emission tomography. Arch Intern Med. 2009;169(18):1668-76. 8. Prince M, Patel V, Saxena S, Maj M, Maselko J, Phillips MR, et al. No health without mental health. Lancet. 2007;370(9590):859-77. 9. Instituto Brasileiro de Geografia e Estatística (IBGE). Síntese de indicadores sociais. uma análise das condições de vida da população brasileira. Rio de Janeiro; 2010. 10. Nützer J, Katon W, Callahan CM, Williams JW Jr, Hunkeler E, Harpole L, et al; IMPACT Investigators. Improving Mood-Promoting Access to Collaborative Treatment. Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. JAMA. 2002;288(22):2836-45. 11. Davidson KW, Rieckmann N, Clemow L, Schwartz JE, Shimbo D, Medina V, et al. Enhanced depression care for patients with acute coronary syndrome 13. Weintraub WS, Spertus JA, Kolm P, Maron DJ, Zhang Z, Jurkovitz C, et al; COURAGE Trial Research Group, Mancini GB. Effect of PCI on quality of life in patients with stable coronary disease. N Engl J Med. 2008;359(7):677-87. 14. Gottlieb SS, Kop WJ, Ellis SJ, Binkley P, Howlett J, O’Connor C, et al; HFACTION Investigators. Relation of depression to severity of illness in heart failure (from Heart Failure and a Controlled Trial Investigating Outcomes of Exercise Training (HF-ACTION). Am J Cardiol. 2009;103(9):1285-9. 15. Scott IA, Guyatt GH. Cautionary tales in the interpretation of clinical studies involving older persons. Arch Intern Med. 2010;170(7):587-95. Erratum in: Arch Intern Med. 2010;170(11):927. 16. O’Connor CM, Jiang W, Kuchibhatla M, Silva SG, Cuffe MS, Callwood DD, et al; SADHART-CHF Investigators. Safety and efficacy of sertraline for depression in patients with heart failure: results of the SADHART-CHF (Sertraline Against Depression and Heart Disease in Chronic Heart Failure) trial. J Am Coll Cardiol. 2010;56(9):692-9. 17. Fries JF, Spitz PW, Young DY. The dimensions of health outcomes: the health assessment questionnaire, disability and pain scales. J Rheumatol. 1982;9(5):789-93. 18. Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care.1992;30(6):473-83. 19. Spitzer RL, Williams JB, Kroenke K, Linzer M, deGruy FV 3rd, Hahn SR, et al. Utility of a new procedure for diagnosing mental disorders in primary care: The PRIME-MD 1000 Study. JAMA. 1994;272(22):1749-56. 20. Folstein MF, Folstein SE, McHugh PR. “Mini-Mental State”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189-98. Arq Bras Cardiol. 2015; 104(6):443-449 448 Rodrigues et al. Depression in elderly patients with cardiovascular diseases Original Article 21. An PG, Rabatin JS, Manwell LB, Linzer M, Brown RL, Schwartz MD; MEMO Investigators. Burden of difficult encounters in primary care: data from the minimizing error, maximizing outcomes study. Arch Intern Med. 2009;169(4):410-4. 22. Boyd CM, Darer J, Boult C, Fried LP, Boult L, Wu AW. Clinical practice guidelines and quality of care for older patients with multiple comorbid diseases: implications for pay for performance. JAMA. 2005;294(6):716-24. 23. Mezuk B, Gallo JJ. Depression and medical illness in late life: race, resources, and stress. In: Lavretsky H, Sajatovic M, Reynolds CF. (editors). Late-life mood disorders. Oxford: Oxford University Press; 2013. p. 270-94. 24. Evans DL, Charney DS, Lewis L, Golden RN, Gorman JM, Krishnan KR, et al. Mood disorders in the medically ill: scientific review and recommendations. Biol Psychiatry. 2005;58(3):175-89. 25. Ciechanowski PS, Katon WJ, Russo JE. Depression and diabetes: impact of depressive symptoms on adherence, function, and costs. Arch Intern Med. 2000;160(21):3278-85. 26. Freedland KE, Carney RM, Skala JA. Depression and smoking in coronary heart disease. Psychosom Med. 2005;67 Suppl 1:S42-6. 27. Alexopoulos GS, Meyers BS, Young RC, Kalayam B, Kakuma T, Gabrielle M, et al. Executive dysfunction and long-term outcomes of geriatric depression. Arch Gen Psychiatry. 2000;57(3):285-90. 28. Murray CJ, Lopez AD. The global burden of disease: a comprehensive assessment of mortality and disability from diseases, injuries, and risk factors in 1990 and projected to 2020. Cambridge (MA): Harvard University Press; 1996. 29. Harpole LH, Williams JW Jr, Olsen MK, Stechuchak KM, Oddone E, Callahan CM, et al. Improving depression outcomes in older adults with comorbid medical illness. Gen Hosp Psychiatry. 2005;27(1):4-12. 30. Centers for Disease Control and Prevention (CDC). Current depression among adults. United States, 2006 and 2008. MMWR Morb Mortal Wkly Rep. 2010;59(38):1229-35. 31. Strine TW, Chapman DP, Kobau R, Balluz L, Mokdad AH. Depression, anxiety, and physical impairments and quality of life in the U.S. noninstitutionalized population. Psychiatr Serv. 2004;55(12):1408-13. 449 Arq Bras Cardiol. 2015; 104(6):443-449 32. Byers AL, Yaffe K, Covinsky KE, Friedman MB, Bruce ML. High occurrence of mood and anxiety disorders among older adults: the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2010;67(5):489-96. 33. Collerton J, Davies K, Jagger C, Kingston A, Bond J, Eccles MP, et al. Health and disease in 85 year olds: baseline findings from the Newcastle 85+ cohort study. BMJ. 2009;399:b4904. 34. Murabito JM, Pencina MJ, Zhu L, Kelly-Hayes M, Shrader P, D’Agostino RB Sr. Temporal trends in self-reported functional limitations and physical disability among the community-dwelling elderly population: the Framingham heart study. Am J Public Health. 2008;98(7):1256-62. 35. Manton KG. Recent declines in chronic disability in the elderly U.S. population: risk factors and future dynamics. Annu Rev Public Health. 2008;29:91-113. 36. Weintraub WS, Spertus JA, Kolm P, Maron DJ, Zhang Z, Jurkovitz C, et al; COURAGE Trial Research Group, Mancini GB. Effect of PCI on quality of life in patients with stable coronary disease. N Engl J Med. 2008;359(7):677-87. 37. Mark DB, Pan W, Clapp-Channing NE, Anstrom KJ, Ross JR, Fox RS, et al. Quality of life after late invasive therapy for occluded arteries. N Engl J Med. 2009;360(8):774-83. 38. Gottlieb SS, Kop WJ, Ellis SJ, Binkley P, Howlett J, O’Connor C, et al; HFACTION Investigators. Relation of depression to severity of illness in heart failure (from Heart Failure And a Controlled Trial Investigating Outcomes of Exercise Training [HF-ACTION). Am J Cardiol. 2009;103(9):1285-9. 39. Reuben DB. Medical care for the final years of life: “when you’re 83, it’s not going to be 20 years”. JAMA. 2009;302(24):2686-94. 40. Lichtman JH, Bigger JT Jr, Blumenthal JA, Frasure-Smith N, Kaufmann PG, Lespérance F, et al; American Heart Association Prevention Committee of the Council on Cardiovascular Nursing; American Heart Association Council on Clinical Cardiology; American Heart Association Council on Epidemiology and Prevention; American Heart Association Interdisciplinary Council on Quality of Care and Outcomes Research; American Psychiatric Association. Depression and coronary heart disease: recommendations for screening, referral, and treatment: a science advisory from the American Heart Association Prevention Committee of the Council on Cardiovascular Nursing, Council on Clinical Cardiology, Council on Epidemiology and Prevention, and Interdisciplinary Council on Quality of Care and Outcomes Research: endorsed by the American Psychiatric Association. Circulation. 2008;118(17):1768-75. Back to the Cover Original Article Assessment of Autonomic Function by Phase Rectification of RRInterval Histogram Analysis in Chagas Disease Olivassé Nasario-Junior1, Paulo Roberto Benchimol-Barbosa1,3, Roberto Coury Pedrosa2, Jurandir Nadal1 Programa de Engenharia Biomédica – COPPE/UFRJ1; Hospital Universitário Clementino Fraga Filho – UFRJ2; Hospital Universitário Pedro Ernesto – UERJ3, Rio de Janeiro, RJ – Brazil Abstract Background: In chronic Chagas disease (ChD), impairment of cardiac autonomic function bears prognostic implications. Phase‑rectification of RR-interval series isolates the sympathetic, acceleration phase (AC) and parasympathetic, deceleration phase (DC) influences on cardiac autonomic modulation. Objective: This study investigated heart rate variability (HRV) as a function of RR-interval to assess autonomic function in healthy and ChD subjects. Methods: Control (n = 20) and ChD (n = 20) groups were studied. All underwent 60-min head-up tilt table test under ECG recording. Histogram of RR-interval series was calculated, with 100 ms class, ranging from 600–1100 ms. In each class, mean RR-intervals (MNN) and root-mean-squared difference (RMSNN) of consecutive normal RR-intervals that suited a particular class were calculated. Average of all RMSNN values in each class was analyzed as function of MNN, in the whole series (RMSNNT), and in AC (RMSNNAC) and DC (RMSNNDC) phases. Slopes of linear regression lines were compared between groups using Student t-test. Correlation coefficients were tested before comparisons. RMSNN was log-transformed. (α < 0.05). Results: Correlation coefficient was significant in all regressions (p < 0.05). In the control group, RMSNNT, RMSNNAC, and RMSNNDC significantly increased linearly with MNN (p < 0.05). In ChD, only RMSNNAC showed significant increase as a function of MNN, whereas RMSNNT and RMSNNDC did not. Conclusion: HRV increases in proportion with the RR-interval in healthy subjects. This behavior is lost in ChD, particularly in the DC phase, indicating cardiac vagal incompetence. (Arq Bras Cardiol. 2015; 104(6):450-456) Keywords: Chagas Disease; Chagas Cardiomyopathy; Heart Rate; Organ Dysfunction Scores; Sympathetic Nervous System; Charts; Statistics as Topic. Introduction Chagas disease (ChD) is a major cause of cardiomyopathy in Latin America. It has been estimated that 8–11 million people are currently infected by Trypanosoma cruzi worldwide, potentially becoming a significant healthcarerelated problem in Europe and in the United States due to migration1,2. In chronic ChD, autonomic dysfunction has been associated with impairment of both parasympathetic and sympathetic limbs3-5, with prognostic implications6. Heart rate variability (HRV) analysis is a powerful and simple method for assessing autonomic influence on the sinus node and risk stratification in many cardiac diseases7,8. On routine clinical assessment, parameters in time domain are usually estimated during a predefined time sequence Mailing Address: Paulo Roberto Benchimol Barbosa • Universidade do Estado do Rio de Janeiro. Boulevard Vinte e Oito de Setembro, 77. Térreo. Sala da Coordenadoria de Assistência Médica, Vila Izabel. Postal Code 20551-030, Rio de Janeiro, RJ – Brazil E-mail: [email protected], [email protected] Manuscript received November 10, 2014; revised manuscript January 24, 2015; accepted January 26, 2015. DOI: 10.5935/abc.20150032 450 of normal-to-normal RR-intervals. Among the parameters usually employed, root-mean-squared difference (RMSNN) is particularly useful, as it expresses the amount of energy associated with data variability7. However, none of these indexes distinguish between vagal and sympathetic effects. Recently, an approximate isolation of distinct autonomic contribution on heart rate (HR) has been possible by assessing the capability of RR-interval series to accelerate (AC) or decelerate (DC), representing sympathetic and parasympathetic contributions, respectively. To further accomplish this task, it was initially detected that if a particular RR-interval changed relative to the previous one, the corresponding RR-interval was separated in a new series9,10. In healthy subjects, it has been demonstrated that HRV indices tended to increase as RR-intervals enlarged11,12. On the other hand, this relationship may be lost during a disease state and may further precipitate some forms of ventricular arrhythmia, such as long QT syndrome, and ischemic cardiomyopathy13. Thus, the aims of this study were (i) to assess RMSNN index on AC and DC phases of RR-interval series in order to isolate sympathetic and parasympathetic effects, respectively, and (ii) to correlate RMSNN and mean RR-intervals (MNN) to assess heart rate dependence of autonomic modulation index in chronic ChD. Nasario-Junior et al. Phase RR-interval histogram in Chagas disease Original Article Methods Study population ECG signals were extracted from an existing high resolution ECG database14. The study protocol was approved by the Hospital Universitário Clementino Fraga Filho Ethics Committee and informed consent was obtained from each volunteer. A group of gender-matched 20 healthy sedentary participants [Control group, (mean age ± SD) 51.1 ± 17.6 years] and 20 subjects with chronic ChD (Chagas group, 55 ± 10.3 years) were studied. Chronic ChD subjects were enrolled to the study based on spontaneous demand. Due to the exploratory nature of the study, the number of participants was arbitrarily defined and equally distributed between groups. According to surface ECG data analysis, in ChD group, seven had normal ECG. Among 13 subjects with abnormal ECG, nine showed left atrial overload based on Morris criteria, nine had left anterior fascicular block, nine had complete right bundle branch block and one had first degree AV block. Two subjects showed isolated supraventricular tachycardia and four showed isolated ventricular premature beats. Additionally, all participants met the following criteria: (i) no intake of nutritional supplements or potential ergogenic aids of any type (e.g., exogenous anabolic androgenic steroids); (ii) non-smokers; (iii) normal blood pressure; (iv) non-diabetic; (v) no history of alcohol addiction; (vi) no history of thyroid dysfunction; and (vii) not taking medications that affect cardiac electrical properties and/or autonomic function. Signal acquisition and processing All subjects underwent 60-min head-up tilt test (HUTT) under modified Westminster protocol15 at 70° and continuous high-resolution ECG recording in an acclimatized (27°C) and quiet room. Subjects were oriented to withhold exercise for 48 h before the exam, fast for at least 4 h, and avoid taking caffeine-containing beverages on the day of the exam. Before ECG recording, subjects remained in the supine position for at least 5 min in order to reduce orthostatic autonomic memory on spontaneous RR-interval variations16,17. ECG signal acquisition periods were characterized by 10 min of supine rest followed by 40-min HUTT and another 10-min supine rest. Accordingly, HRV was expected to be influenced by two predominant autonomic inputs: parasympathetic input during supine rest, and sympathetic input during tilt7. High-resolution ECG signals were acquired using modified bipolar Frank XYZ orthogonal leads18. Digital data were processed with custom-made pattern recognition software19-21. The analysis of the HRV was done by extraction of the normal RR-intervals, after detection of the QRS complex using a low‑pass triangular filter. Any RR-interval that exhibited more than 20% change from the previous RR-interval were excluded, as they were likely to be related to measurement noise or ectopic beats21,22. Instantaneous RR-interval analysis The RR-interval histogram was constructed for each individual series and split into 100-ms width classes, ranging from 600–1100 ms. For each histogram class, and respective to each RR-interval series, mean (MNN) and root-mean-square diference (RMSNN) of consecutive normal RR-intervals suiting a particular class were calculated. Only the pairs of consecutive normal RR-intervals for individual series that were inside a particular class of the RR histogram were analyzed together. For a particular histogram class (class) of the ith series, containing Ni,class RR-intervals, calculation of the mean (Mi,class) and the root-mean-squared difference (RMSi,class) of the normal RR-intervals was performed as follows: (1) Ni,classe Mi,classe = Σ K = 1 RRk Ni,classe (2) Ni,classe RMSi,classe = Σk = 1 (RRk - RRk - 1)2 Ni,classe For each histogram, classes with intervals of 30 or less were excluded to avoid bias due to lack of statistical precision. The values of the variables M i,class and RMS i,class were aggregated to the respective histogram class. The ensemble mean (MNNclass) and root-mean-squared difference (RMSNNclass) of RR-intervals for each histogram class, weighed by the respective degree‑of‑freedom (ηi,class), were calculated according to: (3) 20 MNNclasse = +1 Σ i = 1Mi,classe . (ηi,classe ) 20 +1 Σ i = 1(ηi,classe ) (4) RMSNNclasse = 20 2 +1 Σ i = 1(RMSi,classe) . (ηi,classe ) 20 Σ i = 1(ηi,classe ) +1 Instantaneous AC and DC analysis RR-interval histograms in AC and DC phases were also built following the procedures described above; RMSNN in AC (RMSNNAC) and RMSNN in DC (RMSNNDC) phases were calculated accordingly. To further accomplish this task, data points were initially isolated as acceleration (AC) or deceleration (DC) capacities. If a particular RR-interval increased relative to the previous one, a DC interval occurred. As the instantaneous RR‑interval increased, it represented a parasympathetic action (DC; lozenge symbols in Figure 1). Conversely, a sympathetic effect on the RR-interval was represented whenever the RR‑interval decreased relative to the previous one, and AC interval was defined (AC; represented by circle symbols in Figure 1). Arq Bras Cardiol. 2015; 104(6):450-456 451 Nasario-Junior et al. Phase RR-interval histogram in Chagas disease Original Article Acceleration RR interval RR-intervals histogram RR-intervals (ms) 1000 (n) Deceleration RR interval 900 800 700 600 3 8 13 18 Beat index (n) 23 Figure 1 – Deceleration and Acceleration anchor points are represented in RR-intervals samples that were derived from an ECG recording. RR-interval histogram is represented on the right. Statistical analysis The RMSNN and MNN of each subject were pooled and averaged on a class-by-class basis in the control and ChD groups. RMSNN was analyzed in the whole series (RMSNN T) as well as in the AC and DC phases. Regression lines were analyzed and angular coefficient was compared between ChD and control groups using non‑paired Student’s t-test. Correlation coefficients (r) were tested before each test. Due to strong asymmetry in their probability density functions, the RMSNN variables were log-transformed before analysis to fit appropriately in the parametric statistical analysis. All tests were considered significant at α level < 0.05. Results Table 1 shows the linear correlation coefficient (r) and respective angular coefficient (slope) of the regression line between MNN and other each pooled variable. The r-values were significant in all regression lines (p < 0.05). The log-transformed pooled RMSNN (T, AC, and DC), as a function of pooled MNN, were presented for each group (Figure 2). RMSNNAC were significantly different in both groups, whereas, in the control group, RMSNNT, RMSNNAC, and RMSNN DC significantly increased proportionally to MNN (p < 0.05); in the ChD group, only RMSNNAC showed significant increase as a function of MNN, whereas RMSNNT and RMSNNDC did not. Based on the total number of RR-intervals suiting a particular histogram class, the percent value (mean ± SD) of RR-interval pairs rejected as not pertaining to the same histogram class was 31.7% ± 21.7% for the control group 452 Arq Bras Cardiol. 2015; 104(6):450-456 and 27.0% ± 14.7% for ChD. Figure 3 shows histograms of RR-interval pairs for each group according to the AC and DC phases, respectively. Discussion Cardiac autonomic dysfunction, characterized mainly by parasympathetic depression, is an important aspect of human ChD3-5. The observation of marked autonomic dysfunction in association with normality of most ventricular echocardiographic variables suggested that there was no clear relationship between autonomic and ventricular function23. Additionally, autonomic dysfunction seemed to be a primary phenomenon, preceding ventricular mechanical changes in chronic ChD evolution6,24,25. In a previous study22, DC index adaptation was proposed to measure cardiac vagal modulation by a phase-rectified signal averaging (PRSA) procedure10,11 that was effective in distinguishing athletes from sedentary healthy volunteers. It was hypothesized that depending on vagal stimulus intensity, the rate of ascent of the RR-interval series would change accordingly, determining slope variation. Thus, the strongest vagal stimulus determined the steepest slope and vice-versa, potentially affecting the DC value. Although PRSA has been originally developed to risk-stratify subjects post myocardial infarction10, its application in assessing physiological conditions that are strongly related to vagal activity modulation has been shown to be highly pertinent and feasible as well. In the present study, the behavior of RR-intervals was analyzed by grouping time domain RMSNN parameters calculated at different histogram classes. This procedure Nasario-Junior et al. Phase RR-interval histogram in Chagas disease Original Article Table 1 – Correlation of parameters: MNN vs. Variables Ln RMSNNT Group Control ChD Ln RMSNNAC Ln RMSNNDC r 0.96 * 0.99 * 0.99 * slope 0.0011 ** 0.0012 0.0008 ** r -0.55 * 0.96 * -0.75 * slope -0.0002 0.0010 -0.0003 (*) p < 0.05; (**) p < 0.05 for intergroup comparison. Log-transformed RMSNNT, RMSNNAC e RMSNNDC In the control group, HRV (RMSNN T, RMSNN AC and RMSNNDC) was strongly dependent on the instantaneous RR-interval, confirming the previous findings of BenchimolBarbosa et al.13. In the physiological range of RR-interval variation (600–1100 ms), RMSNN was lower during headup tilt and higher during supine position, representing sympathetic and parasympathetic autonomic influences on HRV, respectively. Moreover, it was notable that RR‑interval variation had average inter-beat “jumps” that were proportional to the average RR-intervals (Figure 2). This relation was also represented by a strong linear dependence between RMSNN and MNN (r > 0.96). On the other hand, in the ChD group, only RMSNNAC showed significant increase as a function of MNN (p < 0.05), which assessed the isolated contribution of sympathetic nervous system on HRV. RMSNNDC, which assessed the isolated parasympathetic influence, not only had its mean value lower than the control group, but also showed no variations with changes in mean RR-interval. These findings indicate that not only vagal modulation was reduced in this population, but also the ability of parasympathetic system to modulate RR-intervals at different heart rates throughout a wide range of RR-intervals analyzed. We named this later observation as parasympathetic incompetence. This study has its limitations, including a relatively small sample size and application of the method using two physiologically well-defined groups. Although the groups were not matched by age, both had their mean age above 40 years. Assessment of left ventricular systolic function was not carried out in the present study; however, in Chagas disease, there was no clear relationship between autonomic and ventricular function24. Further studies are needed to confirm present findings. Ln RMSNNT (Ln ms) 3.5 3.0 2.5 4.0 Ln RMSNNAC (Ln ms) The essential point of this study was to stratify HR and HRV according to instantaneous RR-interval difference using a parameter that expresses energy (RMSNN) from all series and to isolate sympathetic and parasympathetic contributions. Also, it introduced novel information that represents insights into the dependence of autonomic modulation on heart rate in a population of chronic ChD. 4.0 3.5 3.0 2.5 4.0 Ln RMSNNDC (Ln ms) made it possible to cluster beats under the influence of similar instantaneous time factors. Additionally, assessment of the capacity of RR-interval series to accelerate or decelerate enabled the isolation of both sympathetic (AC phase) and parasympathetic (DC phase) contributions on the RR-intervals series. 3.5 3.0 2.5 (a) Control slope: 0.0011 Chagas slope: -0.0002 p < 0.05 600 700 800 900 1000 1100 (b) Control slope: 0.0012 Chagas slope: 0.0010 p = NS 600 700 800 900 1000 1100 (c) Control slope: 0.008 Chagas slope: -0.0003 p < 0.05 600 700 800 900 1000 1100 IM (ms) Figure 2 – Comparison of control and ChD groups in terms of logtransformed of pooled RMSNNT (a), RMSNNAC (b), and RMSNNDC (c) as a function of pooled RR-intervals (MNN), and the respective angular coefficient (slope) of regression line. p value refers to Student’s t-test significance for comparing slopes. Correlation was significant for all regression lines. (See text for details) Arq Bras Cardiol. 2015; 104(6):450-456 453 Nasario-Junior et al. Phase RR-interval histogram in Chagas disease Original Article (a) Acceleration phase Total 8000 6000 Control Chagas 4000 2000 0 400 500 600 700 800 900 1000 1100 1200 1300 1400 (b) Decelaration phase 8000 Total 6000 Control Chagas 4000 2000 0 400 500 600 700 800 900 1000 1100 1200 1300 1400 RR-interval classes (ms) Figure 3 – RR-interval pairs histograms assessed for each group and phase: acceleration phase (a) and deceleration phase (b). Conclusion In subjects with chronic Chagas disease, a significant reduction of autonomic modulation of the heart is observed throughout a wide physiological range of RR-intervals. Additionally, in healthy sedentary subjects, RMSNN increases proportionally with RR-interval. This relationship is not observed in chronic Chagas disease, particularly during parasympathetic stimulation phase, indicating parasympathetic incompetence in modulating heart rate variation in this scenario. Acknowledgements This work was partially supported by Fundação Carlos Chagas Filho de Amparo à Pesquisa do Estado do Rio de Janeiro (FAPERJ) and the Brazilian Agencies CNPq and CAPES. We wish to thank Dr. Aline Medeiros for her dedication in the acquisition of ECG data of the patients. Author contributions Conception and design of the research:Nasario-Junior O, Benchimol-Barbosa PR. Acquisition of data: Pedrosa 454 Arq Bras Cardiol. 2015; 104(6):450-456 RC. Analysis and interpretation of the data: Nasario-Junior O, Benchimol-Barbosa PR, Nadal J. Statistical analysis: Nasario-Junior O, Benchimol-Barbosa PR, Nadal J. Obtaining financing: Pedrosa RC, Nadal J. Writing of the manuscript: Nasario-Junior O, Benchimol-Barbosa PR, Pedrosa RC, Nadal J. Critical revision of the manuscript for intellectual content: Nasario-Junior O, BenchimolBarbosa PR, Pedrosa RC, Nadal J. Supervision / as the major investigador:Nadal J. Potential Conflict of Interest No potential conflict of interest relevant to this article was reported. Sources of Funding This study was partially funded by FAPERJ, CNPq e CAPES. Study Association This study is not associated with any thesis or dissertation work. Nasario-Junior et al. Phase RR-interval histogram in Chagas disease Original Article References 1. Dias JC, Silveira AC, Schofield CJ. The impact of Chagas’ disease control in Latin America: a review. Mem Inst Oswaldo Cruz. 2002;97(5):603-12. 2. Guerri- Guttenberg RA, Grana DR, Ambrosio G, Milei J. Chagas cardiomyopathy: Europe is not spared! Eur Heart J. 2008;29(21):2587-91. 3. Gallo Junior L, Morelo Filho J, Maciel BC, Marin Neto JA, Martins LE, Lima Filho EC. Functional evaluation of sympathetic and parasympathetic system in Chagas’ disease using dynamic exercise. Cardiovasc Res. 1987;21(12):922-7. 4. Junqueira Junior LF, Beraldo PS, Chapadeiro E, Jesus PC. Cardiac autonomic dysfunction and neuroganglionitis in a rat model of chronic Chagas’ disease. Cardiovasc Res. 1992;26(4):314-9. 5. Dávila DF, Inglessis G, Mazzei de Dávila CA. Chagas’ heart disease and the autonomic nervous system. Int J Cardiol. 1998;66(2):123-7. 6. Benchimol-Barbosa PR, Tura BR, Barbosa EC, Kantharia BK. Utility of a novel risk score for prediction of ventricular tachycardia and cardiac death in chronic Chagas disease - the SEARCH-RIO study. Braz J Med Biol Res. 2013;46(11):974-84. 7. Heart rate variability. Standards of measurement, physiological interpretation, and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Eur Heart J. 1996;17(3):354-81. 8. Rajendra Acharya U, Paul Joseph K, Kannathal N, Lim CM, Suri JS. Heart rate variability: a review. Med Biol Eng Comput. 2006;44(12):1031-51. 9. Bauer A, Kantelhardt JW, Barthel P, Schneider R, Mäkikallio T, Ulm K, et al. Deceleration capacity of heart rate as a predictor of mortality after myocardial infarction: cohort study. Lancet. 2006;367(9523):1674-81. 14. Medeiros AS. Avaliação autonômica cardíaca em indivíduos com doença de Chagas sem disfunção ventricular empregando o teste de inclinação (TiltTest). [Tese]. Rio de Janeiro: Universidade Federal do Rio de Janeiro; 2008. 15. Bomfim AS, Benchimol-Barbosa PR, Barbosa EC, Boghossian SH, Ribeiro RL, Ginefra P. Teste de inclinação: fundamentos e aplicação clínica. Rev SOCERJ. 2004;17(4):243-50. 16. Lipsitz LA, Mietus J, Moody GB, Goldberger AL. Spectral characteristics of heart rate variability before and during postural tilt: relations to aging and risk of syncope. Circulation. 1990;81(6):1803-10. 17. Ryan SM, Goldberger AL, Ruthazer R, Mietus J, Lipsitz LA. Spectral analysis of heart rate dynamics in elderly persons with postprandial hypotension. Am J Cardiol. 1992;69(3):201-5. 18. Barbosa PR, Barbosa-Filho J, de Sá CA, Barbosa EC, Nadal J. Reduction of electromyographic noise in the signal-averaged electrocardiogram by spectral decomposition. IEEE Trans Biomed Eng. 2003;50(1):114-7. 19. Nasario-Junior O, Benchimol-Barbosa PR, Nadal J. Principal component analysis in high resolution electrocardiogram for risk stratification of sustained monomorphic ventricular tachycardia. Biomedical Signal Process Control. 2014;10:275-80. 20. Nasario-Junior O, Benchimol-Barbosa PR, Trevizani GA, Marocolo M, Nadal J. Effect of aerobic conditioning on ventricular activation: a principal components analysis approach to high-resolution electrocardiogram. Comput Biol Med. 2013;43(11):1920-6. 21. Nasario-Junior O, Benchimol-Barbosa PR, Nadal J. Refining the deceleration capacity index in phase-rectified signal averaging to assess physical conditioning level. J Electrocardiol. 2014; 47(3):306-10. 10. Bauer A, Kantelhardt JW, Bunde A, Bundec A, Barthela P, Schneider R, et al. Phase-rectified signal averaging detects quasi-periodicities in nonstationary data. Physica A. 2006;364:423-34. 22. Clifford GD, McSharry PE, Tarassenko L. Characterizing artifact in the normal human 24-hour RR time series to aid identification and artificial replication of circadian variations in human beat to beat heart rate using a simple threshold. Computers in Cardiology. 2002;29:129-32. 11. Merri M. QT variability. In: Moss AJ, Stern S (eds). Noninvasive electrocardiology: clinical aspects of Holter monitoring. London: Saunders WB; 1996. p. 421-43. 23. Ribeiro AL, Moraes RS, Ribeiro JP, Ferlin EL, Torres RM, Oliveira E, et al. Parasympathetic dysautonomia precedes left ventricular systolic dysfunction in Chagas disease. Am Heart J. 2001;141(2):260-5. 12. Benchimol-Barbosa PR, Barbosa-Filho J, Cordovil I, Nadal J. The effect of the instantaneous RR interval on the dynamic properties of the heart rate and the ventricular repolarization duration variability. Computers in Cardiology. 2000;27:821-4. 24. Vasconcelos DF, Junqueira LF Jr. Cardiac autonomic and ventricular mechanical functions in asymptomatic chronic Chagasic cardiomyopathy. Arq Bras Cardiol. 2012;98(2):111-9. 13. Pitzalis MV, Mastropasqua F, Massari F, Totaro P, Di Maggio M, Rizzon P. Holterguided identification of premature ventricular contractions susceptible to suppression by beta-blockers. Am Heart J. 1996;131(3):508-15. 25. Gerbi FC, Takahashi JT, Cardinalli-Neto A, Nogueira PR, Bestetti RB. Heart rate variability in the frequency domain in chronic Chagas disease: correlation of autonomic dysfunction with variables of daily clinical practice. Int J Cardiol. 2011;150(3):357-8. Arq Bras Cardiol. 2015; 104(6):450-456 455 Nasario-Junior et al. Phase RR-interval histogram in Chagas disease Original Article 456 Arq Bras Cardiol. 2015; 104(6):450-456 Back to the Cover Original Article Post-Acute Coronary Syndrome Alcohol Abuse: Prospective Evaluation in the ERICO Study Abner Morilha, Samuel Karagulian, Paulo A. Lotufo, Itamar S. Santos, Isabela M. Benseñor, Alessandra C. Goulart Centro de Pesquisa Clínica e Epidemiológica - Hospital Universitário, Universidade de São Paulo, São Paulo - Brazil Abstract Background: Some studies have indicated alcohol abuse as one of the contributors to the development of cardiovascular disease, particularly coronary heart disease. However, this relationship is controversial. Objective: To investigate the relationship between post-acute coronary syndrome (ACS) alcohol abuse in the Acute Coronary Syndrome Registry Strategy (ERICO Study). Methods: 146 participants from the ERICO Study answered structured questionnaires and underwent laboratory evaluations at baseline, 30 days and 180 days after ACS. The Alcohol Use Disorders Identification Test (AUDIT) was applied to assess harmful alcohol consumption in the 12 months preceding ACS (30 day-interview) and six months after that. Results: The frequencies of alcohol abuse were 24.7% and 21.1% in the 12 months preceding ACS and six months after that, respectively. The most significant cardiovascular risk factors associated with high-risk for alcohol abuse 30 days after the acute event were: male sex (88.9%), current smoking (52.8%) and hypertension (58.3%). Six months after the acute event, the most significant results were replicated in our logistic regression, for the association between alcohol abuse among younger individuals [35-44 year-old multivariate OR: 38.30 (95% CI: 1.44-1012.56) and 45-54 year-old multivariate OR: 10.10 (95% CI: 1.06-96.46)] and for smokers [current smokers multivariate OR: 51.09 (95% CI: 3.49-748.01) and past smokers multivariate OR: 40.29 (95% CI: 2.37-685.93)]. Conclusion: Individuals younger than 54 years and smokers showed a significant relation with harmful alcohol consumption, regardless of the ACS subtype. (Arq Bras Cardiol. 2015; 104(6):457-467) Keywords: Alcoholism; Acute Coronary Syndrome; Myocardial Infarction; Alcohol Drinking; Questionnaires. Introduction According to recent data from the World Health Organization (WHO), the prevalence of alcohol dependence can reach 12% of the adult population. The probability of alcohol dependence of subjects with any mental disorder can be at least two times greater than that of individuals without the disorder1. The burden is not equally distributed among the countries. Alcohol consumption is the leading risk factor for the burden of disease in developing countries and the third largest risk factor in developed countries1. It should be noted that drinking patterns have not only been linked to acute health outcomes, such as injuries2,3, but also to chronic diseases, such as coronary heart disease (CHD)4-7. In fact, some studies even indicate alcohol abuse as one of the contributors to the development of cardiovascular diseases (CVD), particularly CHD 4-9 . However, this Mailing Address: Alessandra C. Goulart • Av. Prof. Lineu Prestes 2565, Cidade Universitária, Butantã. Postal Code 05508-000, São Paulo, SP – Brazil E-mail: [email protected]; [email protected]. Manuscript received July 14 , 2014; revised manuscript November 18, 2014; accepted December 26, 2014. DOI: 10.5935/abc.20150038 457 relationship is controversial 8. Although some beneficial effects of moderate alcohol intake have been described, it can become a risk factor for CHD if the alcohol consumption pattern is characterized as “binge drinking or heavy episodic drinking”, which is defined as more than five drinks for men and four drinks for women in just one occasion1,6-9. In developing countries, such as Brazil, alcohol is also considered a risk factor that contributes most to the burden of diseases, such as cirrhosis of the liver and several types of cancer1. Therefore, we aimed to evaluate the hazardous and harmful uses of alcohol and its dependence symptoms 30 days and 180 days after an acute coronary event among participants from the ERICO study (Acute Coronary Syndrome Registry Strategy)10. Materials and Methods Study design and population This sub-study assessed harmful alcohol consumption, hazardous alcohol consumption and dependence symptoms in a subsample of the ERICO study, a prospective cohort study, ongoing since 2009, which included potential participants with ACS admitted to the São Paulo University-affiliated hospital (HU-USP) in the city of São Paulo, Brazil10. Morilha et al. Alcohol abuse and acute coronary syndrome Original Article After signing the Informed Consent Form, patients with confirmed medical diagnosis of ACS [ST-elevation myocardial infarction (STEMI), non-ST-elevation acute myocardial infarction (NSTEMI) or unstable angina (UA)] were invited to participate in our sub-study 30 days after the acute event. The eligibility criteria were: age ≥ 18 years, confirmed diagnosis of ACS, and ability to understand and speak Portuguese. The usual treatment for ACS has not changed and the procedures followed were in accordance with the ethical standards approved by the HU-USP Institutional Review Board. Exclusion criteria were based on a Psychological Screening Questionnaire built on Structured Clinical Interview for DSM Disorders (SCID - I) 11 to identify individuals with psychotic, schizophrenia or bipolar disorders, and on a test based on the Mini-Mental State Exam (MMSE)12 to exclude those with cognitive impairment or dementia 30 days after the acute event. 30- and 180-day follow-up All participants who fulfilled the eligibility criteria answered structured questionnaires and underwent clinical and laboratory evaluations, including depression evaluation using the Brazilian-Portuguese version of the Patient Health Questionnaire (PHQ-9), which is composed of nine questions that assess depressive mood and anhedonia based on the Diagnostic and Statistical Manual of Mental Disorders fourth edition (DSM-IV). The PHQ-9 scores each of the nine DSM-IV criteria as “0” (not at all) to “3” (nearly every day), the total score ranging from 0 to 27, and, in this study, PHQ-9 was applied at baseline, and 30 and 180 days after ACS13,14. In addition, hazardous and harmful alcohol consumption and dependence symptoms were assessed by using the Alcohol Use Disorders Identification Test (AUDIT) in a personal and in a telephone interview, 30 and 180 days after ACS, respectively15. Of note, 30 days after ACS, participants were asked about alcohol abuse during the last 12 months, and, during the 180-day interview, they were asked about changes in their alcohol behavior six months after ACS. Acute coronary syndrome definition Myocardial infarction (MI) was defined as the presence of symptoms consistent with cardiac ischemia in the 24 hours preceding hospital presentation and troponin I levels above the 99th percentile with a test-specific coefficient of variation < 10%16,17. STEMI was defined as the presence of MI criteria plus one of the following: (a) persistent ST-segment elevation ≥ 1 mm in two contiguous electrocardiographic leads or (b) the presence of a new or presumably new left bundle branch block. NSTEMI was defined as the presence of MI criteria, but not of STEMI. The UA diagnosis required the presence of symptoms consistent with cardiac ischemia 24 hours prior to hospital admission, absence of MI criteria and at least one of the following: (a) history of CHD; (b) positive coronary disease stratification test (invasive or non‑invasive); (c) transient ST‑segment changes ≥ 0.5 mm in two contiguous leads, new T-wave inversion ≥1 mm, and/or pseudonormalization of previously inverted T waves; (d) troponin I >0.4 ng/mL (which guarantees a troponin I level above the 99th percentile regardless of the kit used); or (e) diagnostic concordance between two independent doctors. Alcohol abuse definition Based on the AUDIT score that ranges from 1 to 40, the following cutoff points were considered for main analyses: ≤ 7, low-risk drinking; and ≥ 8, high-risk alcohol abuse18-20. In secondary analysis, the following three AUDIT domains were also evaluated: a) Hazardous alcohol use (1-7 points) - characterized as a pattern that increases the risk of harmful consequences for the user and/or others. These patterns are of public health significance despite the absence of any current disorder in the user; b)Harmful alcohol use (8-19 points) - refers to alcohol intake that might result in consequences for physical and mental health. Some would also consider the social consequences of the harm caused by alcohol; c) Alcohol dependence symptoms (≥ 20 points) characterized by a cluster of behavioral, cognitive and physiological phenomena, which may develop after repeated alcohol use. Typically, these phenomena include a strong desire to consume alcohol, impaired control of its use, persistent drinking, despite harmful consequences, a higher priority given to consumption than to other activities and obligations, increased substance tolerance and physical withdrawal reaction when the substance use is discontinued18-20. Two trained psychologists administered all questionnaires during the follow-up. Statistical analysis The participants’ baseline characteristics, including ACS subtypes, were described according to the alcohol abuse symptoms assessed by using the AUDIT questionnaire, with the following cutoff points suggested in the literature19-21: ≤ 7, low-risk drinking; and ≥ 8, high-risk alcohol abuse18-20. In addition, the baseline characteristics were classified according to the AUDIT domains (hazardous alcohol use, harmful alcohol use and alcohol dependence symptoms). Categorical variables were analyzed by using chi‑square test, and continuous variables, by using Student t or Mann‑Whitney test, according to continuous variables distribution. Additionally, we performed multivariate logistic regression adjusted to potential confounders (or those with a p-value < 0.2 on univariate analysis) identified at 30 days to evaluate the odds ratios (OR) with 95% confidence intervals (CI) for the possible association of some classical cardiovascular risk factors (CVRF) with alcohol abuse 180 days after the acute event. All analyses with a p-value < 0.05 were considered statistically significant. The SPSS software, version 19.0, was used to perform all statistical analyses. Arq Bras Cardiol. 2015; 104(6):457-467 458 Morilha et al. Alcohol abuse and acute coronary syndrome Original Article Results Case series Of 225 patients with a confirmed diagnosis of ACS (STEMI, NSTEMI or UA) and included in the main study, 146 (64.9%) were enrolled in the present sub-study. At 180 days, 142 (63%) were evaluated, because four died during the period. The reasons for no inclusion in this study were early death (16/225, 7.1%) within 30 days and exceeded time limit for the interview (63/209, 30.1%). Evaluation of alcohol abuse during follow-up AUDIT score was almost the same (3.8 points) for the entire sample and by sex (men: 5.1 vs. women: 1.6). The most significant results observed at 30 days were replicated in our logistic regression after 180 days, for the association between alcohol abuse among younger individuals [35‑44 year‑old multivariate OR: 38.30 (95% CI: 1.44-1012.56) and 45‑54 year‑old multivariate OR: 10.10 (95% CI: 1.06‑96.46)] and for smokers [current smokers multivariate OR: 51.09 (95% CI: 3.49-748.01) and past smokers multivariate OR: 40.29 (95% CI: 2.37-685.93)] (Table 3). Depression versus alcohol abuse during follow-up In this sub-sample, no statistical association was found between depression and alcohol use after multivariate analysis during the follow-up. 30-day follow-up The baseline characteristics of all 146 participants in the main study were described according to alcohol abuse symptoms assessed by using the information obtained from AUDIT (Table 1) in a personal interview 30 days after ACS. The frequency of alcohol abuse was 24.7% in the first period, reflecting the alcohol abuse in the 12 months preceding ACS. The overall mean AUDIT score was 4.8 points, being higher in men as compared to women (6.3 vs. 2.0, p ≤ 0.001). In addition, the frequency of alcohol abuse (score ≥ 8) was higher among men as compared to women (88.9% vs. 11.1%, p = 0.001) and among current smokers as compared to past or non-smokers (52.8% vs. 38.9% vs. 8.3%, p = 0.004) and patients with hypertension (58.3%, p = 0.03) (Table 1). Interestingly, the sample with alcohol abuse suggested by AUDIT showed a statistically lower frequency of classical CVRF, such as dyslipidemia, diabetes and sedentary lifestyle, as compared to individuals without alcohol abuse, but with no statistical significance (Table 1). The frequency of alcohol abuse did not differ in the ACS subtypes during follow-up (Figure 1). At 30 days, we also found statistically significant associations between some sociodemographic and cardiovascular risk factors and each item of the AUDIT domains, except for questions 7 (“Guilt after drinking”) and 8 (“Blackouts”) in the “Harmful alcohol use” domain. In general, high frequencies of positive answers were found among men and smokers (Table 2). Interestingly, we found higher frequencies of positive answers for question 5 (“Increased salience of drinking”) from the “Dependence symptoms” domain among those who had STEMI as compared to the other ACS subtypes (Table 2). Further, we found higher frequencies of positive answers among participants who had hypertension, diabetes, dyslipidemia and a sedentary lifestyle as compared to those without these comorbidities in the three domains, particularly in the “Dependence symptoms” and the “Harmful alcohol use” domains (Table 2). 180-day follow-up Six months after the acute event, we observed a slight reduction in the alcohol abuse frequency, which was 21.1% among the 142 survivors by the end of the follow-up. In addition, the mean 459 Arq Bras Cardiol. 2015; 104(6):457-467 Sensitivity analyses In additional analyses, we compared ERICO participants who were excluded (79) or did not complete the entire follow‑up (four deaths between 30 days and 180 days after the acute event) with those who completed the 180-day follow‑up (142) in this sub-study. Individuals who were followed up for six months after an acute event in this sub‑study had a higher educational level (9-11 years of formal education: 59.9% vs. 56.1, p = 0.04), were mostly white or of mixed self-reported heritage (96.4% vs. 89%, p = 0.03) and had a more sedentary lifestyle (63.8% vs. 81.5%, p = 0.006) than those who were not followed‑up (Table 4). Moreover, comparing ERICO participants included in this sub-study of alcohol abuse (146) with the ERICO population (820), we found that the former had a higher educational level (≥ 11 years of formal education: 12.3% vs. 6.8%, p=0.02) and most were married (69.2% vs. 59.6%, p = 0.03). In addition, their frequencies of diabetes (30.8% vs. 41.2%, p=0.02) and of sedentary lifestyle (64.8% vs. 73.0%, p = 0.05) were lower than those found in the ERICO population. Finally, a high proportion of STEMI cases (36.3% vs. 26.5%, p = 0.02) was detected in this sub-study (Table 5). Discussion This sub-study showed that three of ten patients were at high risk for alcohol abuse. The alcohol abuse frequency was 24.7% 30 days after ACS, and decreased by 4% six months later. As expected, higher frequencies of alcohol abuse were observed in men, younger individuals and smokers. Data from a Brazilian population-based study, the Megacity Mental Health Survey, performed with 5,037 individuals in the city of São Paulo, reported an overall lifetime prevalence of alcohol abuse of 9.8%. In a sex-stratified analysis, a higher prevalence of alcohol abuse was found among men (16.4% vs. 4.0%) based on the DSM-VI and WHO-Composite International Diagnostic Interview (WMH-CIDI)21. Another Brazilian hospital-based study performed with 345 patients with ACS (206 with MI and 139 with UA) interviewed about sociodemographic data, smoking status, screening for depression (Prime-MD and Beck Depression Inventory - BDI) and anxiety (State-Trait Anxiety Inventory for Morilha et al. Alcohol abuse and acute coronary syndrome Original Article Table 1 – Baseline characteristics of the 146 participants in the sub-study of alcohol abuse/dependence in the ERICO study, according to the presence of harmful alcohol use 30 days after an acute coronary event Sociodemographic characteristics Low-risk n = 110 (75.3%) High-risk* n = 36 (24.7%) Total n = 146 (100%) p value Age range (%) 35-44 years 4 (3.6) 3 (8.3) 7 (4.8) 45-54 years 19 (17.3) 13 (36.1) 32 (21.9) 55-64 years 39 (35.5) 12 (33.3) 51 (34.9) 65-74 years 28 (25.5) 3 (8.3) 31 (21.2) ≥ 75 years 20 (18.2) 5 (13.9) 25 (17.1) Male 63 (57.3) 32 (88.9) 95 (65.1) Female 47 (42.7) 4 (11.1) 51 (34.9) 0.046 Gender (%) 0.001 Educational level (%) 9 (8.2) 2 (5.6) 11 (7.5) 1-7 years of education Illiterate 42 (38.2) 18 (50.0) 60 (41.1) ≥ 8 years of education 59 (53.6) 16 (44.4) 75 (51.4) Single 8 (7.3) 4 (11.1) 12 (8.2) Married 0.47 Marital Status (%) 73 (66.4) 28 (77.8) 101 (69.2) Separated 8 (7.3) 3 (8.3) 11 (7.5) Widow(er) 21 (19.1) 1 (2.8) 22(15.1) White 75 (68.2) 19 (54.3) 94 (64.8) 0.20 Self-reported ethnicity (%) Brown 31 (28.2) 14 (40.0) 45 (31.0) Black 2 (1.8) 2 (5.7) 4 (2.8) Yellow 2 (1.8) - 2 (1.4) 0.25 Clinical comorbidities (%) Smoking Current 30 (27.3) 19 (52.8) 49 (33.6) Past 45 (40.9) 14 (38.9) 59 (40.4) Never 35 (31.8) 3 (8.3) 38 (26.0) Hypertension 83 (76.9) 21(58.3) 104 (72.2) 0.004 0.03 Diabetes mellitus 37 (33.9) 7 (20.6) 44 (30.8) 0.14 Dyslipidemia 57 (56.4) 13(39.4) 70 (52.2) 0.09 Sedentary lifestyle 73 (68.9) 18 (51.4) 91 (64.5) 0.06 Major depression† 37 (33.6) 15 (41.7) 52 (35.6) 0.38 Acute Coronary Syndrome subtype (%) Unstable angina 28 (25.5) 4 (11.1) 32 (21.9) NSTEMI 46 (41.8) 16 (44.4) 62 (42.5) STEMI 36 (32.7) 16 (44.4) 52 (35.6) 0.16 STEMI: ST-elevation myocardial infarction; NSTEMI: non-ST-elevation myocardial infarction. Some proportions might not add up to 100% due to rounding or missing values. *Individuals who scored 8 points or more on the AUDIT were considered with tendency to alcohol abuse. †The PHQ-9 score ≥ 10 points suggested major depression. P-values are derived from the Chi-square test. Arq Bras Cardiol. 2015; 104(6):457-467 460 Morilha et al. Alcohol abuse and acute coronary syndrome Original Article 11.1% 10.0% 44.4% 43.3% 44.4% 46.7% 0.16 0.14 Figure 1 – Alcohol consumption suggestive of alcohol abuse detected by AUDIT in the subsample from the ERICO study. UA: Unstable Angina; NSTEMI: non-ST-elevation acute myocardial infarction; STEMI: ST-elevation myocardial infarction. Adults - STAI), and alcohol consumption (AUDIT) has reported lower AUDIT scores for both sexes as compared to those found in our study. Similar to our findings, that study has reported no association between alcohol intake and depression22. Regarding CVRF, participants at high risk for alcohol abuse had a higher frequency of smoking but lower frequencies of hypertension, dyslipidemia, diabetes and sedentary lifestyle as compared to low-risk participants. However, when analyzing each item separately, significant associations were observed with some binging behaviors in the AUDIT domains, such as “increased salience of drinking” and “morning drinking”, and smoking, sedentary lifestyle, hypertension, diabetes, and even ACS subtype. After six months, a high risk of alcohol abuse remained among younger individuals (≤ 54 years) and smokers. The relationship between alcohol consumption and CVD, particularly CHD, is controversial4-9,23. Some studies have suggested that a light-moderate alcohol consumption may have a favorable impact on morbidity and mortality from ischemic heart disease6-8. However, the cardioprotective effect of drinking disappears with heavy drinking (binge) 6-8 . Russel et al. 6 have tested a linear dose-response model for the association between drinking patterns and MI6. A lower MI risk was associated with the consumption of less than 4.55 drinks per day for men (95% CI: 2.77 to 7.18) and less than 3.08 drinks per day for women (95% CI: 1.35 to 5.16), and that risk increased after these crossover points were exceeded. The MI risk increased as drinking dosage doubled, regardless of sex6. 461 Arq Bras Cardiol. 2015; 104(6):457-467 The Prospective Epidemiological Study of Myocardial Infarction (PRIME) has investigated the effect of alcohol intake patterns on ischemic heart disease in Northern Ireland and France in 9,778 men aged 50-59 years, free of ischemic heart disease at baseline, during a 10-year follow-up 7. After multivariate analysis for classic CVRF and center, the hazard ratio for hard coronary events (incident MI and coronary death) compared with regular drinkers was as follows: 1.97 (95% CI: 1.21 to 3.22) for binge drinkers; 2.03 (95% CI: 1.41 to 2.94) for never drinkers; and 1.57 (95% CI: 1.11 to 2.21) for former drinkers for the entire cohort. Only wine drinking was associated with a lower risk of hard coronary events, irrespective of the country7. A systematic review that investigated the relationship between alcohol consumption and some CVD endpoints performed with more than 4,000 studies has described a dose-response effect, demonstrated by the lowest risk of CHD mortality occurring with one to two drinks per day23. Another systematic review including 44 observational studies (case-control or cohort) has reported a relative risk of alcohol intake in relation to ischemic heart disease risk. The analyses included 957,684 participants and substantial heterogeneity across studies was found, making it difficult to confirm any cardioprotective effect of alcohol use on ischemic heart disease for all drinkers, even at low intake levels8. The pathophysiology of the cardioprotective effects of most alcoholic beverages is probably due to a high-density lipoprotein elevation and the ability of alcohol to prevent platelet aggregation and increase fibrinolysis; particularly an increased favorable effect from red wine24. Morilha et al. Alcohol abuse and acute coronary syndrome Original Article Table 2 – Distribution of positive answers according to baseline characteristics by AUDIT domains 30 days after an acute event in the sub‑sample of 146 participants from the ERICO study Domains Subgroup of risk Hazardous alcohol consumption p-value Frequency of drinking (question 1) Male gender (%) 46 (79.3) 0.003 Single 6 (10.3) 0.04 Married 43 (74.1) Separated 6 (10.3) Widow(er) 3 (5.2) Marital status (%) Smoking (%) Current 28 (48.3) Past 24 (41.4) Never 6 (10.3) < 0.001 Typical quantity (question 2) Male gender (%) 21 (84,0) 0.003 Current 17(68,0) < 0.001 Past 7 (28,0) Never 1(4,0) Smoking (%) Frequency of heavy drinking (question 3) Male gender (%) 36 (87.8) < 0.001 Current 20 (48.8) 0.02 Past 16 (39.0) Never 5 (12.2) Smoking (%) Dependence Symptoms Impaired control over drinking (question 4) Acute coronary syndrome subtype (%) Unstable angina 0 (0) NSTEMI 5 (38.5) STEMI 8 (61.5) Acute coronary syndrome subtype (%) Unstable angina 0.053 Increased salience of drinking (question 5) 0 (0) 0.046 NSTEMI 2 (25.0) STEMI 6 (75.0) Morning drinking (question 6) Male gender (%) 18 (85.7) 0.03 Hypertension (%) 11 (52.4) 0.03 Diabetes mellitus (%) 2 (10.0) 0.03 Harmful alcohol consumption Guilt after drinking(question 7) None Arq Bras Cardiol. 2015; 104(6):457-467 462 Morilha et al. Alcohol abuse and acute coronary syndrome Original Article Continuation Blackouts (question 8) None Alcohol-related injuries (question 9) Male gender Dyslipidemia (%) 9 (100,0) 0.02 1 (12,5) 0.02 Others concerned about drinking consumption (question 10) Age range (years) (%) 35-44 4 (9.8) 45-54 14 (34.1) 55-64 14 (34.1) 65-74 3 (7.3) ≥ 75 6 (14.6) Male gender (%) 0.02 34 (82.9) 0.005 Current 24 (58.5) < 0.001 Past 15 (36.6) Smoking (%) Never 2 (4.9) Hypertension (%) 23 (56.1) 0.006 Sedentary lifestyle (%) 19 (47.5) 0.008 P-values are derived from the Chi-square test. Some proportions may not round up to 100% because of missing data STEMI: ST-elevation myocardial infarction; NSTEMI: non-ST-elevation myocardial infarction. Limitations We did not evaluate the alcohol intake with a specific food questionnaire. However, we used a very reliable instrument to screen alcohol abuse/dependence 16. In the present study, two well-trained and experienced psychologists interviewed our patients; however the presence of a psychiatrist during the study could have contributed further to the detection of new cases of alcohol abuse or even depression. We found some significant differences in the frequency of some sociodemographic factors, such as educational level, self-reported ethnicity and marital status, as well as, some CVRF, such as diabetes and sedentary lifestyle, comparing participants from the alcohol abuse study with those who did not participate in this sub-study. Of note, all these characteristics are very subject to recall bias and had no interference on the alcohol abuse pattern in our main analyses. Additionally, the extent to which the findings can be generalized is limited due to the small sample size from one single center. Thus, we cannot rule out the possibility of a selection bias. 463 Arq Bras Cardiol. 2015; 104(6):457-467 Conclusions We found high frequency of alcohol abuse, which remained during the six-month follow-up, regardless of the ACS subtype. Hazardous alcohol consumption was strongly evident among younger individuals aged 35-54 years and smokers. In the present study, the binge drinking pattern was observed among smokers, individuals with a sedentary lifestyle, hypertension, diabetes and STEMI. Author contributions Conception and design of the research: Morilha A, Karagulian S, Goulart AC. Acquisition of data: Morilha A, Karagulian S, Goulart AC. Analysis and interpretation of the data: Lotufo PA, Santos IS, Goulart AC. Statistical analysis: Morilha A, Lotufo PA, Santos IS, Benseñor IM, Goulart AC. Obtaining financing: Goulart AC. Writing of the manuscript: Morilha A, Karagulian S, Lotufo PA, Santos IS, Benseñor IM, Goulart AC. Critical revision of the manuscript for intellectual content: Morilha A, Karagulian S, Lotufo PA, Santos IS, Benseñor IM, Goulart AC. Supervision / as the major investigador: Morilha A, Goulart AC. Morilha et al. Alcohol abuse and acute coronary syndrome Original Article Table 3 – Factors associated with alcohol abuse/dependence assessed on logistic regression by AUDIT on 142 participants of the ERICO study 180 days after an acute coronary event Acute Coronary Syndrome Low-risk OR (95%CI) High-risk * multivariate OR (95%CI) UA Reference (1.0) Reference (1.0) NSTEMI Reference (1.0) 1.27 (0.18-8.92) STEMI Reference (1.0) 1.77 (0.24-12.99) Female Reference (1.0) Reference (1.0) Male Reference (1.0) 3.51 (0.78-15.82) 35-44 years Reference (1.0) 38.30 (1.44-1021.56) 45-54 years Reference (1.0) 10.10 (1.06-96.46) 55-64 years Reference (1.0) 0.71 (0.09-5.87) 65-74 years Reference (1.0) 1.07 (0.11-10.81) ≥ 75 years Reference (1.0) Reference (1.0) Current Reference (1.0) 51.09 (3.49-748.01) Past Reference (1.0) 40.29 (2.37-685.93) Never Reference (1.0) Reference (1.0) Hypertension Reference (1.0) 1.43 (0.36-5.68) Diabetes mellitus Reference (1.0) 0.90 (0.19-4.25) Dyslipidemia Reference (1.0) 0.36 (0.10-1.30) Sedentary lifestyle Reference (1.0) 0.29 (0.09-0.99) Gender Age Range Smoking * Subjects who scored 8 points or more on the AUDIT were considered with high-risk alcohol abuse. STEMI: ST-elevation myocardial infarction; NSTEMI: non-ST-elevation myocardial infarction; UA: unstable angina. OR (odds ratio), 95% confidence interval (95%CI). Multivariate OR was adjusted for ACS subtype, gender, age, smoking, medical diagnosis or medication use for hypertension, diabetes mellitus and dyslipidemia, and sedentary lifestyle. Except itself. Potential Conflict of Interest No potential conflict of interest relevant to this article was reported. Study Association This article is part of the thesis of master submitted by Abner Morilha, from University of São Paulo (USP). Sources of Funding This study was funded by FAPESP. Arq Bras Cardiol. 2015; 104(6):457-467 464 Morilha et al. Alcohol abuse and acute coronary syndrome Original Article Table 4 – Comparison of baseline characteristics of 142 individuals from the alcohol abuse sub-study and those of 83 individuals who were not followed-up 180 days post-ACS in the ERICO study Baseline characteristics ERICO participants with 180-day follow-up in the alcohol abuse sub-study YES (n = 142) NO (n = 83) 7 (4.9) 2 (2.4) 0.21 Age range (years) (%) 35-44 p-value 45-54 34 (23.9) 14 (16.9) 55-64 50 (35.2) 24 (28.9) 65-74 28 (19.7) 23 (27.7) ≥ 75 23 (16.2) 20 (24.1) Male 91 (64.1) 48 (57.8) Female 51 (35.9) 35 (42.2) 28 (19.7) 15 (18.3) Gender (%) 0.04 Educational level (years) (%) Up to 8 0.35 9-11 85 (59.9) 46 (56.1) ≥ 11 29 (20.4) 20 (24.4) 0.18 Marital status (%) Single 12 (8.5) 11 (13.4) Married 99 (69.7) 44 ( 53.7) Divorced 9 (6.3) 9 (11.0) Widow(er) 22 (15.5) 18 (22.0) 0.03 Self-reported ethnicity (%) White 91 (64.5) 57(69.5) Brown 45 (31.9) 16 (19.5) Black 3 (2.1) 8 (9.8) Asian 2 (1.4) 1 (1.2) Current 49 (34.5) 25 (30.5) Past 56 (39.4) 28 (34.1) Clinical comorbidities (%) Smoking 0.34 Never 37 (26.1) 29 (35.4) Hypertension 100 (71.4) 63 (75.9) 0.47 Diabetes mellitus 41 (29.5) 32 (38.6) 0.17 Dyslipidemia 67 (51.5) 41 (56.9) 0.46 Sedentary lifestyle 88 (63.8) 66 (81.5) 0.006 Unstable angina 36 (25.4) 30 (36.1) NSTEMI 54 (38.0) 34 ( 41.0) STEMI 52 (36.6) 19 (22.9) 0.09 Acute coronary syndrome (%) STEMI: ST-elevation myocardial infarction; NSTEMI: non-ST-elevation myocardial infarction Some proportions might not add up to 100% due to rounding or missing values. P-values are derived from the Chi-square test. 465 Arq Bras Cardiol. 2015; 104(6):457-467 Morilha et al. Alcohol abuse and acute coronary syndrome Original Article Table 5 – Comparison of baseline characteristics of 146 participants from the alcohol abuse sub-study and those of the ERICO study population Baseline characteristics Participants (n = 146) Non participants (n = 820) p-value 62 (11.8) 63 (13.6) 0.26 Male 95 (65.1) 476 (58.0) 0.11 Female 51 (34.9) 344 (42.0) Mean age ( ± SD) Gender (%) 0.02 Educational level (years) (%) Up to 8 98 (67.1) 631 (77.1) 9-11 30 (20.5) 131 (16.0) ≥ 11 18 (12.3) 56 (6.8) Single 45 (30.8) 329 (40.4) Married 101 (69.2) 486(59.6) White 94 (64.4) 538(65.6) Brown 45 (30.8) 224 (27.3) Black 4 (2.7) 46(5.6) Asian 3 (2.1) 12 (1.5) Current 49 (33.6) 257 (28.8) Past 59 (40.4) 325 (36.5) Never 38 (26.0) 309 (34.7) Hypertension Marital status (%) 0.03 Self-reported ethnicity (%) Clinical comorbidities (%) Smoking 0.12 104 (72.2) 624 (78.0) 0.13 Diabetes mellitus 44(30.8) 326 (41.2) 0.02 Dyslipidemia 70 (52.2) 386 (55.4) 0.50 Sedentary lifestyle 92 (64.8) 552 (73.0) 0.05 0.02 Acute coronary syndrome (%) Unstable angina 36 (24.7) 282 (34.4) NSTEMI 57 (39.0) 321 (39.1) STEMI 53 (36.3) 217 (26.5) Some proportions might not add up to 100% due to rounding or missing values. P-values are derived from the Chi-square test. STEMI: ST-elevation myocardial infarction; NSTEMI: non-ST-elevation myocardial infarction Arq Bras Cardiol. 2015; 104(6):457-467 466 Morilha et al. Alcohol abuse and acute coronary syndrome Original Article References 1. World Health Organization (WHO). International guide for monitoring alcohol consumption and related harm. 2000 [cited 2013 August 21]. Available from: http://whqlibdoc.who.int/hq/2000/who_msd_ msb_00.4.pdf . 14. Osório FL, Mendes AV, Crippa A, Loureiro SR. Study of the discriminative validity of the PHQ-9 and PHQ-2 in a sample of Brazilian women in the context of primary health care. Perspect Psychiatr Care. 2009; 45(3): 216-27. 2. Greenfield TK. Individual risk of alcohol-related disease and problems. In: Heather N, Peters TJ, Stockwell T, eds. International handbook of alcohol dependence and problems - Part IV: drinking patterns and types of alcohol problem. Chichester: John Wiley & Sons Ltd; 2001.p.413-38. 15. Lima CT, Freire ACC, Silva AP, Teixeira RM, Farrell M ,Prince M. Concurrent and construct validity of the AUDIT in an urban Brazilian sample. Alcohol. 2005; 40 (6): 584-9. 3. Rossow I, Amundsen A. Alcohol abuse and suicide: a 40-year prospective study of Norwegian conscripts. Addiction. 1995;90(5):685-91. 4. Britton A, McKee M. The relation between alcohol and cardiovascular disease in Eastern Europe: explaining the paradox. J Epidemiol Commun Health. 2000; 54(5):328-32. 5. Puddey IB, Rakic V, Dimmitt SB, Beilin LJ. Influence of pattern of drinking on cardiovascular disease and cardiovascular risk factors: a review. Addiction. 1999; 94 (5):649-63. 6. Russell M, Chul Chu B, Banerjee A, Fan AZ, Trevisan M, Dorn JM et al. Drinking Patterns and Myocardial Infarction: A Linear Dose-Response Model. Alcohol Clin Exp Res. 2009; 33(2): 324-31. 7. Ruidavets JB, Ducimetière P, Evans A, Montaye M, Haas B, Bingham A, et al. Patterns of alcohol consumption and ischaemic heart disease in culturally divergent countries: the Prospective Epidemiological Study of Myocardial Infarction (PRIME).BMJ. 2010; 341: c6077. 8. Roerecke M, Rehm J. The cardioprotective association of average alcohol consumption and ischaemic heart disease: a systematic review and metaanalysis. Addiction. 2012; 107(7): 1246–60. 9. Corrao G, Rubbiati L, Bagnardi V, Zambon A, Poikolainen K. Alcohol and coronary heart disease: a meta-analysis. Addiction. 2000; 95(10): 1505-23. 10. Goulart AC, Santos IS, Sitnik D, Staniak HL, Fedeli LM, Pastore CA, et al. Design and baseline characteristics of a coronary heart disease prospective cohort: two-year experience from the strategy of registry of acute coronary syndrome study (ERICO study). Clinics (Sao Paulo). 2013; 68 (3):431-4. 11. Spitzer MB, Robert L, Gibbon M, Gibbons W, Janet BW. Structured clinical interview for DSM-IV-TR Axis I Disorders, Research Version, Non-patient Edition. (SCID-I/NP). New York: Biometrics Research/ New York State Psychiatric Institute;2002. [cited 2013 August 21]. Available from: http:// www.scid4.org/index.html . 467 16. Luepker RV, Apple FS, Christenson RH, Crow RS, Fortmann SP, Goff D ,et al. Case definitions for acute coronary heart disease in epidemiology and clinical research studies: a statement from the AHA Council on Epidemiology and Prevention; AHA Statistics Committee; World Heart Federation Council on Epidemiology and Prevention; the European Society of Cardiology Working Group on Epidemiology and Prevention; Centers for Disease Control and Prevention; and the National Heart, Lung, and Blood Institute. Circulation. 2003;108(20):2543–9. 17. Thygesen K, Alpert JS, White HD, Joint ESC/ACCF/AHA/WHF Task Force for the Redefinition of Myocardial Infarction. Universal definition of myocardial infarction. Eur Heart J. 2007;28 (20):2525–38. 18. Lykouras L, Rontos I, Rontos K, Katsaras A, Markoulis T, Papasteriades E, et al. Detecting alcohol-related problems among general hospital patients with heart disease. Psychother Psychosom.2001;70(1): 25–9. 19. Mendoza-Sassi RA, Béria JU. Prevalence of alcohol use disorders and associated factors: A population-based study using AUDIT in southern Brazil. Addiction. 2003; 98(6):799-804. 20. Barbor FT, Higgins-Biddle JC, Saunders JB, Monteiro MG. AUDIT: The Alcohol use disorder identification test. Guidelines for use in primary care. 2nd ed. Washington (DC):World Health Organization, Department of Mental Health and Substance Dependence. 2001 [cited 2013 August 21]. Available from: http://whqlibdoc.who.int/hq/2001/who_msd_ msb_01.6a.pdf 21. Viana CM, Andrade HL. Lifetime prevalence, age and gender distribution and age-of-onset of psychiatric disorders in the São Paulo Metropolitan Area, Brazil: results from the São Paulo megacity mental health survey. Rev Bras Psiquiatr. 2012;34(3):249-60. 22. Perez GH, Nicolau JC, Romano BW, Laranjeira R. Depression and acute coronary syndromes: gender-related differences. Arq Bras Cardiol. 2005:85:319-26. 12. Lourenço RA, Veras RP. Mini mental State Examination: psychometric characteristics in elderly outpatients. Rev Saude Publica. 2006; 40(4):712-9. 23. Ronksley PE, Brien SE, Turner BJ, Mukamal KJ, Ghali WA. Association of alcohol consumption with selected cardiovascular disease outcomes: a systematic review and meta-analysis. BMJ. 2011;342:d671. 13. Kroenke K, Spitzer RL, Williams JBW. The PHQ-9 Validity of a brief depression severity measure. J Gen Intern Med.2001;16(9):606-13. 24. Constant J. Alcohol, ischemic heart disease, and the French paradox. Coron Artery Dis. 1997;8(10):645-9. Arq Bras Cardiol. 2015; 104(6):457-467 Back to the Cover Original Article APOE and LDLR Gene Polymorphisms and Dyslipidemia Tracking. Rio de Janeiro Study Rossana Ghessa Andrade de Freitas1, Erika Maria Gonçalves Campana1,2, Roberto Pozzan1,2, Andréa Araujo Brandão1,2, Ayrton Pires Brandão1,2, Maria Eliane Campos Magalhães1,2, Dayse Aparecida da Silva1,3 Universidade do Estado do Rio de Janeiro1; Hospital Universitário Pedro Ernesto2; Instituto de Biologia Roberto Alcântara Gomes3, Rio de Janeiro, RJ – Brazil Abstract Background: Studies show an association between changes in apolipoprotein E (ApoE) and LDLR receptor with the occurrence of dyslipidemia. Objectives: To investigate the association between polymorphisms of the APOE (ε2, ε3, ε4) and LDLR (A370T) genes with the persistence of abnormal serum lipid levels in young individuals followed up for 17 years in the Rio de Janeiro Study. Methods: The study included 56 individuals (35 males) who underwent three assessments at different ages: A1 (mean age 13.30 ± 1.53 years), A2 (22.09 ± 1.91 years) and A3 (31.23 ± 1.99 years). Clinical evaluation with measurement of blood pressure (BP) and body mass index (BMI) was conducted at all three assessments. Measurement of waist circumference (WC) and serum lipids, and analysis of genetic polymorphisms by PCR-RFLP were performed at A2 and A3. Based on dyslipidemia tracking, three groups were established: 0 (no abnormal lipid value at A2 and A3), 1 (up to one abnormal lipid value at A2 or A3) and 2 (one or more abnormal lipid values at A2 and A3). Results: Compared with groups 0 and 1, group 2 presented higher mean values of BP, BMI, WC, LDL-c and TG (p < 0.01) and lower mean values of HDL-c (p = 0.001). Across the assessments, all individuals with APOE genotypes ε2/ε4 and ε4/ε4 maintained at least one abnormal lipid variable, whereas those with genotype ε2/ε3 did not show abnormal values (χ2 = 16.848, p = 0.032). For the LDLR genotypes, there was no significant difference among the groups. Conclusions: APOE gene polymorphisms were associated with dyslipidemia in young individuals followed up longitudinally from childhood. (Arq Bras Cardiol. 2015; 104(6):468-475) Keywords: Polymorphism, Genetic; Dyslipidemias; Young Adult; Epidemiology; Apolipoproteins E. Introduction Cardiovascular diseases (CVDs) are the leading causes of death in adults worldwide, contributing to high rates of early morbidity and mortality1,2. In Brazil, CVDs concentrate annually 1/3 of the overall deaths3,4. Dyslipidemia is one of the risk factors (RF) for development of CVDs 5. Given its importance, studies are being conducted to determine the abnormalities associated with plasma lipid changes and their implications on the occurrence of CVDs6,7. In genetics, several gene polymorphisms and mutations have been identified and associated with atherosclerosis and coronary artery disease (CAD)8,9. This is the case of the apolipoprotein E (ApoE), which is essential for the transport and metabolism of Mailing address: Rossana Ghessa Andrade de Freitas • Laboratório de Diagnósticos por DNA. Universidade do Estado do Rio de Janeiro. Instituto de Biologia Roberto Alcântara Gomes. Rua São Francisco Xavier, 524, Pavilhão Haroldo Lisboa da Cunha. Postal Code 20550-900, Rio de Janeiro, RJ – Brazil E-mail: [email protected] Manuscript received August 27, 2014; revised manuscript January 21, 2015; accepted January 28, 2015. DOI: 10.5935/abc.20150036 468 cholesterol and structural stability of lipoproteins 10,11, and whose gene has three polymorphic alleles (ε2, ε3 and ε4) 12. Population studies have shown higher plasma levels of low-density lipoprotein cholesterol (LDL-c) in carriers of the ε4 allele12, leading to an association of this allele with the occurrence of CVDs13. Mutations in the LDL receptor gene (LDLR) have also been implicated with dyslipidemias, particularly in primary forms of homozygous or heterozygous hypercholesterolemia such as familial hypercholesterolemia (FH), a condition associated with early severe atherosclerosis and CAD14‑16. The LDLR gene encodes a protein with binding domains for apolipoproteins B and E. Among the different polymorphisms found in the LDLR gene, the A370T has been investigated for its association with increased lipid levels and cardiovascular risk17,18. Dyslipidemias may be present from an early age, and abnormal lipids tend to persist over time (tracking effect) until adulthood. The identification of genetic markers involved with abnormal lipid metabolism may contribute to the recognition at a young age of patterns of genetic susceptibility and guide interventions to correct these abnormalities. Freitas et al. Genetic polymorphisms and dyslipidemia tracking Original Article Based on that, the aim of this study was to investigate the distribution pattern of polymorphisms of the APOE and LDLR genes and their associations with the dyslipidemia phenotype, notably on its tracking effect, in a young population followed up for 17 years. Method The sample of this study was retrieved from the Study of Rio de Janeiro (Estudo do Rio de Janeiro, ERJ). This longitudinal cohort study is part of a line of research on blood pressure (BP) and other cardiovascular RFs in young adults developed in 1983 at the Hypertension Unit of the Hospital Universitário Pedro Ernesto (HUPE) at Universidade do Estado do Rio de Janeiro (UERJ)19. The ERJ included three different assessments, named A1, A2 and A3. Assessment A1 was conducted between 1987 and 1988 in individuals aged 10-16 years (mean 13.30 ± 1.53 years), A2 was conducted between 1996 and 1999 in individuals aged 18-26 years (mean 22.09 ± 1.91 years) and A3 was conducted between 2004 and 2005 in individuals aged 27‑35 years (mean 31.23 ± 1.99 years)19. We selected for genetic evaluation 75 individuals from the original ERJ cohort who had undergone all three assessments (A1, A2 and A3). However, laboratory evaluation was not performed in 19 individuals at A2 and these individuals were excluded from the analysis, yielding a study sample of 56 individuals with serum lipid evaluation at assessments A2 and A3, as well as genetic profile evaluation. Dyslipidemia was considered present when one or more lipid values were increased (total cholesterol [Col-T], LDL-c and triglycerides [TG]) or decreased (high-density lipoprotein cholesterol [HDL-c]), alone or in combination, using as cutoff values those recommended by the V Brazilian Guideline on Dyslipidemias and Atherosclerosis Prevention20. The tracking effect consists of a repeat behavior of these abnormal variables (increase or decrease) at both assessments conducted during young adulthood (A2 and A3). Three groups were established based on the occurrence of dyslipidemia tracking: Measurement of BP Measurement of BP was carried out according to the recommendations of the VI Brazilian Guidelines of Hypertension21. The BP was measured on the right arm, with the individual lying down and then seated, using an aneroid mercury sphygmomanometer (Romed) fixed to the wall, and zeroed to the midaxillary line. We selected cuffs with size and width suitable for the circumference and length of the individuals’ arms. We considered as systolic BP (SBP) the appearance of the first Korotkoff sound (Korotkoff phase I), and for diastolic BP (DBP), the disappearance of the sound (Korotkoff phase V). The BP was measured three times with 5-minute intervals between each measurement, and the last measurement was used for the analysis. We considered the BP to be increased in A1 when SBP and/or DBP was ≥ 95th percentile for gender and age, and in A2 and A3 when SBP was ≥ 140 mmHg and/or DBP ≥ 90 mmHg. Anthropometric variables Weight (W) and height (H) were measured on a platform scale (Filizola, São Paulo, Brazil) with a 150-kilogram (kg) capacity and 100-gram precision. Weight was expressed in kg and determined with the individual barefoot and wearing light clothes. Height was expressed in centimeters (cm) and determined from the distance between the vertex of the head to the soles of the feet with the individual in an upright position and barefoot22. From the measurements of weight and height, we calculated the BMI using the formula BMI = W/H2 and expressed the results in kg/m2. The WC was measured parallel to the ground with a flexible and inelastic tape measure with precision of 0.1 cm, with the individual in an upright position and the abdomen relaxed. The measurement was determined horizontally on the shortest distance between the lower border of the last rib and the iliac crest, with the tape held firmly but without pressure against the skin22. Laboratory variables Group 0: No abnormal lipid variables in A2 and A3; n = 11 individuals (10 women) with a mean age of 30.89 ± 1.64 years; Blood was collected by antecubital venipuncture under standard conditions in the morning (before 8:30 am) after a 12-hour fasting. Group 1: At least one abnormal lipid variable in one of the evaluations (A2 or A3); n = 12 individuals (10 men) with a mean age of 31.47 ± 2.35 years; All samples were placed in siliconized vacuum tubes and processed in up to 30 minutes. Measurements were performed in the serum obtained after centrifugation at a speed of 3,500 rotations per minute for five minutes. Group 2: One or more abnormal lipid variables in two evaluations (A2 and A3); n = 33 individuals (24 men) with a mean age of 31.25 ± 1.99 years. Clinical, anthropometric, laboratory, and genetic evaluations Both BP and BMI were evaluated at A1, A2 and A3. The A2 and A3 assessments also included measurements of Col-T, HDL-c and TG after a 12-hour fasting, and calculation of LDL-c. Blood collection for genetic testing and measurement of waist circumference (WC) were performed at A3. For measurement of serum cholesterol and HDL-c, we used the enzymatic colorimetric method CHOD/PAP and for measurement of TG, we used the enzymatic method GPD/BAP. To calculate the LDL-c levels, we used the Friedewald formula when TG levels were < 400 mg/dl. Genetic analysis DNA was extracted by the salting-out method using 2-ml aliquots of whole blood23. The analyses of the allelic variants of the APOE gene (ε2, ε3, ε4) were carried out with Arq Bras Cardiol. 2015; 104(6):468-475 469 Freitas et al. Genetic polymorphisms and dyslipidemia tracking Original Article the technique of polymerase chain reaction (PCR) with the primers APOE F 5'- TAA GCT TGG CAC GGC TGT CCA AGG A-3' and APOE R 5'- ACA GAA TTC GCC CCG GCC TGG TAC AC-3' in 35 PCR cycles (95ºC for 60 sec, 63ºC for 60 sec and 72ºC for 120 sec) to amplify a product of 244 base pairs (bp)24. The products of PCR amplification were digested with the enzyme HhaI (Fermentas) and the fragments were visualized in 12% polyacrylamide gel by silver nitrate staining. The fragments representing each genotype are as follows: ε2ε3 (91, 83 and 48 bp), ε3ε4 (91, 72 and 48 bp), ε2ε4 (91, 83, 72 and 48 bp) and ε3ε3 (91 and 48 bp). To genotype the A370T polymorphism, a region of 150 bp was amplified by PCR using the primers P1: 5’‑GAG TGT CAG GAT CCC GAC ACC TGC GCC-3’ and P2: 5 '-AAG TCG ACC CAC CCG CCT GCC TCC CGT-3' in 35 cycles (95°C for 60 sec, 68°C for 60 sec and 72° C for 120 sec)25. To determine the polymorphism, PCR products were digested with the enzyme HaeIII (Biotech), and fragments were separated on 3.5% agarose gel and visualized by ethidium bromide staining. The fragments representing A allele were 77, 47 and 26 bp, and those representing the T allele were 124 and 26 bp. To demonstrate the random genetic distribution of the ERJ cohort, the genotype and allelic frequencies of the polymorphisms analyzed in the study were compared with those observed in a cohort of 75 non-hospitalized individuals (41 men and 34 women) randomly selected from a DNA database of more than 10,000 individuals who underwent parental testing, provided for this study by the Laboratório de Diagnósticos por DNA (LDD) at UERJ. This sample was identified as LDD. It is worth noting that the populations are not required to be phenotypically homogeneous for comparison of genetic distribution. The study was approved by the Ethics Committee for Research of HUPE under the number 2130-CEP/HUPE, and all participants signed an Informed Consent Form. Statistical Analysis For statistical treatment of the data, we used the software SPSS for Windows version 12.0 (Chicago, Illinois, USA). Gene and haplotype frequencies were estimated according to Saitou and Nei26, using the program Arlequin, version 3.0 27. Chi-square test (χ²) and analysis of variance (F) were used to compare the pattern of distribution of the polymorphisms with clinical anthropometric and lipid variables, with p < 0.05 results considered significant. The test of homogeneity of variances was applied to evaluate the normal distribution of the studied variables. Results The sample consisted of 56 individuals, 35 (62.5%) of whom were males and 21 (37.5%) females, aged between 27-35 years (mean 31.23 ± 1.99 years). Table 1 presents the clinical, anthropometric and laboratory variables of the studied population at all three assessments (A1, A2 and A3). Table 2 shows the results of clinical (SBP and DBP), anthropometric (WC and BMI) and laboratory (Col-T, HDL-c, LDL-c and TG) variables at A3 for all three groups (groups 0, 1 and 2) stratified by dyslipidemia tracking. When compared with groups 0 and 1, group 2 presented higher mean values of SBP, BMI, WC, TG and LDL-c and lower mean values of HDL-c. The genetic analysis of the 56 individuals identified the following genotypes for APOE: ε3ε3 (62.5%), ε3ε4 (25.0%), ε2ε3 (5.4%), ε2ε4 (5.4%) and ε4ε4 (1.8%) (Table 3). As for the distribution of the APOE genotypes in the groups according to the occurrence of dyslipidemia tracking, we observed that in group 0, genotype ε3ε3 affected 45.5% of the individuals, followed by ε2ε3 and ε3ε4, each affecting 27.3% of the individuals. In group 1, the ε3ε3 genotype was present in 83.3% of the individuals and the ε3ε4 genotype in 16.7%. Genotypes ε2ε3, ε2ε4 and ε4ε4 were not observed in group 1. In group 2, which Table 1 – Clinical, anthropometric and laboratory variables of the studied population at three assessments* Evaluations Variables A1 (n = 56) A2 (n = 56) A3 (n = 75) Age (years) 13.30 ± 1.53 22.09 ± 1.91 31.23 ± 1.99 SBP (mmHg) 115.28 ± 14.83 124.35 ± 13.79 125.43 ± 16.67 DBP (mmHg) 63.81 ± 12.84 79.86 ± 10.79 83.20 ± 13.72 BMI (kg/m ) 20.26 ± 3.05 24.04 ± 3.64 26.79 ± 5.53 WC (cm) - - 92.96 ± 14.66 Col-T (mg/dL) - 175.37 ± 34.34 181.44 ± 31.72 TG (mg/dL) - 88.37 ± 42.34 103.71 ± 56.14 HDL-c (mg/dL) - 45.87 ± 13.16 49.05 ± 15.87 LDL-C (mg/dL) - 111.82 ± 27.58 111.23 ± 27.95 2 * Values are expressed as mean ± standard deviation; SBP: systolic blood pressure; DBP: diastolic blood pressure; BMI: body mass index; WC: waist circumference; Col-T: total cholesterol; TG: triglycerides; HDL-c: high-density lipoprotein cholesterol; LDL-c: low-density lipoprotein cholesterol. 470 Arq Bras Cardiol. 2015; 104(6):468-475 Freitas et al. Genetic polymorphisms and dyslipidemia tracking Original Article Table 2 – Clinical, anthropometric and laboratory variables at A3 in the studied groups according to dyslipidemia tracking* Variables Groups of dyslipidemia 0 (n = 11) 1 (n = 12) 2 (n = 33) Test F p Age (years) 30.89 ± 1.64 31.47 ± 2.35 31.25 ± 1.99 0.239 0.788 SBP (mmHg) 114.36 ± 14.58 120.17 ± 13.05 129.76 ± 15.79 5.01 0.01 DBP (mmHg) 76.36 ± 8.66 78.17 ± 13.89 85.27 ± 13.44 2.69 0.07 BMI (kg/m2) 23.81 ± 3.72 24.34 ± 4.02 28.67 ± 5.81 5.43 0.007 WC (cm) Col-T (mg/dL) 80.50 ± 6.74 86.91 ± 8.72 98.63 ± 14.26 10.86 < 0.001 164.45 ± 18.35 179.58 ± 29.12 187.78 ± 34.50 2.37 0.10 HDL-c (mg/dL) 62.09 ± 9.63 53.0 ± 11.55 43.51 ± 15.99 7.50 0.001 LDL-C (mg/dL) 89.47 ± 13.59 106.56 ± 28.60 119.90 ± 27.55 6.01 0.004 TG (mg/dL) 64.18 ± 31.44 81.33 ± 41.37 125.03 ± 57.68 7.48 0.001 10 F / 1 M 2 F/ 10 M 9 F/ 24 M - - Gender * Values expressed as mean ± standard deviation; group 0: no abnormal lipid variable at A2 and A3; group 1: one or more abnormal lipid variables at A2 or A3; group 2: one or more abnormal lipid variables at A2 and A3; SBP: systolic blood pressure; DBP: diastolic blood pressure; BMI: body mass index; WC: waist circumference; Col-T: total cholesterol; HDL-c: high-density lipoprotein cholesterol; LDL-c: low-density lipoprotein cholesterol; TG: triglycerides; F: female; M: male; F-test: analysis of variance. Table 3 – APOE genotypes according to dyslipidemia group* Dyslipidemia group APOE genotypes ε2ε3 n(%) Total 0 n = 11 (19.6%) 1 n = 12 (21.4%) 2 n = 33 (59.0%) n = 56 (100.0%) 3 (27.3%) - - 3 (5.4%) ε3ε3 n(%) 5 (45.5%) 10 (83.3%) 20 (60.6%) 35 (62.5%) ε3ε4 n(%) 3 (27.3%) 2 (16.7%) 9 (27.3%) 14 (25%) ε2ε4 n(%) - - 3 (9.1%) 3 (5.4%) ε4ε4 n(%) - - 1 (3.0%) 1 (1.8%) * Values are expressed as n (%) χ = 16.848; p = 0.032; APOE: apolipoprotein E gene; group 0: no abnormal lipid variable at A2 and A3; group 1: one or more abnormal lipid variables at A2 or A3; group 2: one or more abnormal lipid variables at A2 and A3. 2 featured the greatest genotype diversity in the sample, the distribution was 60.6% for ε3ε3, 27.3% for ε3ε4, 9.1% for ε2ε4 and 3% for ε4ε4. Genotype ε2ε3 was not observed in this group. This distribution had statistical significance (χ2 = 16.848, p = 0.0032) and showed that 39.4% of the individuals in group 2 had genotypes containing the ε4 allele. It should be noted that all subjects with genotypes ε2ε4 and ε4ε4 maintained at least one abnormal lipid value in A2 and A3 (group 2 – one or more abnormal lipid variables in A2 and A3), whereas none of the subjects with genotype ε2ε3 had abnormal lipids (group 0 – no abnormal lipid values in A2 and A3) (Table 3). We also analyzed the polymorphisms of the LDLR gene and identified the following genotypes: AA in 85.7%, AT in 12.5% and TT in 1.8% of the individuals (Table 4). The analysis of the distribution of LDLR genotypes according to dyslipidemia tracking showed no statistically significant difference between the groups (Table 4). For comparison purposes, the genotype and allele frequencies of APOE and LDLR gene polymorphisms of the 56 individuals from the ERJ cohort and 75 individuals from the LDD cohort are shown in Table 5. Fisher's exact test showed no significant differences between the allele distributions of the ERJ and LDD cohorts. Discussion Studies have shown an association between APOE and LDLR genotypes with increased levels of lipid macromolecules such as Col-T, TG and LDL-c, decreased levels of HDL-c, and cardiovascular disease, especially CAD11,28. In the present study, we investigated the distribution pattern of APOE and LDLR gene polymorphisms in a population of adolescents followed up for 17 years, considering the occurrence of dyslipidemia based on change (increase or decrease) of one or more lipid variables and their repetition (tracking) at two different moments (A2 and A3) during young adulthood. Arq Bras Cardiol. 2015; 104(6):468-475 471 Freitas et al. Genetic polymorphisms and dyslipidemia tracking Original Article Table 4 – LDLR genotypes according to dyslipidemia group* Dyslipidemia group LDLR genotypes Total 0 n = 11 (19.6%) 1 n = 12 (21.4%) 2 n = 33 (59.0%) n = 56 (100.0%) AA n (%) 9 (81.8%) 10 (83.3%) 29 (87.9%) 48 (85.7%) AT n (%) 2 (18.2%) 2 (16.7%) 3 (9.1%) 7 (12.5%) TT n (%) - - 1 (3.0%) 1 (1.8%) * Values expressed as n (%) χ2 = 1.500; p = 0.827; LDLR: low-density lipoprotein receptor gene; group 0: no abnormal lipid variable at A2 and A3; group 1: one or more abnormal lipid variable at A2 or A3; group 2: one or more abnormal lipid variable at A2 and A3. Table 5 – Genotype and allele frequencies of APOE and LDLR gene polymorphisms in the ERJ and LDD cohorts APOE Genotypes LDLR Frequency (%) Genotypes ERJ(n = 56) LDD(n = 75) 5.3 4.2 ε2ε3 Frequency (%) ERJ(n = 56) LDD(n = 75) AA 88.0 86.5 ε3ε3 66.7 75.0 AT 10.6 13.5 ε3ε4 22.7 18.0 TT 1.3 - ε2ε4 4.0 2.8 ε4ε4 1.3 - Alleles Frequency (%) Alleles Frequency (%) ε2 6.6 3.5 A 93.5 93.3 ε3 79.4 86.0 T 6.5 6.7 10.5 13.5 ε4 14.0 10.5 Ho 34.6 25.0 Ho He 34.8 24.8 He 12.3 12.6 HWE p = 0.5098 DP = 0.0005 p = 0.2128 DP = 0.0004 HWE p = 0.2715 DP = 0.0004 p = 1.000 DP = 0.00 Fisher's exact test p = 0.51528 DP = 0.001 - Fisher's exact test p = 0.990, SD = 0.003 - ERJ: participants of the Rio de Janeiro Study; LDD: cohort from the Laboratório de Diagnósticos por DNA; APO: apolipoprotein E gene; LDLR: low-density lipoprotein receptor gene; He: expected heterozygosity, Ho: observed heterozygosity; HWE: Hardy-Weinberg equilibrium; SD: standard deviation. In the analysis of APOE polymorphisms based on dyslipidemia tracking, our study showed that individuals with genotype ε2ε3 were concentrated in group 0, that is, the group in which lipid variables (Col-T, TG, HDL-c and LDL-c) were normal at two evaluations (A2 and A3). These findings are in agreement with those by Ferreira et al.29 who demonstrated in a study with 216 individuals (109 with dyslipidemia and 107 without dyslipidemia) a similar frequency of allele distribution for APOE polymorphisms in both groups. However, in individuals with normal lipid levels in that study, the presence of the ε2 allele was strongly associated with low serum levels of Col-T and LDL-c, which may suggest a possible protective role associated with this allele29,30. Similarly, Bazzaz et al. 31 , in a cohort study with 320 individuals in Iran, investigated the association between APOE gene polymorphisms, lipid profile and BMI. The authors 472 Arq Bras Cardiol. 2015; 104(6):468-475 observed that the ε2 allele was more frequent in individuals with Col-T < 200 mg/dl (p = 0.01), and found an even greater association of the individuals with normal serum Col-T levels with genotype ε2ε3 when compared with individuals with abnormal levels of Col-T (p = 0.003)31. As for the ε4 allele, studies in the general population and hypertensive patients have shown an association of this allele with an increase in levels of Col-T and LDL-c. Due to that, the ε4 allele has been associated with higher risk of CAD even in healthy individuals28,32. Fuzikawa et al.30, in a study with 1,406 adults of both genders, observed a high prevalence of hypertension (61.3%) and higher average values of LDL-c in patients with the ε4 allele (p = 0.036) when compared with patients with the ε2 allele (p < 0.001)30. Similarly, Salazar et al.33 showed an association of the ε4 allele with dyslipidemias in a study that investigated APOE gene polymorphism in Freitas et al. Genetic polymorphisms and dyslipidemia tracking Original Article 150 women with and without CAD. Compared with the control group in that cohort, women with CAD showed significantly higher levels of Col-T, TG and LDL-c and a higher frequency of the ε4 allele and the ε3ε4 genotype33. In the present study, 18 individuals (32.1%) were carriers of the ε4 allele in different genotype combinations, 13 (72.2%) of whom were in group 2 which aggregated higher values of SBP, BMI and WC and therefore, worse cardiovascular risk profile. It is worth noting that the only individual in the cohort with genotype ε4ε4 was in group 2. Thus, the evidence seems to point to a possible damaging role for the ε4 allele and a protective role for the ε2 allele. However, the combination of these alleles in different genotypes can render these roles less clear. In this study for example, all subjects with genotype ε2ε4 were in group 2 which had the worse risk profile and one or more abnormal lipid variables at two evaluations. This result seems to suggest that when the ε4 allele is present, the protective role of the ε2 allele is either lost or decreased. In the present study, we also observed a predominance of males in group 2 (n = 24; 72.72%) (Table 2). This group presented the worst cardiovascular risk profile, which is in line with the premise that the male gender is associated with increased cardiovascular risk21. We found no association between LDLR gene polymorphisms and dyslipidemia tracking in the young individuals of this cohort. Frikke-Schmidt et al.25 also found no significant association between plasma levels of Col-T, LDL-c and individuals with AA genotype compared with those with a TT genotype. However, these authors reported increased risk (3.6 times) of ischemic stroke in homozygous individuals with a TT genotype compared with those with an AA genotype25. We found five genotypes for the APOE polymorphism in the ERJ cohort. As for the LDLR polymorphism, all three were found in this cohort. The most frequent APOE genotypes were ε3ε3 and the most frequent LDLR genotype was AA. It is worth noting that the genotype and allele frequencies found in the ERJ cohort for APOE gene polymorphisms were similar to those found in cohorts from other states in Brazil, such as the cohort from Rio Grande do Sul (Porto Alegre)12 and in other cohorts worldwide34. The genotype and allele frequencies of the ERJ cohort for the LDLR polymorphisms were similar to those found in other populations, such as the one from the study of Frikke-Schmidt et al.25. Similarly, the comparison of the genetic distribution in the ERJ cohort with that from a representative sample group randomly selected from the state of Rio de Janeiro (LDD), and the confirmation of the homogeneity of their distributions, suggests that the ERJ cohort has a random profile, suitable for the development of the proposed study. Despite the limitations of the study, the association between a specific genetic profile with the presence of dyslipidemia in young individuals over time in a small population brings a novel and relatively unknown perspective to the currently available medical literature. Studies with more than 20 years of follow-up, such as the ERJ, have losses associated with the longitudinal tracking of the participants, but have unequivocally contributed to a better understanding of the behavior of cardiovascular risk factors in the Brazilian population. Conclusion A study of APOE gene polymorphisms in participants of the ERJ showed that the presence of the ε4 allele was more prevalent in group 2, which consisted of young individuals with repeatedly abnormal lipid variables during longitudinal follow-up (tracking effect). This group also showed aggregation of worse anthropometric variables (higher BMI and WC) and increased BP, rendering a worse cardiovascular risk profile to these individuals. This study was partially funded by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) and Fundação Carlos Chagas de Amparo à Pesquisa do Estado do Rio de Janeiro (FAPERJ). Author contributions Conception and design of the research:Freitas RGA, Campana EMG, Brandão AA, Brandão AP, Magalhães MEC, Silva DA. Acquisition of data: Freitas RGA, Campana EMG, Brandão AP, Silva DA. Analysis and interpretation of the data: Freitas RGA, Pozzan R. Statistical analysis: Pozzan R. Writing of the manuscript: Brandão AA, Magalhães MEC, Silva DA. Critical revision of the manuscript for intellectual content: Freitas RGA. Supervision / as the major investigador:Magalhães MEC, Silva DA. Potential Conflict of Interest No potential conflict of interest relevant to this article was reported. Study Association This article is part of the thesis of master submitted by Rossana Ghessa Andrade de Freitas, from Universidade do Estado do Rio de Janeiro. Sources of Funding This study was funded by CAPES E FAPERJ. Arq Bras Cardiol. 2015; 104(6):468-475 473 Freitas et al. Genetic polymorphisms and dyslipidemia tracking Original Article References 1. World Health Organization (WHO). [Internet]. Programmes. Cardiovascular disease. About cardiovascular diseases. Definition. [cited 2013 Oct 16]. Available from: <http://www.who.int/cardiovascular_ diseases/about_cvd/en> 17. Vieira JR, Whittall RA, Cooper JA, Miller GJ, Humphries SE. The A370T variant (StuI Polymorphism) in the LDL receptor gene is not associated with plasma lipid levels or cardiovascular risk in UK men. Ann Hum Genet. 2006; 70(Pt 6):697-704. 2. 18. Wang J, Huff E, Janecka L, Hegele RA. Low density lipoprotein receptor (LDLR) gene mutations in Canadian subjects with familial hypercholesterolemia, but not of French descent. Hum Mutat. 2001;18(4):359. World Health Organization (WHO). [Internet]. Media Centre. Fact Sheets. Noncommunicable diseases. Updated March 2013. [cited 2013 Oct 16]. Available from: <http://www.who.int/mediacentre/factsheets/fs355/en/ index.html> 3. Ministério da Saúde. [Internet]. Rede Interagencial de Informações para a Saúde (RIPSA). Indicadores e dados básicos (IDB). Indicadores de mortalidade. [atualizada em 2012] [acesso em 2014 dez. 03]. Disponível em: <http://tabnet.datasus.gov.br/cgi/idb2012/matriz.htm> 4. Ministério da Saúde. Secretaria de Vigilância em Saúde. [Internet]. 6a ed. Brasília; 2009. [atualizada em 2010 dez. 14]. [acesso em 2011 jun. 20]. Disponível em: <http://portal.saude.gov.br/portal/aplicacoes/ noticias/default.cfm?pg=dspDetalheNoticia&id_area=124&CO_ NOTICIA=11994> 5. World Health Organization (WHO). [Internet]. Prevention of cardiovascular disease: guidelines for assessment and management of cardiovascular risk. Part 1: The total risk approach to prevention of cardiovascular disease. Washington DC; 2007. [cited 2013 Oct 16]. Available from:<http:// whqlibdoc.who.int/publications/2007/9789241547178_eng.pdf> 6. Berenson GS, Srinivasan SR, Bao W, Newman WP 3rd, Tracy RE, Wattigney WA. Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. The Bogalusa Heart Study. N Engl J Med. 1998;338(23):1650-6. 7. Quezada A, Fajardo MA, Rodríguez MA, Ponce G. Análisis de los factores de riesgo vinculados con el síndrome metabólico en niños de Comodoro Rivadavia. Bioquímica y Patología Clínica. 2010;74(1):30-5. 8. López-Reyes A, Rodríguez-Pérez JM, Fernández-Torres J, MartínezRodríguez N, Pérez-Hernández N, Fuentes-Gómez AJ, et al. The HIF1A rs 2057482 polymorphism is associated with risk of developing premature coronary artery disease and with some metabolic and cardiovascular risk factors. The Genetics of Atherosclerotic Disease (GEA) Mexican Study. Exp Mol Pathol. 2014;96(3):405-10. 9. Keenan TE, Rader DJ. Genetics of lipid traits and relationship to coronary artery disease. Curr Cardiol Rep. 2013;15(9):396. 10. Costa PM. Polimorfismo da apolipoproteína E e perfil de distribuição de subfrações de lipoproteínas. [Dissertação]. Porto Alegre: Pontifícia Universidade Católica do Rio Grande do Sul; 2004. 11. Martinelli N, Olivieri O, Shen GQ, Trabetti E, Pizzolo F, Busti F, et al. Additive effect of LRP8/APOER2 R952Q variant to APOE ε2/ε3/ε4 genotype in modulating apolipoprotein E concentration and the risk of myocardial infarction: a case-control study. BMC Med Genet. 2009;10:41. 12. Schwanke CHA, Cruz IBM, Leal NF, Scheibe R, Moriguchi Y, Moriguchi EH. Análise da associação entre polimorfismo do gene da apolipoproteína E e fatores de risco cardiovasculares em idosos longevos. Arq Bras Cardiol. 2002;78(6):561-70. 13. Smith JD. Apolipoprotein E4: an allele associated with many diseases. Ann Med. 2000;32(2):118-27. 14. Marques e Sá AC. O papel dos polimorfismos genéticos na doença cardíaca isquêmica [Dissertação]. Porto: Universidade do Porto; 2010. 474 19. Campana EM, Brandão AA, Pozzan R, França MF, Fonseca FL, Pizzi OL, et al. Pressão arterial em jovens como marcador de risco cardiovascular. Estudo do Rio de Janeiro. Arq Bras Cardiol. 2009;93(6):657-65. 20. Xavier HT, Izar MC, Faria Neto JR, Assad MH, Rocha VZ, Sposito AC, et al; Sociedade Brasileira de Cardiologia. V Diretriz Brasileira de Dislipidemias e Prevenção da Aterosclerose. Rio de Janeiro. Arq Bras Cardiol. 2013; 101(4 supl. 1):1-22. 21. Sociedade Brasileira de Cardiologia; Sociedade Brasileira de Hipertensão; Sociedade Brasileira de Nefrologia. VI Diretrizes Brasileiras de Hipertensão. Arq Bras Cardiol. 2010;95(1 supl. 1):1-51. 22. Callaway CW, Chumlea WC, Bouchard C, Himes JH, Lohman TG, Martin AD, et al. Circumferences. In: Lohman TG, Roche AF, Martorell R, eds. Anthropometric standardization reference manual. Champaign: Human Kinetics; 1991. p.44-5. 23. Miller SA, Dykes DD, Polesky HF. A simple salting out procedure for extracting DNA from human nucleated cells. Nucleic Acids Res. 1988;16(3):1215. 24. Hixson JE, Vernier DT. Restriction isotyping of human apolipoprotein E by gene amplification and cleavage with HhaI. J Lipid Res. 1990; 31(3):545-8. 25. Frikke-Schmidt R, Nordestgaard BG, Schnohr P, Tybjaerg-Hansen A. Single nucleotide polymorphism in the low-density lipoprotein receptor is associated with a threefold risk of stroke. A case-control and prospective study. Eur Heart J. 2004; 25(11):943-51. 26. Saitou N, Nei M. The neighbor-joining method: a new method for reconstructing phylogenetic trees. Mol Biol Evol. 1987;4(4):406-25. 27. Excoffier L, Laval G, Schneider S. Arlequin (version 3.0): an integrated software package for population genetics data analysis. Evol Bioinform Online. 2007:1:47-50. 28. Moreno JA, López-Miranda J, Pérez-Jiménez F. Influencia de los factores genéticos y ambientales en el metabolismo lipídico y riesgo cardiovascular asociado al gen apõe. Med Clin (Barc). 2006;127(9):343-51. 29. Ferreira CN, Carvalho MG, Fernandes AP, Lima LM, Loures-Valle AA, Dantas J, et al. Comparative study of apolipoprotein-E polymorphism and plasma lipid levels in dyslipidemic and asymptomatic subjects, and their implication in cardio/cerebro-vascular disorders. Neurochem Int. 2010;56(1):177-82. 30. Fuzikawa AK, Peixoto SV, Taufer M, Moriguchi EH, Lima-Costa MF. Association of ApoE polymorphisms with prevalent hypertension in 1406 older adults: the Bambuí Health Aging Study (BHAS). Braz J Med Biol Res. 2008; 41(2):89-94. 31. Bazzaz JT, Nazari M, Nazem H, Amiri P, Fakhrzadeh H, Heshmat R, et al. Apolipoprotein E gene polymorphism and total serum cholesterol level in Iranian population. J Postgrad Med. 2010; 56(3):173-5. 32. Beydoun MA, Beydoun HA, Kaufman JS, An Y, Resnick SM, O’Brien R, et al. Apolipoprotein E ε4 allele interacts with sex and cognitive status to influence all-cause and cause-specific mortality in U.S. older adults. J Am Geriatr Soc. 2013;61(4):525-34. 15. Guardamagna O, Restagno G, Rolfo E, Pederiva C, Martini S, Abello F, et al. The type of LDLR gene mutation predicts cardiovascular risk in children with familial hypercholesterolemia. J Pediatr. 2009; 155(2):199-204.e2. 33. Salazar LA, Hirata MH, Giannini SD, Forti N, Diament J, Lima TM, et al. Seven DNA polymorphisms at the candidate genes of atherosclerosis in Brazilian women with angiographically documented coronary artery disease. Clin Chem Acta. 2000; 300(1-2):139-49. 16. Oliveira PR. Dislipidemia: hipercolesterolemia familiar. [monografia]. Santa Barbara d’Oeste(SP): Anhanguera Educacional S.A; 2010. 34. Davignon J, Gregg RE, Sing CF. Apolipoprotein E polymorphism and atherosclerosis. Arterioesclerosis.1988; 8(1):1-21. Arq Bras Cardiol. 2015; 104(6):468-475 Freitas et al. Genetic polymorphisms and dyslipidemia tracking Original Article Arq Bras Cardiol. 2015; 104(6):468-475 475 Back to the Cover Original Article Circulatory and Ventilatory Power: Characterization in Patients with Coronary Artery Disease Viviane Castello-Simões1, Vinicius Minatel1, Marlus Karsten1,2, Rodrigo Polaquini Simões1, Natália Maria Perseguini1, Juliana Cristina Milan1, Ross Arena3, Laura Maria Tomazi Neves1, Audrey Borghi-Silva1, Aparecida Maria Catai1 Laboratório de Fisioterapia Cardiovascular, Núcleo de Pesquisa em Exercício Físico, Universidade Federal de São Carlos1, São Carlos, SP; Departamento de Fisioterapia, Universidade Federal de Ciências da Saúde de Porto Alegre2, Porto Alegre, RS – Brazil; Departamento de Fisioterapia e Laboratório de Fisiologia Integrativa, Faculdade de Ciências Aplicadas da Saúde, Universidade de Illinois Chicago3, Chicago, IL – USA Abstract Background: Circulatory power (CP) and ventilatory power (VP) are indices that have been used for the clinical evaluation of patients with heart failure; however, no study has evaluated these indices in patients with coronary artery disease (CAD) without heart failure. Objective: To characterize both indices in patients with CAD compared with healthy controls. Methods: Eighty-seven men [CAD group = 42 subjects and healthy control group (CG) = 45 subjects] aged 40–65 years were included. Cardiopulmonary exercise testing was performed on a treadmill and the following parameters were measured: 1) peak oxygen consumption (VO2), 2) peak heart rate (HR), 3) peak blood pressure (BP), 4) peak rate-pressure product (peak systolic HR x peak BP), 5) peak oxygen pulse (peak VO2/peak HR), 6) oxygen uptake efficiency (OUES), 7) carbon dioxide production efficiency (minute ventilation/carbon dioxide production slope), 8) CP (peak VO2 x peak systolic BP) and 9) VP (peak systolic BP/carbon dioxide production efficiency). Results: The CAD group had significantly lower values for peak VO2 (p < 0.001), peak HR (p < 0.001), peak systolic BP (p < 0.001), peak rate-pressure product (p < 0.001), peak oxygen pulse (p = 0.008), OUES (p < 0.001), CP (p < 0.001), and VP (p < 0.001) and significantly higher values for peak diastolic BP (p = 0.004) and carbon dioxide production efficiency (p < 0.001) compared with CG. Stepwise regression analysis showed that CP was influenced by group (R2 = 0.44, p < 0.001) and VP was influenced by both group and number of vessels with stenosis after treatment (interaction effects: R2 = 0.46, p < 0.001). Conclusion: The indices CP and VP were lower in men with CAD than healthy controls. (Arq Bras Cardiol. 2015; 104(6):476-486) Keywords: Exercise; Oxygen Uptake; Cardiopulmonary Exercise; Cardiovascular Disease, Adults. Introduction Cardiopulmonary exercise testing (CPX) is considered the gold standard for evaluating the response to aerobic exertion in patients with cardiovascular diseases to determine the physiological mechanisms of exercise intolerance1. Some indices, such as peak oxygen consumption (VO2), carbon dioxide production eficiency derived from the linear relationship between minute ventilation (VE) and carbon dioxide production (VCO2) (VE/VCO2 slope)2 and oxygen uptake efficiency (OUES), derived from the linear relationship between VO2 and VE3,4, Mailing Address: Viviane Castello-Simões • Universidade Federal de São Carlos – Departamento de Fisioterapia. Rodovia Washington Luis km 235, Jardim Guanabara. Postal Code 13565-905, São Carlos, SP – Brazil E-mail: [email protected] Manuscript received August 8, 2014; revised manuscript January 23, 2015; accepted January 23, 2015. DOI: 10.5935/abc.20150035 476 have been used to assess healthy subjects2,4, patients with heart failure5-8 and with other forms of heart disease9, such as coronary artery disease (CAD)10,11. Circulatory power (CP) is a less frequently assessed variable obtained from CPX and calculated as the product of peak VO2 and peak systolic blood pressure (BP). CP has shown some potential for clinical utility12-15 and has been proposed as a surrogate for cardiac power. This index has also been shown to be an independent predictor of mortality, with a lower CP portending a worse prognosis12,14,15. More recently, Forman et al. (2012)16 introduced and evaluated the prognostic use of a novel index, named ventilatory power (VP), which was calculated by dividing peak systolic BP by the VE/VCO2 slope. According to the authors, better prognosis is reflected by a higher VP value, i.e., greater systolic BP and/or lower VE/VCO2 slope. While these variables have been assessed in heart failure cohorts, we are unaware of any previous study that evaluated the CP and VP indices in CAD patients without heart failure who were managed using standard medication, angioplasty or coronary artery bypass graft (CABG) surgery. Thus, the purpose of this study was to test the hypothesis that both CP and VP would be significantly lower in these CAD patients Castello-Simões et al. Circulatory and ventilatory power Original Article compared with healthy controls; therefore, could provide another potentially valuable measure of cardiopulmonary function in these patients. Methods This is an observational, cross-sectional, comparative study. Participants Men between 40–65 years of age were allocated to two groups: 1) patients with CAD confirmed by cardiac catheterization (CAD-G) and without heart failure and 2) an apparently healthy control group (CG). Subjects in CAD-G were recruited through a local hospital (hemodynamic section) and CG subjects were identified from a registry database in our laboratory and contacted to determine interest. Subjects were invited to participate in this study between June 2008 and April 2013. The inclusion criteria for CAD-G were: 1) CAD patients with or without myocardial infarction (1 month to 3 years since the event) optimally managed using current standard pharmacologic regimens and potentially: a) mechanical or chemical reperfusion and/or b) CABG surgery (6 months to 3 years post-surgery) and 2) preserved left ventricular function with an ejection fraction > 50%. Inclusion criteria for CG were: 1) apparently healthy based on clinical examination and 2) no use of prescription medications. The exclusion criteria for both groups were: 1) body mass index (BMI) ≥ 30 kg/m2, 2) use of tobacco, 3) habitual drinking or illegal drug use, 4) orthopedic limitations, 5) neurological disease, 6) diabetes, 7) uncontrolled systemic arterial hypertension, 8) functional capacity ≤ 4 metabolic equivalents, 9) lung diseases, 10) inappropriate behavior of BP to exertion, 11) malignant ventricular arrhythmia, 12) atrial fibrillation, 13) complex ectopic ventricular beats, 14) supraventricular or sinus tachycardia, 15) 2º and 3º atrioventricular block, 16) fixed frequency pacemaker, and 17) participation in a regular exercise program in the last 6 months. This study was approved by the local Ethics Committee and conducted in accordance with the Declaration of Helsinki (1975). Written informed consent was obtained from each individual before the initiation of the study. Clinical examination Prior to study initiation, all subjects underwent a clinical evaluation to characterize their clinical status. The evaluation comprised: 1) clinical cardiac examination; 2) resting ECG (Ecafix TC 500, São Paulo, São Paulo, Brazil); 3) maximal standard exercise test on a treadmill (DIGISTRESS Vega, Digitronica, Belo Horizonte, Minas Gerais, Brazil); and 4) laboratory measurements: glycemia, hemoglobin, lipid profile, urea, creatinine, and uric acid. Subjects discontinued pharmacological prior to the exercise test, which was conducted by a physician using the Bruce protocol17 in accordance with the American Thoracic Society recommendations1, Symptoms of dyspnea and leg fatigue were assessed using the modified Borg scale18 and all subjects were asked about the occurrence of angina at each stage of the exercise protocol.. After a minimum resting period of 48 h, all eligible subjects performed CPX. Cardiopulmonary exercise testing (CPX) On the same day as CPX, the maximal walking velocity on a treadmill (Master ATL, Inbramed, Porto Alegre, Rio Grande do Sul, Brazil) was determined for all subjects. The starting treadmill speed was set at 3.0 km/h without elevation, with subsequent 0.5 km/h increases in speed every 30 s. At this point, the speed was increased or decreased by 0.1 km/h until the subjects reached a maximal comfortable walking cadence without running19. After determining the maximal walking velocity, symptom-limited CPX was performed using a calibrated ventilatory expired gas unit (CPX-D, Medical Graphics, Saint Paul, Minnesota, United States) according to a ramping protocol: 1) 1 min at rest; 2) an incremental phase, beginning at an initial speed of 0.8 km/h until maximal walking velocity was reached; 3) 0.5% increase in incline grade every 15 s; 4) 1 min of active recovery at 3.0 km/h; and 5) 5 min of passive recovery. Ventilatory expired gases were collected breath-by-breath and calculated as moving means after every eight respiratory cycles (Breeze Suite 6.4.1, Medical Graphics, Saint Paul, Minnesota, United States)19,20. The criteria for test termination were based on current exercise guidelines21,22. Throughout CPX, ECG (12 simultaneous leads) and heart rate (HR) were monitored and registered (WinCardio, Micromed, Brasilia, Distrito Federal, Brazil). Delta of HR was expressed as peak HR minus HR at rest and the predicted maximum HR was calculated as 220 minus age in years. The BP was measured at rest, every 2 min during the test and throughout recovery (BD, São Paulo, São Paulo, Brazil). Perceived exertion (symptoms of dyspnea and leg fatigue) was assessed using the modified Borg scale18 and all subjects were asked about the occurrence of angina and symptoms at each stage of the exercise protocol, according to current exercise guidelines21,22. Peak VO2 and peak respiratory exchange ratio (RER) (defined as the ratio between VCO2 and VO2) were expressed as the highest averaged values observed during the last 30 s of exercise19,23. The VE/VCO2 slope and the OUES were calculated from the initiation of exercise to peak16,22. The VE/VCO2 slope was obtained by analyzing the linear relationship between VE and VCO2, with VE on the y-axis and VCO2 on the x-axis2. The OUES was obtained by analyzing the linear relationship between VO2 and VE, with VO2 on the y-axis and the log‑transformation of VE on the x-axis3,4. Other variables were calculated: 1) peak rate-pressure product (RPP) = product of peak systolic BP and peak HR; 2) peak oxygen pulse = peak VO2 divided by the peak HR; 3) CP = product of peak VO2 and peak systolic BP12 and 4) VP = peak systolic BP divided by the VE/VCO2 slope16. Statistical analysis Based on a pilot study using VP and CP as endpoints (CAD-G = 5 individuals; CG = 5 individuals), a sample size for the current study that would provide sufficient statistical power (β = 0.8) to detect an important difference (α = 0.05) was estimated to be 12 and 21 subjects (VP and CP, respectively) in each group (GPower software package, version 3.1.6, Kiel, Schleswig–Holstein, Germany). The Kolmogorov–Smirnov test was used to investigate the data distribution. Continuous Arq Bras Cardiol. 2015; 104(6):476-486 477 Castello-Simões et al. Circulatory and ventilatory power Original Article quantitative variables were expressed as mean ± standard deviation (SD) and categorical variables as absolute values and percentages. Subjective data (dyspnea and leg fatigue) were expressed as median ± [minimum − maximum]. The unpaired Student’s t-test was used to compare the continuous quantitative variables between CAD-G and CG. Fisher’s exact test was used to compare the categorical variables between groups and the situations after versus before treatment. Stepwise regression analysis was performed to determine the possible influence of group, medications, risk factors (hypertension and dyslipidemia) and number of vessels with stenosis after treatment on the main studied variables (HR, BP, VO2, VE/VCO2 slope, CP and VP). One-way ANOVA (followed by Tukey’s post-hoc test) was performed after subdividing CAD-G according to the type of event and treatment to assess possible differences between subgroups. Pearson correlation analysis was applied to determine the relationships between CP or VP and peak VO2, OUES, RPP and oxygen pulse. The probability of type 1 error occurrence was established at 5% for all tests (p < 0.05). SPSS (version 17.0, SPSS Inc., Chicago, Illinois, United States) was used to perform the statistical analysis. Results Of a total of 97 apparently healthy subjects, we excluded 52 subjects aged < 40 or > 65 years. Forty-five subjects were contacted and recruited for CG. In relation to CAD-G, 54 subjects were recruited; however, 12 were excluded after clinical examination because of BMI ≥ 30 kg/m2 (n = 2), use of tobacco (n = 2), chronic obstructive pulmonary disease (n = 2), presence of cardiac arrhythmias (n = 2), uncontrolled systemic arterial hypertension (n = 1), restenosis after mechanical reperfusion (n = 2), and inability to perform the maximal standard exercise test (n = 1). Thus, our sample consisted of 87 men (45 in CG and 42 in CAD-G). It is important to emphasize that a preliminary analysis (one-way ANOVA) was performed by dividing CAD-G into subgroups according to the type event and treatment. There were no significant differences between subgroups pertinent to any of the studied variables; thus, we pooled the data of all patients in CAD-G. The characteristics of CAD-G and CG are presented in Table 1. No significant difference was found between groups with regard to age (p = 0.087), height (p = 0.318), weight (p = 0.165), and BMI (p = 0.222). In relation to the clinical data of CAD-G before treatment, most patients had two vessels with stenosis (33%), and considering only the 41 subjects with stenosis, the vessel most affected was the anterior descending artery (78%). After treatment, most patients had one-vessel stenosis (48%), and considering only the 29 subjects with stenosis, the vessel most affected was the left circumflex artery (45%). Most subjects in CAD-G (76%) previously suffered a myocardial infarction and had been managed in the following ways: 1) only with standard medication (2%), 2) angioplasty (60%), and 3) CABG (14%). The remaining subjects in the experimental group had CAD with no previous myocardial infarction (24%) and had been managed with: 1) medication only (5%), 2) angioplasty (7%), and 3) CABG (12%) (Table 1). Of the 42 subjects in CAD-G, 15 had a past smoking history and 478 Arq Bras Cardiol. 2015; 104(6):476-486 none was diabetic; furthermore, 38 subjects were diagnosed with systemic arterial hypertension and 39 with dyslipidemia; both risk factors were managed pharmacologically. Of the 45 subjects in CG, three had a past smoking history and none had a diagnosis of diabetes, systemic arterial hypertension or dyslipidemia. None of the CG subjects used any prescribed medication (Table 1). Table 2 shows the comparison between groups in relation to peak variables obtained during the maximal standard exercise test that preceded CPX. CAD-G had significantly lower values for HR (p < 0.001) and systolic BP (p = 0.012) compared with CG. In addition, CAD-G had significantly higher values for diastolic BP (p = 0.016) and symptoms of dyspnea and leg fatigue (p < 0.001 and p = 0.008, respectively) compared with CG. Furthermore, the occurrence of angina (reported by the patients) was present in only 5% of CAD-G (n = 2), whereas it was not present in any subjects in CG. ECG recordings revealed that 7% of CAD-G (n = 3) presented ST segment depression < 2 mm and 5% (n = 2) presented ST segment depression ≥ 2 mm; there was no abnormality in ECG in CG (Table 2). During CPX, the maximum walking velocity obtained was significantly lower in CAD-G (6.2 ± 0.4 km/h, range: 5–7 km/h) than CG (7.1 ± 0.7 km/h, range: 6–8 km/h in CG) (p < 0.001); however, there were no significant differences with respect to maximum grade obtained between groups: 12.8 ± 4.9 % (range: 3.5–22 %) in CAD-G and 11.6 ± 5.6% (range: 1.5–21 %) in CG (p = 0.311). Key CPX variables and aerobic functional classification according to American Heart Association (AHA) guidelines24 for CAD-G and CG are presented in Table 3. There were no significant differences in HR and BP between groups during rest. During peak effort, CAD-G had significantly lower values for VO2 (p < 0.001), HR (p < 0.001), % of predicted maximum HR (p < 0.001), delta of HR (p < 0.001), systolic BP (p < 0.001), RPP (p < 0.001), oxygen pulse (p = 0.008), OUES (p < 0.001), CP (p < 0.001), and VP (p < 0.001) compared with CG. In addition, during peak effort, CAD-G had significantly higher values for diastolic BP (p < 0.001), the VE/VCO2 slope (p = 0.004), symptoms of dyspnea and leg fatigue (p = 0.008 and p < 0.001, respectively) compared with CG. Furthermore, angina (reported by the patients) occurred only in 2% of CAD-G (n = 1) and was not present in any subjects in CG. There were no ECG abnormalities in either group (CAD-G and CG) during CPX (Table 3). With regard to the aerobic functional classification according to AHA guidelines24, Table 3 shows that the majority of patients of CAD-G had a weak aerobic classification (53%), while in CG slightly more than half of subjects had a regular level of aerobic classification (53%). Stepwise regression analysis was performed to determine the possible influence of group, medications, risk factors (hypertension and dyslipidemia), and number of vessels with stenosis after treatment on CPX variables of interest. We found that none of the variables were affected by risk factors. However, the following influences were determined: 1) peak VO2 was influenced by group and medications (interaction effects: R2 = 0.46, β of group = 0.95 and β of medications = −0.35, p < 0.001); 2) peak systolic BP was influenced only by medications (R2 = 0.11, β = 0.34, p < 0.001); 3) the Castello-Simões et al. Circulatory and ventilatory power Original Article Table 1 – Characteristics of CAD-G and CG CAD-G (n = 42) CG (n = 45) p value 54.3 ± 6.6 53.9 ± 6.4 0.087 Height, m 1.70 ± 0.07 1.73 ± 0.13 0.318 Weight, kg 79.0 ± 12.3 76.9 ± 9.9 0.165 27 ± 3.9 26 ± 5.9 0.222 63.9 ± 7.1 - - Age, years Anthropometry Body mass index, kg/m2 Cardiac function LVEF, % Vessels with stenosis, n (%) Before treatment (n = 42) After treatment (n = 42) 1 (2) 13 (31) - < 0.001 One diseased vessel 10 (24) 20 (48) - 0.039 Two diseased vessels 14 (33) 6 (14) - 0.071 Three diseased vessels 8 (19) 3 (7) - 0.194 Multivessel (> 3 diseased vessels) 9 (22) 0 - 0.002 Before treatment (n = 41) After treatment (n = 29) Without stenosis Location of stenosis (> 50%), n (%) Anterior descending artery 32 (78) 8 (28) - < 0.001 Left circumflex artery 26 (63) 13 (45) - 0.147 Right coronary artery 24 (58) 10 (34) - 0.056 Diagonal arteries 8 (19) 6 (21) - 1.000 Marginal arteries 4 (10) 1 (3) - 0.394 CAD characteristics, n (%) With myocardial infarction Treated only with medication 1 (2) - - Treated with angioplasty 25 (60) - - Treated with CABG 6 (14) - - 2 (5) - - Treated with angioplasty 3 (7) - - Treated with CABG 5 (12) - - 15 (36) 3 (7) < 0.001 0 0 - Arterial hypertension 38 (90) 0 < 0.001 Dyslipidemia 39 (93) 0 < 0.001 Without myocardial infarction Treated only with medication Risk factors, n (%) History of smoking Diabetes Medications, n (%) Beta-blocker 37 (88) - - ACE inhibitor 24 (57) - - Diuretic 12 (29) - - Lipid-lowering 39 (93) - - Antiplatelet/ anticoagulant 42 (100) - - Data are presented as mean ± SD or absolute values (%). CAD-G: coronary arterial disease group; CG: control group, n: number of individuals; LVEF: left ventricular ejection fraction; CABG: coronary artery bypass grafting; (-): not applicable; ACE: angiotensin converting enzyme. Unpaired Student’s t-test and Fisher’s exact test. Arq Bras Cardiol. 2015; 104(6):476-486 479 Castello-Simões et al. Circulatory and ventilatory power Original Article Table 2 – Peak variables obtained during maximal standard exercise testing for clinical evaluation in CAD-G and CG CAD-G (n = 42) CG (n = 45) p value HR, bpm 144.9 ± 20.0 169.9 ± 19.1 < 0.001 Systolic BP, mmHg 175.7 ± 26.5 189.5 ± 22.3 0.012 Diastolic BP, mmHg 91.3 ± 11.8 85.0 ± 11.2 0.016 Symptoms of dyspnea (0–10) 7.0 [2 - 10] 4.0 [2 - 6] < 0.001 Leg fatigue (0–10) 6.0 [0 - 10] 4.5 [2 - 5] 0.008 Angina, n (%) 2 (5) 0 0.230 ST segment depression < 2 mm, n (%) 3 (7) 0 0.108 ST segment depression ≥ 2 mm, n (%) 2 (5) 0 0.230 Data are presented as mean ± SD, median [minimum - maximum] or absolute values (%). CAD-G: coronary artery disease group; CG: control group; n: number of subjects; HR: heart rate; BP: blood pressure. Unpaired Student’s t-test and Fisher’s exact test. VE/VCO2 slope was influenced only by group (R2 = 0.08, β = 0.30, p < 0.001); 4) CP was influenced only by group (R2 = 0.44, β = 0.67, p < 0.001); and 5) VP was influenced by group and number of vessels with stenosis after treatment (interaction effects: R2 = 0.46, β of group = 0.62 and β of number of vessels with stenosis after treatment = −0.30, p < 0.001). Figure 1 illustrates a significant correlation between both CP and VP and peak VO2, considering the subjects by aerobic functional classification according to AHA guidelines24. For better visualization of Figure 1, only those with a weak (n = 22) and regular level of classification (n = 14) in CAD-G and only those with regular (n = 24) and good level of classification (n = 15) in CG were included in the statistical analysis and presented in this figure. With respect to CP, there was a strong positive correlation with peak VO2 (Figure 1A, r = 0.91, p < 0.001), while VP showed a moderate positive correlation with peak VO2 (Figure 1B, r = 0.43, p < 0.001). Figure 2 illustrates the significant correlations between CP and VP and other CPX indices (OUES, RPP, and oxygen pulse), considering the entire study cohort. CP exhibited a strong positive correlation with OUES (Figure 2A, r = 0.75, p < 0.001) and peak RPP (Figure 2C, r = 0.74, p < 0.001) and moderate positive correlation with peak oxygen pulse (Figure 2E, r = 0.59, p < 0.001); with regard to VP there was a moderate positive correlation with OUES (Figure 2B, r = 0.55, p < 0.001), peak RPP (Figure 2D, r = 0.58, p < 0.001) and peak oxygen pulse (Figure 2F, r = 0.55, p < 0.001). Discussion The main findings from this study were: 1) CAD patients without heart failure under current standard pharmacologic regimens, angioplasty, or surgical management had lower CP and VP values compared with CG; 2) the indices CP and VP correlated positively with VO2 according to aerobic functional classification as per AHA guidelines24; and 3) the response of CPX and the metabolic, ventilator, and cardiovascular variables demonstrated lower functional capacity and poorer exercise response in subjects with CAD. To the best of our knowledge, this is the first study to introduce CP and VP indices in the functional evaluation of subjects with CAD without heart failure compared with 480 Arq Bras Cardiol. 2015; 104(6):476-486 apparently healthy controls. Thus, our findings have a potential clinical relevance given that these indices may be used to assess the functional significance of the disease process. The potential advantage of CP and VP indices is that both are simple and noninvasive and synergistically combine singular indices related to cardiopulmonary integrity and health. Sample characteristics As listed in Table 1, the groups did not differ in terms of age; this is an important consideration as it is known that aging affects peak VO2 25,26. In addition, we did not include obese individuals because they present with abnormal exercise responses unique to body habitus, which could have confounded our results27,28. We included patients with controlled systemic arterial hypertension and controlled dyslipidemia in CAD-G; however, we observed (using stepwise regression analysis) that these factors did not influence the CPX response. Cardiopulmonary exercise testing (CPX) CP and VP were lower in CAD-G than in CG; the same observation was applicable to the following peak variables obtained during CPX: VO2, HR, % of predicted maximum HR, delta of HR, systolic BP, RPP, oxygen pulse, and OUES. Moreover, higher values of peak diastolic BP and the VE/VCO2 slope were found in CAD-G. Pharmacologic management, such as angiotensin-converting enzyme inhibitors, diuretics, and particularly beta-blockers, may contribute to the exercise response because CAD-G presented with lower values of peak systolic BP, peak HR, and peak VO2 in relation to CG during CPX. In addition, during the maximal standard exercise test performed with suspended pharmacological therapy, CAD-G presented with a higher peak HR (approximately 7%) than CPX, in which the subjects were undergoing pharmacological therapy. Although these medications may have influenced our results, they are considered standard of care therapy for these patients29,30, and beta-blocker withdrawal can increase the risk of heart events31. Because VO2 is present in the formula of CP and BP is present in the formula of CP and VP, it is important to consider that medications Castello-Simões et al. Circulatory and ventilatory power Original Article Table 3 – Variables obtained during cardiopulmonary exercise testing and aerobic functional classification according to AHA guidelines in CAD-G and CG CAD-G (n = 42) CG (n = 45) p value 65.9 ± 11 69.7 ± 11 0.110 Systolic BP, mmHg 120.7 ± 10.7 117.4 ± 18.7 0.298 Diastolic BP, mmHg 82.6 ± 7.6 79.7 ± 9.6 0.103 Rest HR, bpm Peak VO2, ml.kg−1 min−1 22.9 ± 4.8 32.7 ± 6.6 < 0.001 RER 1.11 ± 0.07 1.12 ± 0.08 0.738 HR, bpm 135.4 ± 22.2 165.0 ± 18.7 < 0.001 % of predicted maximum HR 81.8 ± 13.4 97.7 ± 9.9 < 0.001 Delta of HR, bpm 52.7 ± 23.1 85.2 ± 20.7 < 0.001 Systolic BP, mmHg 169.8 ± 24.6 186.1 ± 19.8 < 0.001 Diastolic BP, mmHg 88.3 ± 9.9 80.1 ± 10.7 < 0.001 23052 ± 4889 30713 ± 4800 < 0.001 Oxygen pulse, mL/beat 13.5 ± 2.9 15.4 ± 3.8 0.008 VE/VCO2 slope 31.6 ± 5.2 28.6 ± 4.4 0.004 RPP, mmHg.bpm OUES 1963 ± 449.7 2555 ± 552 < 0.001 CP, mmHg.ml.kg−1 min−1 3902 ± 1016 6099 ± 1403 < 0.001 VP, mmHg 5.5 ± 1.2 6.6 ± 1.3 < 0.001 Symptoms of dyspnea (0–10) 6.0 [4 - 8] 4.5 [2 - 5] 0.008 Leg fatigue (0–10) 7.0 [4 - 9] 4.5 [2 - 6] < 0.001 1 (2) 0 0.230 ST segment depression < 2 mm, n (%) 0 0 - ST segment depression ≥ 2 mm, n (%) 0 0 - Very weak 6 (14) 1 (2) 0.052 Weak 22 (53) 3 (7) < 0.001 Regular 14 (33) 24 (53) 0.083 Good 0 15 (33) < 0.001 Excellent 0 2 (5) 0.494 Angina, n (%) Aerobic functional classification, n (%) Data are presented as mean ± SD, median [minimum - maximum] or absolute values (%). CPX: cardiopulmonary exercise testing; AHA: American Heart Association; CAD-G: coronary artery disease group; CG: control group; n: number of subjects; HR: heart rate; BP: blood pressure; VO : oxygen uptake; RER: respiratory exchange ratio; % of predicted maximum HR: % of 220 minus age; Delta of HR peak HR minus HR at rest; RPP: rate-pressure product; VE/VCO2 slope: linear relation between minute ventilation, and carbon dioxide production; OUES: linear relationship between oxygen uptake and minute ventilation, CP: circulatory power; VP: ventilatory power. Unpaired Student’s t-test and Fisher’s exact test. 2 influenced peak VO2 and peak systolic BP (as indicated by stepwise regression analysis), but did not influence CP and VP. Furthermore, the group influenced peak VO2, the VE/VCO2 slope, CP, and VP, while the number of vessels with stenosis after treatment influenced the VP. Thus, we believe that the lower values of CP and VP observed during CPX in CAD-G are related to standard medications, level of aerobic capacity and characteristics of CAD and that the reduction of VP in this population may also be related to number of vessels with stenosis after treatment. One way to quantify exercise performance is by measuring peak VO2. In the present study the lower values of this variable observed in CAD-G reinforce the role of CAD in a worse CPX response10, which was also directly related to the ventilatory inefficiency observed in this group (higher VE/VCO2 slope and lower OUES). High values of the VE/VCO2 slope are often related to a worsening pulmonary hemodynamic profile and increased chemoreceptor and ergoreceptor activation, as well as decreased autonomic modulation and cardiovascular function7. Lower OUES Arq Bras Cardiol. 2015; 104(6):476-486 481 Castello-Simões et al. Circulatory and ventilatory power Original Article Figure 1 – Circulatory power (CP) and ventilatory power (VP) correlated with oxygen uptake (VO2) by aerobic functional classification according to American Heart Association guidelines. Legend: (ο) coronary artery disease group (CAD-G) with weak functional classification, (•) CAD-G with regular functional classification, (∆) control group (CG) with regular functional classification and (▲) CG with good functional classification. Pearson correlation analysis. values indicate that the extraction and utilization of oxygen is impaired because this variable is strongly correlated to VO 2 3,4,10. Furthermore, we observed in the present study that RPP and oxygen pulse were lower in CAD-G at peak CPX. RPP has been used as a relevant parameter in evaluating ventricular function, and high values at peak exercise are most likely related to good ventricular function and no ischemia32,33. In addition, the oxygen pulse indicates the amount of oxygen consumed per heart beat, which reflects the efficiency of the cardiovascular system and may provide prognostic information in patients with CAD34,35. Another interesting and novel finding of this study was that subjects with a lower peak VO2 presented with lower indices CP and VP that correlated with the aerobic functional classification according to AHA guidelines 24. A recent prospective study36 that evaluated the associations between exercise test parameters and all-cause mortality in patients without previous cardiovascular disease showed that poor exercise tolerance (determined by the observed duration of exercise in relation to the predicted duration) is associated with greater mortality risk. In our cross-sectional comparative study we observed that CP and VP positively correlated (strong and moderate correlation, respectively) with aerobic functional classification evaluated by peak VO2. Cohen-Solal et al. (2002)12 longitudinally evaluated (mean follow-up 25 ± 10 months) 175 heart failure patients who were subjected to an incremental CPX. Their study showed that CP was predictive of prognosis and that the combination of VO2 and systolic BP (through the CP index) strengthens the prognostic value of CPX, particularly in subjects with low peak VO2 and peak BP. Similar to the previous report, Forman et al. (2012)16 evaluated the prognostic use of VP in a longitudinal study (mean follow-up 4 years) with 875 heart failure patients submitted to CPX. The authors showed that VP was independently predictive of cardiac events compared with standard CPX 482 Arq Bras Cardiol. 2015; 104(6):476-486 indices (i.e., peak VO2 and the VE/VCO2 slope); furthermore, in a multivariate analysis, combined CP and VP provided even better prognostic discrimination. Although traditional variables obtained by CPX, such as VO2, systolic BP, and the VE/VCO2 slope, reflect the aerobic capacity, hemodynamic control and carbon dioxide production eficiency efficiency, respectively, CP and VP are indices that combine these variables. VP, as an index that combines systemic hemodynamics with carbon dioxide production efficiency during exercise, and CP as an index that combines central and peripheral components of cardiac stroke work, appear to both portend important information regarding disease severity and prognosis12,16,37. Recently, Borghi-Silva el al (2014)37 assessed the relationship between VP and key measures obtained using Doppler echocardiography in patients with heart failure and reduced ejection fraction; their results showed that lower values of VP translate into a very unfavorable phenotype characterized by a lower peak VO2 and cardiac output response. The current study is a cross-sectional analysis with the goal of characterizing these indices in a CAD cohort under current standard pharmacologic regimens, angioplasty, or surgical management without heart failure. Our findings demonstrate that CP and VP are abnormal in CAD patients compared with healthy controls, and are related not only to standard medication but also to the level of aerobic capacity and characteristics of CAD; moreover, VP is related to the number of vessels with stenosis after treatment. Future work is needed to determine the prognostic utility of CP and VP in patients with CAD and establish whether both indices perform similarly to what has been found in patients with heart failure12,14,16. Study limitations This investigation is characterized by an initial exploration of CP and VP indices in males with CAD; however, it has some limitations. First, although the literature 12,16,37 Castello-Simões et al. Circulatory and ventilatory power Original Article Figure 2 – Circulatory power (CP) and ventilatory power (VP) correlated with OUES, RPP and oxygen pulse. Legend: (ο) coronary arterial disease group (CAD-G), (•) control group (CG), OUES linear relationship between oxygen uptake and minute ventilation, RPP rate-pressure product. Pearson correlation analysis. indicates that CP and VP appear to be important prognostic markers in patients with heart failure, the cross-sectional nature and relatively small sample size of the current study did not allow us to expand upon prognostic utility. Therefore, additional prospective evaluations in this population are needed to determine the usefulness of these indices as prognostic markers. In relation to cardiac function, the CAD group was characterized only by left ventricular ejection fraction because 50% of patients were evaluated by ventriculography and 50% by echocardiogram. Women were not included in this study because the selected age could include both women with regular menstrual cycle (with and without use of contraceptives) and women in the postmenopausal stage (with and without use of hormone replacement therapy) and these differences could influence our results38,39. Although the pharmacologic management of systemic arterial hypertension by angiotensin converting enzyme inhibitors, diuretics, and particularly beta-blockers may have influenced the behavior of CP and VP (as well as of other indices obtained from CPX), medication cessation is not possible because it is mandatory therapy for some patients. Future studies including a control group of systemic Arq Bras Cardiol. 2015; 104(6):476-486 483 Castello-Simões et al. Circulatory and ventilatory power Original Article arterial hypertension patients without CAD (with similar pharmacologic management to our study) could eliminate the possible influence of medications on studied variables. Conclusions The CP and VP indices were lower in men with CAD, without heart failure, and under current standard pharmacologic regimens, angioplasty, or surgical management than healthy controls, demonstrating a poorer cardiopulmonary function in this population. Our results suggest that both CP and VP may hold value as screening tools in assessing the functional significance of disease, exercise tolerance, and may consequently assist in the prescription of physical training in this population when used individually or complementarily to other indices currently attained by CPX. In fact, a multivariate approach including indices related to both central and peripheral function would likely provide a more comprehensive evaluation of exertional physiology. Future investigations are needed to evaluate if lower CP and VP values are due only to the CAD or to the use of standard pharmacologic regimens, as well as to verify the prognostic value of these indices in this patient population. Acknowledgments The authors would like to thank the patients for their effort and enthusiastic cooperation throughout the study and the physicians Sérgio Luiz Berti and João Orávio de Freitas Jr. for support with the hemodynamic section patients. Author contributions Conception and design of the research:Castello-Simões V, Catai AM. Acquisition of data:Castello-Simões V, Minatel V, Karsten M, Simões RP, Perseguini NM, Milan JC, Neves LMT. Analysis and interpretation of the data: Castello-Simões V, Minatel V, Karsten M, Simões RP, Perseguini NM, Milan JC, Arena R, Neves LMT, Catai AM. Statistical analysis: Castello-Simões V, Minatel V, Karsten M, Simões RP, Neves LMT, Borghi-Silva A. Obtaining financing: Castello-Simões V, Karsten M, Perseguini NM, Catai AM. Writing of the manuscript:Castello-Simões V, Karsten M, Simões RP, Catai AM. Critical revision of the manuscript for intellectual content: Castello-Simões V, Simões RP, Arena R, Borghi-Silva A, Catai AM. Potential Conflict of Interest No potential conflict of interest relevant to this article was reported. Sources of Funding This study was funded by Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP), São Paulo/SP/Brasil (processo: 2010/52070-4); Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), Brasília/DF/Brasil; Conselho Nacional de Desenvolvimento Científico e Tenológico (CNPq), Brasília/DF/Brasil (processo: 483945/2007-2). Study Association This article is part of the thesis of Doctoral submitted by Viviane Castello Simões, from Universidade Federal de São Carlos. References 1. American Thoracic Society; American College of Chest Physicians. ATS/ ACCP. Statement on cardiopulmonary exercise testing. Am J Respir Crit Care Med. 2003;167(2):211-77. 8. Arena R, Myers J, Guazzi M. The clinical and research applications of aerobic capacity and ventilatory efficiency in heart failure: an evidence-based review. Heart Fail Rev. 2008;13(2):245-69. 2. Sun XG, Hansen EJ, Garatachea N, Storer TW, Wasserman K. Ventilatory efficiency during exercise in healthy subjects. Am J Respir Crit Care Med. 2002;166(11):1443-8. 9. Tsurugaya H, Adachi H, Kurabayashi M, Ohshima S, Taniguchi K. Prognostic impact of ventilatory efficiency in heart disease patients with preserved exercise tolerance. Circ J. 2006; 70(10):1332-6. 3. 10. Van de Veire NR, Van Laethem C, Philippé J, De Winter O, De Backer G, Vanderheyden M, et al. VE/VCO2 slope and oxygen uptake efficiency slope in patients with coronary artery disease and intermediate peak VO2. Eur J Cardiovasc Prev Rehabil. 200613(6):916-23. Baba R, Nagashima M, Masahiko G, Nagano Y, Yokota M, Tauchi N, et al. Oxygen uptake efficiency slope: a new index of cardiorespiratory functional reserve derived from the relation between oxygen uptake and minute ventilation during incremental exercise. J Am Coll Cardiol. 1996;28(6):1567-72. 4. Baba R, Kubo N, Morotome Y, Iwagaki S. Reproducibility of the oxygen uptake efficiency slope in normal healthy subjects. J Sports Med Phys Fitness. 1999;39(3):202-6. 5. Arena R, Humphrey R, Peberdy MA. Prognostic ability of VE/VCO2 slope calculations using different exercise test time intervals in subjects with heart failure. Eur J Cardiovasc Prev Rehabil. 2003;10(6):463-8. 484 6. Van Laethem C, Bartunek J, Goethals M, Nellens P, Andries E, Vanderheyden M. Oxygen uptake efficiency slope, a new submaximal parameter in evaluating exercise capacity in chronic heart failure patients. Am Heart J. 2005;149(1):175-80. 7. Arena R, Myers J, Hsu L, Peberdy MA, Pinkstaff S, Bensimhon D, et al. The minute ventilation/carbon dioxide production slope is prognostically superior to the oxygen uptake efficiency slope. J Card Fail. 2007;13(6):462-9. Arq Bras Cardiol. 2015; 104(6):476-486 11. Baba R, Tsuyuki K, Yano H, Ninomiya K, Ebine K. Robustness of the oxygen uptake efficiency slope to exercise intensity in patients with coronary artery disease. Nagoya J Med Sci. 2010;72(1-2):83-9. 12. Cohen-Solal A, Tabet JY, Logeart D, Bourgoin P, Tokmakova M, Dahan M. A noninvasively determined surrogate of cardiac power (‘circulatory power’) at peak exercise is a powerful prognostic factor in chronic heart failure. Eur Heart J. 2002;23(10):806-14. 13. Giardini A, Specchia S, Berton E, Sangiorgi D, Coutsoumbas G, Gargiulo G, et al. Strong and independent prognostic value of peak circulatory power in adults with congenital heart disease. Am Heart J. 2007;154(3):441-7. 14. Jaussaud J, Blanc P, Derval N, Bordachar P, Courregelongue M, Roudaut R, et al. Ventilatory response and peak circulatory power: new functional markers of response after cardiac resynchronization therapy. Arch Cardiovasc Dis. 2010;103(3):184-91. Castello-Simões et al. Circulatory and ventilatory power Original Article 15. Madan N, Beachler L, Konstantinopoulos P, Worley S, Sun Z, Latson LA. Peak circulatory power as an indicator of clinical status in children after Fontan procedure. Pediatr Cardiol. 2010; 31(8):1203-8. 16. Forman DE, Guazzi M, Myers J, Chase P, Bensimhon D, Cahalin LP, et al. A novel index that enhances prognostic assessment of patients with heart failure. Circ Heart Fail. 2012;5(5):621-6. 17. Bruce RA, Kusumi F, Hosmer D. Maximal oxygen intake and nomographic assessment of functional aerobic impairment in cardiovascular disease. Am Heart J.1973;85(4):546-62. 18. Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14(5):377-81. 19. Neves LMT, Karsten M, Neves VR, Beltrame T, Borghi-Silva A, Catai AM. Relationship between inspiratory muscle capacity and peak exercise. Heart Lung. 2012;41(2):137-45. 20. Neves LMT, Karsten M, Neves VR, Beltrame T, Borghi-Silva A, Catai AM. Respiratory muscle endurance is limited by lower ventilatory efficiency in post-myocardial infarction patients. Braz J Phys Ther. 2014;18(1):1-8. 21. Mezzani A, Agostoni P, Cohen-Solal A, Corrà U, Jegier A, Kouidi E, et al. Standards for the use of cardiopulmonary exercise testing for the functional evaluation of cardiac patients: a report from the Exercise Physiology Section of the European Association for Cardiovascular Prevention and Rehabilitation. Eur J Cardiovasc Prev Rehabil. 2009;16(3):249-67. 22. Balady GJ, Arena R, Sietsema K, Myers J, Coke L, Fletcher GF, et al. Clinician’s Guide to cardiopulmonary exercise testing in adults: a scientific statement from the American Heart Association. Circulation. 2010;122(2):191-225. 23. Higa MN, Silva E, Neves VF, Catai AM, Gallo L Jr, Silva de Sá MF. Comparison of anaerobic threshold determined by visual and mathematical methods in healthy women. Braz J Med Biol Res. 2007;40(4):501-8. 24. American Heart Association. Committee on Exercise: exercise testing and training of apparently healthy individuals: a handbook for physicians. Dallas;1972. 25. Woo JS, Derleth C, Stratton JR, Levy WC. The influence of age, gender, and training on exercise efficiency. J Am Coll Cardiol. 2006;47(5):1049-57. 26. Simões RP, Bonjorno JC Jr, Beltrame T, Catai AM, Arena R, Borghi-Silva A. Slower heart rate and oxygen consumption kinetic responses in the on- and off-transient during a discontinuous incremental exercise: effects of aging. Braz J Phys Ther. 2013;17(1):69-76. 27. Vanhecke TE, Franklin BA, Miller WM, de Jong AT, Coleman CJ, McCullough PA. Cardiorespiratory fitness and sedentary lifestyle in the morbidly obese. Clin Cardiol. 2009; 32(3):121-4. 28. Castello-Simões V, Polaquini Simões R, Beltrame T, Bassi D, Catai AM, Arena R, et al. Effects of aerobic exercise training on variability and heart rate kinetic during submaximal exercise after gastric bypass surgery-a randomized controlled trial. Disabil Rehabil. 2013; 35(4):334-42. 29. Tabet JY, Meurin P, Ben Driss AB, Thabut G, Weber H, Renaud N, et al. Determination of exercise training heart rate in patients on B-blockers after myocardial infarction. Eur J Cardiovasc Prev Rehabil. 2006;13(4):538-43. 30. Giallauria F, Galizia G, Lucci R, D’Agostino M, Vitelli A, Maresca L, et al. Favourable effects of exercise-based Cardiac Rehabilitation after acute myocardial infarction on left atrial remodeling . Int J Cardiol. 2010;136(3):300-6. 31. Fallahi B, Beiki D, Akbarpour S, Gholamrezanezhad A, Fard-Esfahani A, Akhzari F, et al. Withholding or continuing beta-blocker treatment before dipyridamole myocardial perfusion imaging for the diagnosis of coronary artery disease? A randomized clinical trial. Daru. 2013; 21(1):8. 32. Gobel FL, Nordstron LA, Nelson RR, Jorgensen CR, Wang Y. The ratepressure product as an index of myocardial oxygen consumption during exercise in patients with angina pectoris. Circulation. 1978;57(3):549-56. 33. Fornitano LD, Godoy MF. Increased rate-pressure product as predictor for the absence of significant obstructive coronary artery disease in patients with positive exercise test. Arq Bras Cardiol. 2006;86(2):136-44. 34. Patterson RP, Remole WD. The response of the oxygen pulse during a stress test in patients with coronary artery disease. Cardiology. 1981;67(1):52-62. 35. Laukkanen JA, Kurl S, Salonen JT, Lakka TA, Rauramaa R. Peak oxygen pulse during exercise as a predictor for coronary heart disease and all cause death. Heart. 2006;92(9):1219-24. 36. Dhoble A, Lahr BD, Allison TG, Kopecky SL. Cardiopulmonary fitness and heart rate recovery as predictors of mortality in a referral population. J Am Heart Assoc. 2014;3(2):e000559. 37. Borghi-Silva A, Labate V, Arena R, Bandera F, Generati G, Pellegrino M, et al. Exercise ventilatory power in heart failure patients: functional phenotypes definition by combining cardiopulmonary exercise testing with stress echocardiography. Int J Cardiol. 2014;176(3):1348-9. 38. Neves VF, Silva de Sá MF, Gallo L Jr, Catai AM, Martins LE, Crescêncio JC, et al. Autonomic modulation of heart rate of young and postmenopausal women undergoing estrogen therapy. Braz J Med Biol Res. 2007;40(4):491-9. 39. Perseguini NM, de Medeiros Takahashi AC, Milan JC, dos Santos PR, Neves VF, et al. Effect of hormone replacement therapy on cardiac autonomic modulation. Clin Aut Res. 2014;24(2):63-70. Arq Bras Cardiol. 2015; 104(6):476-486 485 Castello-Simões et al. Circulatory and ventilatory power Original Article 486 Arq Bras Cardiol. 2015; 104(6):476-486 Back to the Cover Original Article Blood Pressure and Hemodynamic Adaptations after a Training Program in Young Individuals with Down Syndrome Bruna Barboza Seron, Karla Fabiana Goessler, Everaldo Lambert Modesto, Eloise Werle Almeida, Márcia Greguol Universidade Estadual de Londrina, Londrina, PR – Brazil Abstract Background: Cardiovascular diseases affect people worldwide. Individuals with Down Syndrome (DS) have an up to sixteen-time greater risk of mortality from cardiovascular diseases. Objective: To evaluate the effects of aerobic and resistance exercises on blood pressure and hemodynamic variables of young individuals with DS. Methods: A total of 29 young individuals with DS participated in the study. They were divided into two groups: aerobic training (AT) (n = 14), and resistance training (TR) (n = 15). Their mean age was 15.7 ± 2.82 years. The training program lasted 12 weeks, and had a frequency of three times a week for AT and twice a week for RT. AT was performed in treadmill/ bicycle ergometer, at an intensity between 50%-70% of the HR reserve. RT comprised nine exercises with three sets of 12 repetition-maximum. Systolic blood pressure (SBP), diastolic blood pressure (DBP), mean blood pressure (MBP) and hemodynamic variables were assessed beat-to-beat using the Finometer device before/after the training program. Descriptive analysis, the Shapiro-Wilk test to check the normality of data, and the two-way ANOVA for repeated measures were used to compare pre- and post-training variables. The Pearson’s correlation coefficient was calculated to correlate hemodynamic variables. The SPSS version 18.0 was used with the significance level set at p < 0.05. Results: After twelve weeks of aerobic and/or resistance training, significant reductions in variables SBP, DBP and MBP were observed. Conclusion: This study suggests a chronic hypotensive effect of moderate aerobic and resistance exercises on young individuals with DS. (Arq Bras Cardiol. 2015; 104(6):487-492) Keywords: Arterial Pressure / physiology; Hemodynamic / physiology; Heart Defects / congenital; Down Syndrome; Adolescent; Resistance Training. Introduction Cardiovascular disease is the major cause of mortality worldwide and although cardiovascular events are more frequent after the fifth decade of life, there is evidence that their precursors have origin in childhood1. Individuals with Down syndrome (DS) show an up to sixteen-time higher risk of mortality for cardiovascular diseases2. While the incidence of congenital heart defects in the general population is of 0.8%, approximately 40%-65% of individuals with DS develop the disease3. The development of congenital heart defects is multifactorial and under the interference of molecular and morphological signaling. Additionally, the incidence of atrioventricular and ventricular septal defects is of 45% and 35% in patients with DS 3, respectively. Mailing Address: Márcia Greguol • Universidade Estadual de Londrina - Rodovia Celso Garcia Cid - Pr 445 Km 380, s/n - Campus Universitário, Postal Code 86057-970, Londrina, PR – Brazil E-mail: [email protected] Manuscript received September 11, 2014; revised manuscript received January 21, 2015; accepted January 22, 2015. DOI: 10.5935/abc.20150033 487 Also, the risk of persistent pulmonary hypertension in neonates is 5.2% higher for children with DS in comparison to the general population3,4. Among the major cardiovascular risk factors, we should point out high blood pressure (BP) and sedentary lifestyle. Some studies have proven that both risk factors show strong tracking from childhood to adulthood5-8 and this suggests that there should be incentives for their reduction from early ages. BP control is related to lifestyle changes including increasing physical activity 9. Few studies correlating the effect of physical training on the cardiovascular response of individuals with DS are available; therefore, the specificities of physical exercises should be carefully verified for this population. Kelley et al 10 conducted a meta-analysis involving non-disabled children and adolescents and demonstrated that short-term physical exercises did not lead to reductions in resting SBP and DBP. Nonetheless, McDonnell et al 11 showed that regular physical exercise is associated with a beneficial vascular profile, which is explained by lower large artery stiffness in older individuals, but lower peripheral vascular resistance in young individuals. Seron et al. Blood Pressure and Young Individuals with Down Syndrome Original Article The literature points to the benefits of an active lifestyle for the general population. However, the population with DS has a less active lifestyle than do individuals without DS. This may be harmful to the health and autonomy of this population12,13. The increase in life expectancy of this population makes the prevention of secondary diseases increasingly more important. Therefore, we hypothesized that physical training (aerobic and resistance) could reduce blood pressure levels and thus improve and/or prevent the development of cardiovascular diseases in individuals with DS. For this reason, knowing the importance of a physically active lifestyle for BP control and for the prevention of cardiovascular diseases, the objective of this study was to investigate the effects of aerobic and resistance training on BP values and hemodynamic variables in young individuals with DS after the training period. Methods Participants Twenty nine young individuals of both genders (20 boys and 9 girls) with Down syndrome and a mean age of 15.7 ± 2.82 years participated in the study. Subject selection was made by inviting all young individuals with DS aged between 12 and 20 years from 3 institutions in the city of Londrina/State of Parana/ Brazil, which provide care for intellectually disabled individuals. Those presenting with orthopedic or cardiac problems; using medications that could affect the heart rate; and those presenting with severe or profound intellectual disability that could affect their understanding and/or ability to perform the procedures were excluded from the study. After receiving explanations on the terms of the research, their parents and/or guardians gave written informed consent. The study was approved by the Research on Humans Ethics Committee, Universidade Estadual de Londrina, under opinion number 93.680/2012. The participants were divided into two groups, according to their availability to attend the physical exercise program: aerobic training group (n = 14, of which 4 were girls and 10 were boys); and resistance training group (n = 15, of which 5 were girls and 10 were boys). Initially, there was a control group; however, the individuals from this group did not attend the second assessment visit, and therefore the control group was excluded from the analysis. Training programs The aerobic and resistance training programs consisted of 12 weeks with 50-minute-duration sessions. The aerobic training was performed three times a week in a treadmill and bicycle ergometer (15 minutes each), at an intensity between 50% and 70% of the HR reserve for 30 minutes, preceded by a 10-minute warm- up (articulations and stretching) and followed by 10 more minutes of recovery (stretching). The intensity was monitored by a Polar FT2 heart rate monitor. The HRmax used for the calculation of HR reserve was obtained by means of a maximal exercise test validated for individuals with DS14. This test started at a 4 km/h speed and 0% inclination for two minutes. Every two minutes the treadmill inclination was increased by 2.5% up to 12.5%. Thereafter, the speed was raised by 1.6 km/h at every minute until volitional fatigue. The test was performed on a treadmill (INBRAMED, model 10.200) with the use of a portable metabolic measurement system (Cosmed k4b², Italy). The resistance training consisted of 9 exercises performed in three sets of 12 repetition-maximum, with a 1-minute interval between the sets and 3-minute intervals between exercises. The following series of exercises was proposed: chest press machine; leg extension machine; lat pull down; biceps cable curl; standing leg curl with ankle weights; cable triceps extension; calf raises with ankle weights; dumbbell front raise and abdominal exercises. The two first sessions were for adaptation to the exercise training with low loads and, subsequently, the load used was estimated by observing the participant’s ability to perform the exercise in 12 repetitions. Load progression was spontaneous, with increases made whenever the participant was able to perform the three sets of twelve complete repetitions15. To participate in the study, the individuals showed a medical clearance certificate for the practice of physical exercises. Additionally, the attendance rate was of at least 75% of the program for all participants, and therefore, none was lost to follow-up. All attended the two assessment visits proposed. Blood pressure Blood pressure was monitored by a Finometer™ (Finapres Medical System, BV, The Netherlands) device before and after the training program. Continuous digital electrocardiographic monitoring and noninvasive cardiovascular hemodynamic monitoring by digital infrared photoplethysmography were performed for 15 minutes with the individual in the sitting position. For the acquisition of pressure curves, a small sensor was placed around the middle phalanx of the left index finger, taking into consideration the participant’s age, body mass, height and gender. Body mass (BM) was expressed in kilograms and measured in a digital scale to the nearest 100 grams; height, in meters, was measured in a stadiometer to the nearest 0.1 centimeter; a 2-m flexible tape measure was used for the measurement of the abdominal circumference (AC). The following hemodynamic variables were considered for the analyses: systolic blood pressure (SBP), diastolic blood pressure (DBP), heart rate (HR), cardiac output (CO), peripheral vascular resistance (PVR) and stroke volume (SV); the latter was obtained using the formula SV = CO/HR. A researcher blind to the groups performed the assessments and analysis of variables. Statistical analyses Data are presented as means and standard deviation of the mean. The Shapiro-Wilk test was used to check the normality of data. The two-way ANOVA for repeated measures was used for the comparison of hemodynamic variables pre- and Arq Bras Cardiol. 2015; 104(6):487-492 488 Seron et al. Blood Pressure and Young Individuals with Down Syndrome Original Article post-aerobic or resistance training. The Pearson’s correlation coefficient was used to correlate the hemodynamic variables with age, body mass and height. Data were analyzed by the SPSS version 18.0 software; in all analyses, the significance level was set at 5%. Results Anthropometric data of the groups obtained before the intervention are shown in Table 1. No BP variables or hemodynamic variables showed statistically significant differences (p > 0.05) between the groups at the pre‑training timepoint. Data presented in Table 2 show a significant reduction (p < 0.05) of systolic, diastolic and mean blood pressure after aerobic and resistance training. No interaction was observed between the factor time and group for variables SBP (p = 0.20), DBP (p = 0.53) and MBP (p = 0.58). Data regarding heart rate, stroke volume, cardiac output and peripheral vascular resistance are shown in Table 3. No statistically significant differences were found for these variables between timepoints pre- and post-exercise in both groups. Finally, the Pearson’s correlation test between anthropometric, hemodynamic and blood pressure variables did not show significant values for any of the two groups studied. Discussion The major finding of the present study suggests a chronic hypotensive effect of aerobic and resistance exercise on young individuals with DS. Nonetheless, the findings of the present study corroborate those of several trials investigating the effects of exercise on blood pressure of non-disabled individuals, which usually show BP reduction after physical – especially aerobic, training. For resistance exercises, the few studies conducted also point to a BP reduction effect15-18 albeit less consistently in comparison to aerobic exercises. Despite the paucity of studies investigating the effect of exercises on blood pressure of individuals with DS, the literature shows some that address aspects of blood pressure and the vascular system in this population. According to Rodrigues et al19, although individuals with DS show early aging in several organ systems, no difference was observed regarding aortic artery stiffness, which is related to several risk factors for CVD, including high BP, in individuals with DS in comparison to individuals without this condition. Some studies have found that individuals with DS have chronic hypotension, i.e., blood pressure levels lower than those of normotensive individuals without the syndrome19-21. However, there is evidence that deaths related to cardiovascular diseases are more common in individuals with DS than in the general population2,22. Although BP levels of individuals with and without DS have not been compared in this study, the mean SBP and DBP found for the participants were considered within normal limits23. Additionally, the baseline levels of SBP, DBP and MBP were similar for both groups. The guidelines suggest that increasing physical activities contributes to the primary and secondary prevention of arterial hypertension15. However, according to Cornelissen and Smart18, the effect of training on the magnitude of BP reduction may vary according to the modality of exercise (aerobic or resistance), duration, intensity, and frequency of training . Our findings corroborate these authors’ recommendation of physical exercises for BP control18 based on the finding that aerobic exercises are effective in BP reduction, as are resistance exercises, which, albeit providing lower reductions in comparison to aerobic exercises, still play Table 1 – Anthropometric data of participants Aerobic training (n = 14) Resistance training (n = 15) 61.43 ± 11.6 52.7 ± 10.0 Height (cm) 151.7 ± 8.11 150.4 ± 7.0 BMI (kg/m²) 26.61 ± 4.36 23.3 ± 4.3 Abdominal circumference (cm) 86.8 ± 11.1 77.5 ± 9.2¥ Body mass (kg) ¥ Significant difference between groups – p < 0.05. Table 2 – Blood pressure values before and after training Variables SBP (mmHg) GrType of Training A Aerobic Training Group Resistance Pre Post Δ Pre Pós Δ Time p Time x group p Group p 119.6 ± 11.46 110.4 ± 11.7* -9.3 ± 8.8 113.19 ± 13.04 107.04 ± 10.41* -6.2 ± 12.0 0.001 0.05 0.03 DBP (mmHg) 77.27 ± 4.73 72.66 ± 6.69* -4.6 ± 6.9 76.98 ± 8.10 72.23 ± 8.30* -4.8 ± 10.2 0.03 0.53 0.98 MBP (mmHg) 92.58 ± 5.40 88.35 ± 7.37* -4.2 ± 7.3 91.74 ± 8.74 86.75 ± 8.38* -5.0 ± 9.7 0.01 0.58 0.74 SBP: systolic blood pressure; DBP: diastolic blood pressure; MBP: mean blood pressure. * significant difference between pre-training and post-training timepoints – p < 0.05. 489 Arq Bras Cardiol. 2015; 104(6):487-492 Seron et al. Blood Pressure and Young Individuals with Down Syndrome Original Article Table 3 – Values of hemodynamic variables before and after training Variables Training Group Aerobic Pre Post Training Group Resistance Pre Post Time p Time x group p Group p CO 2.97 ± 0.71 3.80 ± 0.81 2.76 ± 1.02 3.32 ± 1.05 0.60 0.98 0.20 PVR (mmHg.min.l) 32.91 ± 8.54 24.07 ± 4.48 36.62 ± 10.92 28.56 ± 9.64 0.22 0.93 0.07 HR (bpm/min) SV (ml) 81 ± 11 82 ± 11 84 ± 10.04 84 ± 9.34 0.93 0.58 0.31 0.037 ± 0.00 0.047 ± 0.01 0.032 ± 0.01 0.040 ± 0.01 0.43 0.77 0.17 CO: cardiac output; PVR: peripheral vascular resistance; HR: heart rate; SV: stroke volume. an important role in BP control. Thus, for this population, resistance training showed significant reductions in blood pressure levels (SBP = -6.2 mmHg; DBP = -4.8 mmHg; MBP = -4.2 mmHg). However, in addition to bringing benefits to blood pressure responses, resistance training has been considered safe for individuals with DS because it improves strength, balance and body composition24. As regards the chronic antihypertensive mechanisms of exercise, Pescatello et al25 found a reduction in peripheral vascular resistance as the major mechanism, which is possibly mediated by neuro-humoral and structural adaptations. Reduction in vasoconstrictors such as endothelin-1, and elevation in vasodilators such as nitric oxide have been pointed as neurohumoral adaptations to physical exercises26,27. Although several mechanisms and hemodynamic adaptations have been pointed in response to the chronic effects of aerobic and resistance training on BP, Cornelissen and Fagard28 conducted a meta-analysis and showed that the hemodynamic mechanisms in response to aerobic training resulted from a significant reduction of peripheral vascular resistance (PVR), with no changes in the cardiac output (CO). This can be explained by the increased SV, which is counterbalanced by decreased HR. In the present study, no significant changes were observed for peripheral vascular resistance in any of the groups (aerobic and resistance training) after the 12-week training. The adaptations in BP found in the present study may be important for individuals with DS, because, as Hu et al29 suggest, these individuals may have a higher incidence of cardiovascular risk factors such as a low cardiorespiratory capacity and obesity. In this context, many studies have advanced in relation to the influence of exercise on the physical fitness of young individuals with DS, and usually show positive results regarding their cardiopulmonary capacity, strength and body composition24,30-34. Therefore, the findings of the present study in relation to the chronic reduction of blood pressure after an intervention program contribute with more information on the potential benefits of physical exercises for this population. Although the physical training program has provided significant adaptations of blood pressure, some limitations should be pointed out. First, the number of individuals in each group was small, and this may have hindered some analyses. Additionally, the non-randomized division of intervention groups may have interfered in the results. Nonetheless, our findings may contribute to a better understanding of the physiological adaptations to physical exercises in young individuals with DS, in addition to stressing the importance of this practice for the health of this population. Conclusion By means of the interventions performed, the present study demonstrated that 12 weeks of either aerobic or resistance training provided significant reductions in SBP, DBP and MBP of young individuals with DS. The adaptations found are believed to significantly help control BP and prevent the risk of developing cardiovascular diseases. Therefore, the implementation of either aerobic or resistance training programs and practice of physical exercises is suggested for young individuals with DS as a means of preventing cardiovascular risks. For these individuals, maintaining a physically active lifestyle should be seen as a strategy that can contribute significantly to improve a sedentary lifestyle and obtain several health benefits. Author contributions Conception and design of the research:Seron BB, Goessler KF, Modesto EL, Greguol M. Acquisition of data: Seron BB, Goessler KF, Modesto EL, Almeida EW, Greguol M. Analysis and interpretation of the data: Seron BB, Goessler KF, Modesto EL, Almeida EW, Greguol M. Statistical analysis: Goessler KF. Writing of the manuscript: Seron BB. Critical revision of the manuscript for intellectual content: Seron BB, Goessler KF, Greguol M. Potential Conflict of Interest No potential conflict of interest relevant to this article was reported. Sources of Funding There were no external funding sources for this study. Study Association This article is part of the thesis of master submitted by Bruna Barboza Seron, from Universidade Estadual de Londrina. Arq Bras Cardiol. 2015; 104(6):487-492 490 Seron et al. Blood Pressure and Young Individuals with Down Syndrome Original Article References 1. Jonatan RR, Ortega FB. Physical activity and cardiovascular disease risk factors in children and adolescents. Curr Cardiovasc Risk Rep. 2009;3:281-7. 2. Hill DA, Gridley G, Cnattingius S, Mellemkjaer L, Linet M, Adami HO, et al. Mortality and cancer incidence among individuals with Down syndrome. Arch Intern Med. 2003;163(6):705-11. 3. Al-Bitagi MA. Echocardiography in children with Down syndrome. World J Clin Pediatr. 2013;2(4):36-45. 4. Weijerman ME, Van Furth AM, Van der Mooren MD, Van Weissenbruch MM, Rammeloo L, Broers CJ, et al. Prevalence of congenital heart defects and persistent pulmonary hypertension of the neonate with Down syndrome. Eur J Pediatr. 2010;169(10):1195-9. 5. Pate RR, Baranowski T, Dow M, Trost SG. Tracking of physical activity in young children. Med Sci Sports Exerc. 1996;28(1):92-6. 6. Mokdad AH, Serdula MK, Dietz WH, Bowman BA, Marks JS, Koplan JP. The continuing epidemic of obesity in the United States. JAMA. 2000;284(13):1650-1. 7. Telama R, Yang X, Viikari J, Välimäki I, Wanne O, Raitakari O. Physical activity from child hood to adult hood: a 21-year tracking study. Am J Prev Med. 2005;28(3):267-73. 8. Chen X, Wang Y. Tracking of blood pressure from childhood to adulthood: a systematic review and meta-regression analysis. Circulation. 2008;117(25):3171-80. 9. Blumenthal JA, Siegel WC, Appelbaum M. Failure of exercise to reduce blood pressure in patients with mild hypertension: results of a randomized controlled trial. JAMA. 1991;266(15):2098-104. 20. Richards BW, Enver F. Blood pressure in Down’s syndrome. J Ment Defic Res. 1979;23(2):123-35. 21.Morrison RA, McGrath A, Davidson G, Brown JJ, Murray GD, Lever AF. Low blood pressure in Down’s syndrome: a link with Alzheimer’s disease? Hypertension. 1996;28(4):569-75. 22. Day SM, Strauss DJ, Shavelle RM, Reynolds RJ. Mortality and causes of death in persons with Down syndrome in California. Dev Med Child Neurol. 2005;47(3):171-6. 23. World Health Organization (WHO). A Global brief on hypertension: silent killer, Global public health crisis [Online]. [Acessed on 2014 June 10]. Available from: http://apps.who.int/isis/bitstream/10665/79059/who/_dco. 24. Modesto EL, Greguol M. Influência do treinamento resistido em pessoas com síndrome de Down – uma revisão sistemática. Rev Bras Ativ Fis e Saúde Pelotas/RS. 2014;9(2):153-67. 25. Pescatello LS, Franklin BA, Fagard R, Farquhar WB, Kelley GA, Ray CA; American College of Sports Medicine. American College of Sports Medicine position stand: exercise and hypertension. Med Sci Sports Exerc. 2004;36(3):533-53. 26. Kingwell BA, Sherrard B, Jennings GL, Dart AM. Four weeks of cycle training increases basal production of nitric oxide from the fore arm. Am J Physiol. 1997;272(3 Pt 2):H1070-7. 10. Kelley GA, Kelley KS, Tran ZV. The effects of exercise on resting blood pressure in children and adolescents: a meta-analysis of randomized controlled trials. Prev Cardiol. 2003;6(1):8-16. 27. Maeda S, Miyauchi T, Kakiyama T, Sugawara J, Iemitsu M, Irukayama-Tomobe Y, et al. Effects of exercise training of 8 weeks and detraining on plasma levels of endothelium-derived factors, endothelin-1 and nitric oxide, in healthy young humans. Life Sci. 2001;69(9):1005-16. 11. McDonnell BJ, Maki-Petaja MK, Munnery M, Yasmin, Wilkinson IB, Cockcroft JR, et al. Habitual exercise and blood pressure: age dependency and underlying mechanisms. Am J Hypertens. 2013;26(3):334-41. 28.Cornelissen VA, Fagard RH. Effects of endurance training on blood pressure, blood pressure–regulating mechanisms, and cardiovascular risk factors. Hypertension. 2005;46(4):667-75. 12. Balic MG, Mateos EC, Blasco CG, Fernhall B. Physical fitness levels of physically active and sedentary adults with Down syndrome. Adapt Phys Activity Quarterly. 2000;17:310-21. 29. Hu M, Yan H, Ranadive SM, Agiovlasitis S, Fahs CA, Atiq M, et al. Arterial stiffness response to exercise in persons with and without Down syndrome. Res Dev Disabil. 2013;34(10):3139-47. 13. Dodd KJ, Shields N. A systematic review of the outcomes of cardiovascular exercise programs for people with Down syndrome. Arch Phys Med Rehabil. 2005;86(10):2051-8. 30. Shields N, Taylor NF, Wee E, Wollersheim D, O’Shea SD, Fernhall B. A community-based strength training programme increases muscle strength and physical activity in young people with Down syndrome: a randomised controlled trial. Res Dev Disabil. 2013;34(12):4385-94. 14. Fernhall B, Millar AL, Tymeson GT, Burkett LN. Maximal exercise testing of mentally retarded adolescents and adults: reliability study. Arch Phys Med Rehabil. 1990;71(13):1065-8. 15. American College of Sports Medicine. ACSM’s Guidelines for exercise testing and prescription. 8th ed. Baltimore; 2009. 16. Fagard RH. Exercise is good for your blood pressure: effects of endurance training and resistance training. Clin Exp Pharmacol Physiol. 2006;33(9):853-6. 17. Cardoso CG, Gomides RS, Queiroz AC, Pinto LG, Lobo FS, Tinucci T, et al. Acute and chronic effects of aerobic and resistance exercise on ambulatory blood pressure. Clinics (Sao Paulo). 2010;65(3):317-25. 18. Cornelissen VA, Smart NA. Exercise training for blood pressure: a systematic review and meta analysis. J Am Heart Assoc. 2013;2(1):e004473. 491 19. Rodrigues AN, Coelho LC, Gonçalves WL, Gouvêa SA, Vasconcellos MJ, Cunha RS, et al. Stiffness of the large arteries in individuals with and without Down syndrome. Vasc Health Risk Manag. 2011;7:375-81. Arq Bras Cardiol. 2015; 104(6):487-492 31. Casajus J, Pueyo D, Vicente-Rodríguez G, González-Agüero A. Mejoras de la condición cardiorrespiratoria en jóvenes con síndrome de Down mediante entrenamiento aeróbico: estudio longitudinal. Apunts Med Esport. 2012;47(174):49-54. 32. Lin HC, Wuang YP. Strength and agility training in adolescents with Down syndrome: a randomized controlled trial. Res Dev Disabil. 2012;33(6):2236-44. 33. Gupta S, Rao BK, Kumaran SD. Effect of strength and balance training in children with Down’s syndrome: a randomized controlled trial. Clin Rehabil. 2011;25(5):425-32. 34. Ordonez FJ, Rosety M, Rosety-Rodriguez M. Influence of 12-week exercise training on fat mass percentage in adolescents with Down syndrome. Med Sci Monit. 2006;12(10):CR416-9. Seron et al. Blood Pressure and Young Individuals with Down Syndrome Original Article Arq Bras Cardiol. 2015; 104(6):487-492 492 Back to the Cover Original Article Heart Rate Variability Correlates to Functional Aerobic Impairment in Hemodialysis Patients Maria Angela Magalhães de Queiroz Carreira1, André Barros Nogueira1, Felipe Montes Pena1, Marcio Galindo Kiuchi1, Ronaldo Campos Rodrigues1, Rodrigo da Rocha Rodrigues1, Jorge Paulo Strogoff de Matos2, Jocemir Ronaldo Lugon2 Universidade Federal Fluminense, Department of Cardiology1; Universidade Federal Fluminense, Department of Nephrology2, Rio de Janeiro, RJ - Brazil Abstract Background: Autonomic dysfunction (AD) is highly prevalent in hemodialysis (HD) patients and has been implicated in their increased risk of cardiovascular mortality. Objective: To correlate heart rate variability (HRV) during exercise treadmill test (ETT) with the values obtained when measuring functional aerobic impairment (FAI) in HD patients and controls. Methods: Cross-sectional study involving HD patients and a control group. Clinical examination, blood sampling, transthoracic echocardiogram, 24-hour Holter, and ETT were performed. A symptom-limited ramp treadmill protocol with active recovery was employed. Heart rate variability was evaluated in time domain at exercise and recovery periods. Results: Forty-one HD patients and 41 controls concluded the study. HD patients had higher FAI and lower HRV than controls (p < 0.001 for both). A correlation was found between exercise HRV (SDNN) and FAI in both groups. This association was independent of age, sex, smoking, body mass index, diabetes, and clonidine or beta-blocker use, but not of hemoglobin levels. Conclusion: No association was found between FAI and HRV on 24-hour Holter or at the recovery period of ETT. Of note, exercise HRV was inversely correlated with FAI in HD patients and controls. (Arq Bras Cardiol. 2015; 104(6):493-501) Keywords: Sympathetic Nervous System / physiopathology; Exercise Test; Renal Dialysis; Mortality; Exercise. Introduction The treatment offered to end-stage renal disease (ESRD) patients on hemodialysis (HD) has improved over the past decades resulting in increased survival and better quality of life1. However, cardiovascular morbidity and mortality remain exceptionally high in this group of patients2. The prevalence of autonomic dysfunction (AD) is high in patients undergoing current standard HD treatment1 and this has been associated with an increased risk of sudden death2. In the general population, cardiorespiratory fitness (CRF) is an independent predictor of all-cause and cardiovascular mortality3. In normal subjects, maximal functional aerobic capacity was inversely associated with the risk of all-cause and cardiovascular death. The risk was 2.50 times higher for all-cause death, and 2.04 times higher for cardiovascular death in men with a low exercise capacity than in men with Mailing Address: Maria Angela Magalhães de Queiroz Carreira • Rua Arroio Fundo, 230, Anil. Postal Code 22765-260, Rio de Janeiro, RJ – Brazil E-mail: [email protected] Manuscript received September 12, 2014; revised manuscript January 14, 2015; accepted January 19, 2015. DOI: 10.5935/abc.20150039 493 a high exercise capacity, after adjustment for risk factors and ischemic ST changes during exercise4. Cardiorespiratory fitness is also a predictor of sudden cardiac death in normal subjects. As a continuous variable, one metabolic equivalent (MET) increment in CRF was associated with a 22% decrease in the risk of sudden cardiac death in normal men4. Exercise treadmill test (ETT) has been used in the assessment of autonomic function by analyzing changes in heart rate (HR) under physical stress. The aim of this study was to assess the autonomic function of HD patients and controls by assessing HR variability (HRV) during an ETT and to correlate the results with functional aerobic impairment (FAI). Methods Study population We conducted a cross-sectional study with ESRD patients on HD three times a week (4-hour duration sessions) for at least three months and a control group matched by sex and age without overt kidney disease. Hemodialysis patients were recruited from a single dialysis center and the control group consisted of individuals referred for exercise testing at the University Hospital. Informed consent was obtained, and the study protocol was approved by the Medical School ethical Carreira et al. RR variability and functional aerobic impairment Original Article committee. Chronic medications, including those for blood pressure control, were not discontinued during the study. Exclusion criteria were as follows: impaired gait that prevented walking on the treadmill, arrhythmias preventing proper HR assessment, and presence of symptomatic heart disease. Cardiac evaluation was always accomplished in a middle-of-week non-dialytic day and consisted of clinical examination, transthoracic echocardiogram, 24-h Holter, and ETT. Echocardiography A two-dimensional transthoracic echocardiography was performed with GE VIVID 7 System (General Electric, USA) to assess left ventricle wall motion and systolic and diastolic ventricular function. 24-h Holter Patients underwent a 24-h Holter (Galix Biomedical Instrumentation, Florida, USA). A 3-channel recorder was used to record the electrocardiographic tracings. A time domain analysis of HRV was performed, and the following parameters were obtained: a) SDNN, standard deviation (SD) of all normal RR intervals (NN); b) SDANN, SD of the averages of 5-min NN intervals over 24h; c) rMSSD, the square root of the mean of the square of successive NN intervals; and d) triangular index (TI), integral of the density distribution (that is, the number of all NN intervals) divided by the maximal density distribution. Exercise treadmill test Patients underwent ETT with a treadmill ramp protocol using the Ergo13 program (Heart Ware Co., Minas Gerais, Brazil). The test was symptom limited, with 2-minute active recovery under 40% of the speed and incline of peak effort. Automatic ECG recordings were obtained on 13 simultaneous leads before exercise in the supine and standing positions, at peak exercise, and at every recovery minute. The following HRV parameters were analyzed: SDNN and rMSSD during exercise and recovery. For the ramp protocol, the predicted maximal VO2 was reduced by 20% in HD patients. The maximal VO2 peak exercise was obtained by the Foster formula backed with hands. The FAI was calculated using the formula: FAI= [(maximal predicted VO2–VO2 peak) /maximal predicted VO2] x 100. In ETT, HRV was obtained with a software specially designed for the study, conveying electrocardiographic data findings from Ergo13 to Cardio Smart (Cardios, São Paulo, Brazil) during exercise and recovery separately. Statistics Results were expressed as mean and SD, for normal distribution, and median and range, otherwise. Categorical variables were expressed as frequencies and compared using the Chi-square test. Comparisons between two continuous variables were accomplished by the t test (for normal distribution) or its nonparametric equivalent (Mann‑Whitney test). Correlation was assessed using the Pearson test. Logistic regression was used to analyze associations. Variables with p values < 0.10 were included in the multivariate model, and p < 0.05 was considered significant. Analyses were performed using SPSS for Windows version 18.0 (SPSS Inc., Chicago, IL, USA). Results A total of 125 patients from a single dialysis center were initially evaluated. Nine were promptly excluded due to gait impairment. Of the 116 remaining, 59 agreed to participate and signed the consent form. Eighteen patients were excluded: 10 did not show up for the exams, 4 had a past myocardial infarction, 2 had arrhythmia, 1 had artery-venous fistulas in both arms, and 1 had current pulmonary infection. At the end, 41 HD patients concluded the study. The most common renal disease etiologies were: hypertensive nephrosclerosis (56%), chronic glomerulonephritis (17%), adult polycystic kidney disease (10%), and diabetic nephropathy (7%). Table 1 shows the general features of patients and controls. Use of antihypertensive drugs and physical inactivity were more frequent among patients on HD. Use of beta‑blockers tended to be higher in HD patients, but statistical significance was not found. Diuretic use was more common in the control group. Left ventricular systolic function, analyzed by the ejection fraction on echocardiogram, was similar between groups (66.1 ± 10.1% vs. 68.6 ± 5.4% for HD patients and controls, respectively, p = 0.167), but diastolic dysfunction was more prevalent in HD patients (77% vs. 42%, p = 0.004). Table 2 shows the cardiovascular parameters on ETT. There was no difference between groups in relation to pre‑exercise test parameters. Functional aerobic impairment was found higher in HD patients (Figure 1). Reasons for stopping the exercise were as follows: general exhaustion, 80.5%; exhaustion of the muscles of lower limbs, 4.9%; left bundle branch block of high‑grade, 2.4%; arrhythmia, 2.4%; and hypertension, 2.4%. No complications occurred during ETT in any group. When analyzing the 24-h Holter, HD patients showed less HRV than controls. Differences were observed regarding the mean HRV values during exercise and recovery (Table 3). SDNN was significantly lower in HD patients than in controls on 24-h Holter, and during exercise and recovery (Figure 2). Exercise SDNN correlated with FAI in HD patients and controls (Figure 3). On 24-h Holter, there was no correlation between HRV and FAI (Table 4). An exercise SDNN < 40 ms (median) was used as the dependent variable to test associations with FAI. In every multivariate logistic regression model tested, exercise SDNN < 40 ms was independently associated with FAI, regardless of age, sex, body mass index, smoking, diabetes, and beta‑blocker or clonidine use. However, the association was found to be dependent on serum levels of hemoglobin (Table 5). Arq Bras Cardiol. 2015; 104(6):493-501 494 Carreira et al. RR variability and functional aerobic impairment Original Article Table 1 – General features of HD patients and controls HD patients Age, years 50 ± 14 Male, % 21 (51.2)b a Controls p value 50 ± 13 0.975 21 (51.2) 1.000 Race, non-white % 27 (65.9) 21 (51.2) 0.391 Body mass index, kg/m2 25.1 ± 5.1 27.3 ± 4.1 0.030 HD vintage, months 67.2 ± 47.3 n.a. 4 (9.8) 5 (12.2) 0.724 Diabetes, % Smoking, % 3 (9.1) 8 (20.5) 0.180 Familial CAD,% 15 (36.6) 17 (41.5) 0.520 Familial hypertension, % 26 (63.4) 21 (51.2) 0.525 Sedentary lifestyle, % 33 (80.5) 24 (58.5) 0.031 Anti-hypertensive drugs, % Beta-blocker 33 (80.5) 20 (48.8) 0.003 14 (34.1) 7 (17.1) 0.077 Diuretic 2 (4.9) 8 (19.5) 0.043 Calcium channel blocker 5 (12.2) 2 (4.9) 0.236 ACE inhibitor/ARB 12 (29.3) 16 (39.0) 0.352 Clonidine 8 (19.5) - 0.003 Alfa-blocker Hemoglobin, g/dL eGFR (MDRD study), ml/min/1.73m2 6 (14.6) - 0.011 11.5 ± 1.4 13.8 ± 1.2 < 0.001 n.a. 87.5 ± 23.1 HD: hemodialysis; CAD: coronary artery disease; ACE: angiotensin-converting-enzyme; ARB: AT1-receptor blocker; n.a.: not applicable; eGFR: estimated glomerular filtration rate; MDRD: modification of diet in renal disease. a Mean ± SD; b n (%). Table 2 – Baseline and peak values of heart rate, blood pressure and functional capacity on ETT in HD patients and controls HD patients Controls p value pre-exercise HR, bpm 77 ± 12a 76 ± 13 0.705 pre-exercise SBP, mmHg 131 ± 39 130 ± 31 0.860 pre-exercise DBP, mmHg 82 ± 11 83 ± 9 0.135 peak HR, bpm 130 ± 25 160 ± 19 < 0.001 peak SBP, mmHg 193 ± 26 199 ± 21 0.273 peak DBP, mmHg 99 ± 11 93 ± 11 0.040 Exercise time, min 8.5 ± 1.9 10.1 ± 2.4 0.002 29.5 ± 12.0 2.8 ± 20.1 < 0.001 FAI, % HD: hemodialysis; HR: heart rate; SBP: systolic blood pressure; DBP: diastolic blood pressure. FAI: functional aerobic impairment. a Mean ± SD Discussion In ESRD patients, AD is a frequent abnormality and a marker of cardiovascular events and death5-8. Exercise treadmill test, a valuable tool to assess AD, is hardly used in HD patients. We studied autonomic parameters related to HRV during ETT in HD patients as compared to a control group, and the ETT results were correlated with FAI. 495 Arq Bras Cardiol. 2015; 104(6):493-501 In our sample, the body mass index was in the upper limit of normality (borderline overweight) in HD patients, and clearly above that limit in the control group. This is not unexpected considering that malnutrition was common in HD patients in the past9, but not in the present, and that obesity is a recognized risk factor for cardiovascular disease 10,11. The proportion of diabetes mellitus in our sample was lower than that reported in international series12,13, and even lower than that reported Carreira et al. RR variability and functional aerobic impairment Original Article Figure 1 – Functional aerobic impairment in hemodialysis (HD) patients and controls. Table 3 – Heart rate variability parameters during 24-h Holter and exercise treadmill test in HD patients and controls HD patients Controls p value SDNN, msec 82.6 ± 27.6 119.1 ± 47.6 < 0.001 SDANN, msec 74.3 ± 26.8 113.1 ± 43.2 < 0.001 rMSSD, msec 17.4 ± 7.7 27.6 ± 11.1 < 0.001 Triangular index, msec 23.3 ± 8.4 34.4 ± 9.3 < 0.001 exercise SDNN, msec 33.7 ± 14.2 50.0 ± 21.8 < 0.001 exercise rMSSD, msec 11.0 ± 5.5 15.3 ± 14.7 0.092 recovery SDNN, msec 20.1 ± 9.8 27.3 ± 17.4 0.024 recovery rMSSD, msec 11.5 ± 7.8 15.4 ± 17.3 0.196 24-h Holter Exercise treadmill test HD: hemodialysis; SDNN: standard deviation (SD) of all normal RR intervals (NN); SDANN: SD of the averages of 5-min NN intervals over 24h; rMSSD: the square root of the mean of the square of successive NN intervals. Values shown as mean ± SD. for the Brazilian dialysis population14, probably as a result of the inclusion and exclusion criteria adopted in the study. In support to the majority of reported series1,12-14, a substantial number of HD patients used anti-hypertensive drugs. Consistent with the concept that sympathetic hyperactivity may play an important role in the hypertension of CKD patients, drugs mainly affecting this pathway were more frequently prescribed for HD patients 15. In agreement with previous reports 16,17, left diastolic dysfunction on echocardiogram was more frequent in HD patients. In contrast, left ventricular systolic function was similar in both groups, perhaps due to our enrollment criteria, which excluded patients with overt heart failure. When analyzing cardiovascular parameters in ETT, no difference was found between groups regarding systolic (SBP) or diastolic blood pressure (DBP) either at rest or exercise peak. Similarly, the HR at rest did not differ between groups, but the HR at peak exercise was lower in Arq Bras Cardiol. 2015; 104(6):493-501 496 Carreira et al. RR variability and functional aerobic impairment Original Article Figure 2 – Heart rate variability (SDNN) during 24-h Holter, exercise, and recovery in hemodialysis (HD) patients and controls. Figure 3 – Correlation between functional aerobic impairment and heart rate variability (SDNN) during exercise in hemodialysis patients (left) and controls (right). HD patients. An attenuated HR response to exercise has been shown to predict adverse cardiac events in subjects without overt cardiovascular disease. Reduced HR response to exercise also predicts major adverse cardiac events among individuals with overt or suspected cardiovascular disease even after adjusting for left ventricular function and the severity of exercise-induced myocardial ischemia18. Our population comprised individuals of different ages. For this reason, to analyze functional aerobic capacity we resort to the use of FAI, which compares the obtained VO2 497 Arq Bras Cardiol. 2015; 104(6):493-501 with that expected for age and sex. In our results, FAI was higher in HD patients, a well-documented finding in HD patients 3,19. In the general population, the functional aerobic capacity is a factor independently associated with cardiovascular and overall mortality. Our results found a mean FAI of 30% in the HD group and of 3% in the control group. In this population, the FAI may reach 65% of that predicted for sex and age as compared to controls20. Many factors may be involved with this reduction, some relating to the pathophysiology of the disease and others Carreira et al. RR variability and functional aerobic impairment Original Article Table 4 – Correlation coefficients between functional aerobic impairment and heart rate variability during 24-h Holter and exercise treadmill test in hemodialysis (HD) patients and controls HD patients Controls r p r p -0.046 0.780 -0.183 0.260 24-h Holter SDNN SDANN -0.044 0.792 -0.274 0.087 rMSSD -0.090 0.585 0.248 0.123 Triangular index -0.072 0.661 -0.123 0.451 -0.633 < 0.001 -0.752 < 0.001 Exercise treadmill test exercise SDNN exercise rMSSD 0.300 0.858 0.023 0.887 recovery SDNN -0.017 0.917 0.038 0.813 recovery SDNN 0.080 0.622 -0.028 0.864 r: Correlation coefficient; SDNN: standard deviation (SD) of all normal RR intervals (NN); SDANN: SD of the averages of 5-min NN intervals over 24h; rMSSD: the square root of the mean of the square of successive NN intervals. Table 5 – Crude and adjusted OR and 95% CI in different models of multivariate logistic regression to test for associations of exercise SDNN <40 msec with functional aerobic impairment in hemodialysis patients OR 95% CI p value Crude 1.145 1.033-1.270 0.010 Model 1 1.213 1.059-1.390 0.005 Model 2 1.160 1.022-1.318 0.022 Model 3 1.141 1.010-1.288 0.034 Model 4 1.149 1.007-1.312 0.039 Model 5 1.153 0.979-1.357 0.088 The models consisted of the progressive inclusion of the following confounding factors: age and sex (model 1); smoking and body mass index (model 2); diabetes (model 3); clonidine and beta-blocker use (model 4); and hemoglobin (model 5). to age and environment. 3 During exercise, there is an increased oxygen demand to supply muscle activity. The provision of this increase depends on many factors: peripherally, increased blood flow and increment of the arteriovenous oxygen extraction; and centrally, increased cardiac output. The raise in cardiac output during exercise depends mainly on HR increase. However, in HD patients, the chronotropic reserve is often reduced and this has been attributed to AD, admittedly present in uremia.3 Autonomic tests are frequently abnormal in HD patients. Heart rate variability during a 24-h Holter has been considered a good marker of dysautonomia in those patients7,8. Reduced HRV in the time or frequency domain has been associated with reduced survival in individuals on HD6,7,21. In consonance with previous studies, the HRV during 24-h Holter was lower in our HD patients demonstrating an altered autonomic function5-7,21,22. During ETT, HRV in the time domain decreases in the supine position and during exercise, and increases very slowly in the recovery period after exercise. Sympathetic hyperactivity persists for at least 45 minutes after exercise, being accompanied by a reduction in HRV20. In our results, SDNN during ETT was significantly lower in HD patients during exercise and recovery. These findings again may reflect the hyperadrenergic state characteristic of HD patients, because SDNN represents a general evaluation of the autonomic nervous system balance, which depends on modulation by sympathetic and parasympathetic branches6. In contrast, the variable predominantly affected by the parasympathetic branch, rMSSD, was not different between groups. Our results showed a significant correlation between FAI and SDNN during exercise in both HD patients and controls. This finding reinforces the hypothesis that the reduction in functional aerobic capacity is strongly associated with the presence and severity of dysautonomia.23 The stress resulting from exercise requires substantial changes of the autonomic nervous system, facilitating recognition of disturbances that otherwise could remain undetectable. Arq Bras Cardiol. 2015; 104(6):493-501 498 Carreira et al. RR variability and functional aerobic impairment Original Article Our HD patients had reduced serum levels of hemoglobin, a finding not uncommon in ESRD. To control for anemia and other confounding factors regarding the association of HRV during exercise with FAI, we resort to a variety of logistic regression models in which smoking and diabetes (associated with lower HRV), and anemia and use of beta-blocker or clonidine (associated with increased FAI) were included as explanatory variables. Exercise SDNN was independently associated with FAI in all models tested, except for the one in which serum levels of hemoglobin were included. Several authors23-27 have reported that the reduction of serum levels of hemoglobin causes a significant reduction in CRF and that the higher the reduction, the greater the FAI.23 Furthermore, red cell transfusion23,24 or administration of erythropoietin 25-27 was associated with a significant improvement in functional aerobic capacity, with a 6%-18% increase in VO2 peak in different series and protocols. The clinical relevance of our findings is prominent. Both AD and FAI are important predictors of mortality, justifying that efforts be made to find ways to reduce the risk of affected patients. From the pharmacological point of view, in addition to the treatment of anemia with erythropoietin, which effectively increases the functional capacity of those patients, alternatives are sparse.3,26,,27 In this regard, the use of inhibitors of hepcidin, a peptide involved in the pathogenesis of anemia of chronic/ inflammatory diseases28,29, looks promising. On the other hand, it is well established that training improves functional capacity and reduces the rate of overall and cardiovascular mortality of those patients30,31. The mechanisms by which this occurs are multiple and certainly involve improvement in autonomic function and inflammation31,32. The reduced number of patients recruited from a single dialysis center is a limitation of our study. It should also be pointed that the maximal VO2 during peak exercise was obtained by using the Foster formula, backed with hands, and not by using direct measurement of gas exchange during exercise. This should be especially considered, because we could not find validation studies of the cited formula for HD patients. In view of that, additional studies are needed to confirm our findings. Conclusion Functional aerobic impairment showed a strong correlation with HRV during exercise. This association was independent of age, sex, body mass index, smoking, diabetes, use of beta-blockers or clonidine, but not of serum levels of hemoglobin. Author contributions Conception and design of the research:Carreira MAMQ, Nogueira AB, Pena FM, Kiuchi MG, Rodrigues RC, Rodrigues RR, Matos JPS, Lugon JR. Acquisition of data:Carreira MAMQ, Nogueira AB, Pena FM, Kiuchi MG, Rodrigues RC, Rodrigues RR, Matos JPS, Lugon JR. Analysis and interpretation of the data: Carreira MAMQ, Nogueira AB, Pena FM, Kiuchi MG, Rodrigues RC, Rodrigues RR, Matos JPS, Lugon JR. Statistical analysis: Carreira MAMQ, Nogueira AB, Pena FM, Kiuchi MG, Rodrigues RC, Rodrigues RR, Matos JPS, Lugon JR. Obtaining financing: Carreira MAMQ, Matos JPS, Lugon JR. Writing of the manuscript:Carreira MAMQ, Pena FM, Rodrigues RC, Matos JPS, Lugon JR. Critical revision of the manuscript for intellectual content: Carreira MAMQ, Nogueira AB, Pena FM, Kiuchi MG, Rodrigues RC, Rodrigues RR, Matos JPS, Lugon JR. Potential Conflict of Interest No potential conflict of interest relevant to this article was reported. Sources of Funding This study was partially funded by FAPERJ. Study Association This article is part of the thesis of Doctoral submitted byMaria Angela M. Q. Carreira, from Universidade Federal Fluminense. References 1. Lugon JR, Warrak EA, Lugon AS, Salvador BA, Nobrega AC. Revisiting autonomic dysfunction in end-stage renal disease patients. Hemodial Int. 2003;7(3):198-203. 2. Herzog CA, Mangrum JM, and Passman R. Sudden cardiac death and dialysis patients. Semin Dial. 2008;21(4):300-7. 3. Painter P. Determinants of exercise capacity in CKD patients treated with hemodialysis. Adv Chronic Kidney Dis. 2009;16(6):437-48. 499 4. Laukkanen JA, Mäkikallio TH, Rauramaa R, Kiviniemi V, Ronkainen K, Kurl S. Cardiorespiratory fitness is related to the risk of sudden cardiac death. J Am Coll Cardiol. 2010:56(18):1476-83. 5. Chan CT, Levin NW, Chertow GM, Larive B, Schulman G, Kotanko P; Frequent Hemodialysis Network Daily Trial Group. Determinants of Cardiac Autonomic dysfunction in ESRD. Clin J Am Soc Nephrol. 2010;5(10):1821-7. Arq Bras Cardiol. 2015; 104(6):493-501 6. Fukuta H, Hayamo J, Ishihara S, Sakata S, Mukai S, Ohte N, et al. Prognostic value of heart rate variability in patients with end-stage renal disease on chronic haemodialysis. Nephrol Dial Transplant. 2003;18(2):318-25. 7. Oikawa K, Ishihara R, Maeda T, Yamaguchi K, Koike A, Kawaguchi H, et al. Prognostic value of heart rate variability in patients with renal failure on hemodialysis. Int J Cardiol. 2009;131(3):370-7. 8. Brotman DJ, Bash LD, Qayyum R, Crews D, Whitsel EA, Astor BC, et al. Heart rate variability predicts ESRD and CKD-related hospitalization. J Am Soc Nephrol. 2010;21(9):1560-70. 9. Stenvinkel P, Heimbürger O, Lindholm B, Kaysen GA, Bergström J. Are there two types of malnutrition in chronic renal failure? Evidence for relationships between malnutrition, inflammation and atherosclerosis (MIA syndrome). Nephrol Dial Transplant. 2000;15(7):953-60. Carreira et al. RR variability and functional aerobic impairment Original Article 10. Bonanni A, Mannucci I, Verzola D, Sofia A, Saffioti S, Gianetta E, et al. Protein-energy wasting and mortality in chronic kidney disease. Int J Environ Res Public Health. 2011;8(5):1631-54. 21. Ranpuria R, Hall M, Chan CT, Unruh M. Renal-heart rate variability (HRV) in kidney failure: measurement and consequences of reduced HRV. Nephrol Dial Transplant. 2008;23(2):444-9. 11. Ikizler TA, Cano NJ, Franch H, Fouque D, Himmelfarb J, Kalantar-Zadeh K et al; International Society of Renal Nutrition and Metabolism. Prevention and treatment of protein energy wasting in chronic kidney disease patients: a consensus statement by the International Society of Renal Nutrition and Metabolism. Kidney Int. 2013;84(6):1096-107. 22. Rubinger R, Revis N, Pollak A, Luria MH, Sapoznikov D. Predictors of haemodynamic instability and heart rate variability during haemodialysis. Nephrol Dial Transplant. 2004;19(8):2053-60. 12. United States Renal Data System. Cardiovascular disease. [Accessed in 2014 Feb 10]. Available from: http://www.ursds.org/2012/pdf/ v2_ch4_12.pdf 13. Foster MC, Rawlings AM, Marrett E, Neff D, Willis K, Inker LA, et al. Cardiovascular risk factor burden, treatment, and control among adults with chronic kidney disease in the United States. Am Heart J. 2013;166(1):150-6. 14. Sesso RC, Lopes AA, Thomé FS, Lugon JR, Watanabe Y, Santos DR. [Chronic dialysis in Brazil: report of the Brazilian dialysis census, 2011]. J Bras Nefrol. 2012; 34(3):272-7. 15. Joles JA, Koomans HA. Causes and consequences of increased sympathetic activity in renal disease. Hypertension. 2004;43(4):699-706. 16. Ie EH, Zietse R. Evaluation of cardiac function in the dialysis patient - a primer for the non-expert. Nephrol Dial Transplant. 2006;21(6):1474-81. 17. Jakubovic BD, Wald R, Goldstein MB, Leong-Poi H, Yuen DA, Perl J, et al. Comparative assessment of 2-dimensional echocardiography vs cardiac magnetic resonance imaging in measuring left ventricular mass in patients with and without end-stage renal disease. Can J Cardiol. 2013;29(3):384-90. 18. Elhendy A, Mahoney DW, Khandheria BK, Burger K, Pellikka PA. Prognostic significance of impairment of heart rate response to exercise impact of left ventricular function and myocardial ischemia. J Am Coll Cardiol. 2003;42(5):823-30. 19. Fotbolcu H, Duman D, Ecder SA, Oduncu V, Cevik C, Tigen K, et al. Attenuated cardiovascular response to sympathetic system activation during exercise in patients with dialysis-induced hypotension. Am J Nephrol. 2011;33(6):491-8. 20. Lahiri MK, Chicos A, Bergner D, Ng J, Banthia S, Wang NC, et al. Recovery of heart rate variability and ventricular repolarization indices following exercise. Ann Noninvasive Electrocardiol. 2012;17(4):349-60. 23. Rocha Messias L, de Queiroz Carreira MÂ, Ribeiro de Miranda SM, Cunha de Azevedo J, Ambrósio Gava I, Campos Rodrigues R, et al. Relação entre imagem adrenérgica cardíaca e teste ergométrico. Arq Bras Cardiol. 2011;96(5):370-5. 24. Ekblom B, Goldbarg AN, Gullbrin B. Response to exercise after blood loss and reinfusion. J Appl Physiol. 1972;33(2):175-80. 25. Ekblom B, Wilson G, Astrand PO. Central circulation during exercise after venesection and reinfusion of red blood cells. J Appl Physiol. 1976;40(3):379-83. 26. Thomsen JJ, Rentsch RL, Robach P, Calbet JA, Boushel R, Rasmussen P, et al. Prolonged administration of recombinant human erythropoietin increases submaximal performance more than maximal aerobic capacity. Eur J Appl Physiol. 2007;101(4):481-6. 27. Barany P, Freyschuss U, Pettersson E, Bergstrom J. Treatment of anaemia in haemodialysis patients with erythropoietin: long-term effects on exercise capacity. Clin Sci (Lond). 1993;84(4):441-7. 28. Robertson HT, Haley NR, Guthrie M, Cardenas D, Eschbach JW, Adamson JW. Recombinant erythropoietin improves exercise capacity in anemic hemodialysis patients. Am J Kidney Dis. 1990;15(4):325-32. 29. Poli M, Asperti M, Ruzzenenti P, Regoni M, Arosio P. Hepcidin antagonists for potential treatments of disorders with hepcidin excess. Front Pharmacol. 2014;5:86. 30. Stamatakis E, Weiler R. Prevention of cardiovascular disease: why do we neglect the most potent intervention? Heart. 2010;96(4):261-2. 31. Voller H, Gitt A, Jannowitz C, Karoff M, Karmann B, Pittrow D, et al. Treatment patterns, risk factor control and functional capacity in patients with cardiovascular and chronic kidney disease in the cardiac rehabilitation setting. Eur J Prev Cardiol. 2014;21(9):1125-33. 32. Jae SY, Heffernan KS, Yoon ES, Lee MK, Fernhall B, Park WH. The inverse association between cardiorespiratory fitness and C-reactive protein is mediated by autonomic function: a possible role of the cholinergic antiinflammatory pathway. Mol Med. 2009;15(9-10):291-6. Arq Bras Cardiol. 2015; 104(6):493-501 500 Carreira et al. RR variability and functional aerobic impairment Original Article 501 Arq Bras Cardiol. 2015; 104(6):493-501 Back to the Cover Review Article Reverse Cardiac Remodeling: A Marker of Better Prognosis in Heart Failure José Rosino de Araújo Rocha Reis Filho1, Juliano Novaes Cardoso1, Cristina Martins dos Reis Cardoso1, Antonio Carlos Pereira-Barretto1,2 Serviço de Cardiologia do Hospital Santa Marcelina1; Instituto do Coração, Hospital das Clínicas, Faculdade de Medicina, Universidade de São Paulo (USP)2, São Paulo, SP – Brazil Abstract In heart failure syndrome, myocardial dysfunction causes an increase in neurohormonal activity, which is an adaptive and compensatory mechanism in response to the reduction in cardiac output. Neurohormonal activity is initially stimulated in an attempt to maintain compensation; however, when it remains increased, it contributes to the intensification of clinical manifestations and myocardial damage. Cardiac remodeling comprises changes in ventricular volume as well as the thickness and shape of the myocardial wall. With optimized treatment, such remodeling can be reversed, causing gradual improvement in cardiac function and consequently improved prognosis. Introduction When cardiac function reduces, neurohormonal activity increases. This important compensatory mechanism is a response to reduced cardiac output and also the main component in syndrome progression and in cardiac remodeling process. Neurohormonal activity is initially stimulated in an attempt to maintain compensation in patients; however, when it remains increased, it contributes to the worsening of clinical manifestations and myocardial damage. Similar to cardiac remodeling, the pathophysiological Frank-Starling mechanism is initially activated in an attempt to maintain compensation; nonetheless, when dilation is persistent, this mechanism results in the progression of myocardial damage and clinical manifestations of heart failure (HF) syndrome1-5. Ventricular remodeling is the process by which ventricular size, shape, and function are regulated by mechanical, neurohormonal, and genetic factors. It can be defined by molecular, cellular, and interstitial changes in the myocardium, resulting in alterations in the size, mass, geometry, and function of the heart as a result of a myocardial injury5. Its pathophysiological importance was well-demonstrated in the experimental studies with rats, conducted by the Pfeffer Keywords Heart Failure / therapy; Ventricular Remodeling; Stroke Volume / physiology; Prognosis. Mailing Address: José Rosino de Araújo Rocha Reis Filho • Hospital Santa Marcelina. Rua Santa Marcelina, 177, Itaquera. Postal Code 08270-070, São Paulo, SP – Brazil E-mail: [email protected], [email protected] Manuscript received October 18, 2014; revised manuscript January 5, 2015; accepted January 7, 2015. DOI: 10.5935/abc.20150025 502 and Pfeffer (initially, Marc and Janice). In the myocardial infarction model, they demonstrated that mortality in rats was strongly associated with the degree of cardiac dilation and reduced ejection fraction6,7. Infarcted rats with greater cardiac dilation and lower ejection fraction had poorer outcomes than those with less involvement6,7. The postinfarction period is conventionally divided into two phases: early (up to 72 h) and late (after 72 h)8. Initial remodeling involves the expansion of the infarcted area, which can result in ventricular rupture or aneurysm formation8. In the early stage, after a moderate to large infarction, the ventricular cavity increases in size due to expansion or to stretching and thinning of the infarcted segment8,9. Late remodeling comprises the ventricle as a whole and is associated with time-dependent dilation, ventricle shape distortion, and ventricular wall hypertrophy, which can continue for months to years8,9. Pfeffer and Pfeffer6 observed that rats with small infarctions (infarcted area < 20%) did not develop cardiac dilation and rats with moderate infarction (between 20% and 40% of infarcted area) presented progressive dilatation occurring in the noninfarcted area. The pathophysiological importance of cardiac remodeling and its role in HF prognosis have been expanded with the results of studies on ACE inhibitors in the treatment of infarcted rats. These studies have demonstrated that these drugs prevent cardiac remodeling and, in some cases, promote its reversal7. Rats treated with ACE inhibitors presenting dilation prevention or reverse remodeling had better prognosis than those that did not6,7. It was observed that the benefit of treatment was more significant in rats with moderate infarction7. In a subsequent study, Pfeffer et al.10 coordinated the SAVE study; they demonstrated that the concept of remodeling also applied to humans and that treatment with ACE inhibitors modified the natural course of myocardial infarction and myocardial infarction-associated HF. Patients with myocardial infarction and ejection fraction of < 40% treated with captopril exhibited approximately 40% reduction in cardiovascular events10. Other studies have demonstrated that this knowledge regarding cardiac remodeling could also be applied to patients with cardiac dilatation without myocardial infarction. Data from the Framingham study clearly documented that cardiac dilation was associated with HF11. Patients with cardiac dilation had a 1.47-fold risk of developing heart failure compared with those without dilation11. The role of cardiac remodeling has been highlighted in studies on HF, confirming these findings. In this context, the Val-HeFT study demonstrated that patients with the highest ventricular volumes and lowest baseline left ventricular ejection fractions presented higher mortality12. Cardoso et al. Reverse Cardiac Remodeling in HF Review Article Reverse ventricular remodeling Cardiac dilation is identified as an important marker of poor prognosis. Conversely, its reversal is associated with improved prognosis. Several studies have demonstrated that drugs or procedures, which modify ventricular remodeling, preventing or delaying cardiac dilation, are associated with improved outcomes. Not all drugs used in the treatment of HF influence cardiac remodeling. Animal studies in the postinfarction period have shown that beta-blockers, aldosterone blockers, and renin–angiotensin system inhibitors prevented cardiac dilation, whereas hydralazine and digitalis did not. Thus, clinical and experimental evidence suggests that the renin–angiotensin– aldosterone system and sympathetic nervous system play an important role in the process. ACE inhibitors, as demonstrated in the SOLVD studies, reduced the rate of cardiac dilation and, in initial forms, promoted regression in cardiac dilation10,13,14. Studies on angiotensin II receptor blockers demonstrated that these drugs also have a beneficial effect on ventricular remodeling. In the ELITE study, both patients receiving ACE inhibitors and those receiving angiotensin II AT1 receptor‑antagonists (ARB) presented the same trend regarding ventricular remodeling, with prevention of cardiac dilation. There were no differences in response between the ACE inhibitor and ARB treatments analyzed in that study14. Cardiac dilation is not reversed in all patients with HF and ventricular dysfunction. In patients with lesser involvement, reversal is not generally observed; it is more frequently identified in cases of moderate to intense involvement, with greater magnitude in the former7,10,12,14. Studies have shown reversal of cardiac dilation in approximately 30%–60% of the cases treated with neurohormonal blockers. In a study of outpatients over 70 years of age, Cioffi et al.15 observed an improvement in the ejection fraction in 36% during a mean follow-up of 17 months. Predictors for this improvement were absence of diabetes, history of hypertension, and treatment with beta-blockers; treatment with beta-blockers increased the chance of reversal by 3.4 times15. In the V-HeFT I and II studies, reverse remodeling was also observed both in the group treated with hydralazine and nitrate and that treated with enalapril16. A 5-unit increase in ejection fraction was the best predictor of mortality among the studied variables16. Approximately 30% of the patients had an increase in ejection fraction greater than 5 units; 50% of these presented an increase of more than 10 units. The improvement in cardiac remodeling has also been observed. In the IMPROVE-HF registry, which examined 3,994 patients hospitalized for compensation, ejection fraction increased over 10% in 28.6% of patients17. Increased adrenergic activity appears to have a greater role in ventricular remodeling. Studies have demonstrated that beta-blockers promoted a more intense reversal of cardiac dilation than ACE inhibitors (Figure 1). ACE inhibitors prevent ventricular dilation and promote small increases in ejection Figure 1 – ACE inhibitors prevent cardiac dilation and beta-blockers reverse it. Coh JN et al JACC 2000; 35: 569-82. Arq Bras Cardiol. 2015; 104(6):502-506 503 Cardoso et al. Reverse Cardiac Remodeling in HF Review Article fraction, but reduction in ventricular diameter and increase in ejection fraction are more significant with beta-blockers13,18. The current literature documents that adrenergic activity actually plays an important role in ventricular remodeling, greater than that of the renin–angiotensin system, at least in the most symptomatic forms of the disease. Conversely, the adrenergic system may not be greatly stimulated in the initial phases of ventricular dysfunction because blockage of this system in asymptomatic forms of ventricular dysfunction does not result in a very significant reduction in mortality, as demonstrated in the CAPRICORN study19. Prognosis and remodeling There is a growing body of evidence on the importance of reverse ventricular remodeling in HF prognosis 19-23. Patients who present regression of ventricular dilation or increased ejection fraction after treatment have better quality of life. At follow-up, Cioffi et al.15 demonstrated that patients with reverse cardiac remodeling had lower mortality (3%) compared with those who did not present reversal (22%). In the V-HeFT I study, mortality in the first year of follow-up for patients who had a reduction in ejection fraction greater than 6 units, an alteration in ejection fraction ranging between −5 and 5 units, and those who had an increase in ejection fraction greater than five units was 29%, 16%, and 6%, respectively16. Hoshikawa et al.18 observed that prognosis is related to the reversal of cardiac dilation. They divided their patients into three groups: those with full reverse cardiac remodeling, with LV diameter < 55 mm and Delta D fraction > 25%; those with partial reversal; and those who did not present reversal. The authors observed that all patients with no reversal of cardiac dilation died during the follow-up, which lasted an average of 5 years18. All patients who presented some reversal survived. In that study population, all patients were treated with neurohormonal blockers; 78% showed a reversal of cardiac dilatation and, of these, 57% showed complete reversal18. This same group reassessed their patients. Furthermore, Matsumura et al. 24 demonstrated the role of reverse remodeling in long-term prognosis. This study revealed that in 12 years of follow-up, all patients who had regression of cardiac dilation survived; however, those presenting increased dilation died or required transplantation. In this population of patients with dilated cardiomyopathy, it was observed that 35.6% of patients had some reversal; 37% of these presented normal diameters and ejection fractions24. All patients with some reversal remained alive at the end of 12 years, demonstrating that even small reversals indicate a good response to treatment24. In addition to the analysis of clinical trials and small group studies, reverse cardiac remodeling was assessed in 504 Arq Bras Cardiol. 2015; 104(6):502-506 a meta‑analysis involving 69,766 patients in 30 randomized trials25, which showed a strong relationship between improved ejection fraction and reduced mortality. Overall, mortality significantly decreased by 49% in patients presenting improved ejection fraction compared with those who did not25. Based on the regression analysis, a 5% increase in mean ejection fraction corresponded to a relative reduction of 14% in mortality (OR, 0.86; 95% CI, 0.77–0.96; p = 0.013). For each 5% absolute increase in ejection fraction, patients who presented reversals had a 4.9-fold higher chance of not dying compared with those showing no reversal. Similar results were described for the change in left ventricular volume25. Treatment and reverse remodeling Because prognosis is better in patients with reversed cardiac dysfunction, at least partially, reversal should be considered a primary treatment goal. Patients not presenting this reversal should have their treatment regimen reassessed. In the absence of reversal, they should be more carefully followed up because they are at risk for a poorer outcome. Effective treatment should reverse cardiac remodeling26-28. Notably, all effective drugs and procedures, such as cardiac resynchronization, promote the reversal of cardiac dilation18,29-32. Nonreversal may be a sign that the doses of prescribed medications are inadequate or that the disease severity is high, resulting in a failure to obtain desired response to a proposed treatment. In the treatment of HF, dosage is extremely important. Reverse remodeling is often not observed because the treatment drugs are administered at low doses. The importance of dosage can be observed in the FAST–Carvedilol study33. In this study, half of patients were discharged after using this drug at a dose of 3.125 mg or 6.25 mg twice daily, whereas the dosage for the remaining was rapidly increased during hospitalization and was the highest tolerated dose during discharge. At the outpatient clinic, dosage of carvedilol was not increased by the physicians for various reasons; this was most frequently because of borderline blood pressure. Thus, the average carvedilol dose was 6.99 mg/day in the control group and 16.19 mg/day in the intervention group. At follow-up, the intervention group presented a reversal of cardiac dilation; this reduction was already evident at 3 months of treatment (Figure 2)33. The group treated with low doses did not present reversal. At follow-up, in the first year, the survival rate was 43.5% in the control group versus 65.2% in the intervention group. The data draw attention to the importance of dosage both in reversing cardiac dilatation and reducing mortality and show that both are probably interconnected33. The authors of the present study have used these guidelines in clinical practice, increasing the dosage (particularly for beta-blockers) in patients who did not present reverse cardiac remodeling, thereby achieving a reversal of the dilation not obtained with the usual dosage. In patients whose heart rate is consistently above 70 bpm during optimized treatment, ivabradine has been effective in reversing cardiac dilation34. Cardoso et al. Reverse Cardiac Remodeling in HF Review Article Figure 2 - Beta-blockers used at the correct dosage reverses cardiac dilation; this reduction is already evident at 3 months of treatment. Melo D et al. JACC 2011; 57 (supl A): 17. Conclusion Cardiac dilation is a marker of poorer prognosis in patients with HF. The drugs used to treat HF, particularly beta-blockers, ACE inhibitors, and ARBs, promote reverse remodeling. Patients who present reverse remodeling during treatment have better outcomes and lower mortality than those who do not present it. Filho JRAR, Cardoso JN, Cardoso CMR, Barretto AC. Critical revision of the manuscript for intellectual content: Reis Filho JRAR, Cardoso JN, Cardoso CMR, Barretto AC. Potential Conflict of Interest No potential conflict of interest relevant to this article was reported. Author contributions Sources of Funding Conception and design of the research: Reis Filho JRAR, Cardoso JN, Cardoso CMR, Pereira-Barretto, AC. Acquisition of data: Reis Filho JRAR, Cardoso JN, Cardoso CMR, Barretto AC. Analysis and interpretation of the data: Reis Filho JRAR, Cardoso JN, Cardoso CMR, Barretto AC. Writing of the manuscript: Reis There were no external funding sources for this study. Study Association This study is not associated with any thesis or dissertation work. References 1. Bocchi EA, Marcondes-Braga FG, Bacal F, Ferraz AS, Albuquerque D, Rodrigues Dde A, et al. Atualização das diretrizes brasileiras de insuficiência cardíaca crônica 2012. Arq Bras Cardiol. 2012;98(supl 1):1-33. 5. 2. Jessup M, Brozena S. Heart failure. N Engl J Med. 2003;348(20):2007-18. 3. Colucci WS. Molecular and cellular mechanisms of myocardial failure. Am J Cardiol. 1997;80(11A):15L-25L. 6. Pfeffer MA, Pfeffer JM. Ventricular enlargement and reduced ventricular after myocardial infarction. Circulation. 1987;75(5 Pt 2):IV93-7. 4. Schrier RW, Abraham W. Hormones and hemodynamics in heart failure. N Engl J Med. 1999;341(8):577-85. 7. Zornoff LA, Cicogna AC, Paiva SA, Spadaro J. Remodelamento e seu impacto na progressão da disfunção ventricular. Rev Soc Cardiol Estado de São Paulo. 2002;12(3):371-8. Pfeffer MA, Pfeffer JM, Steinberg CR, Finn P. Survival after an experimental myocardial infarction: beneficial effects of long-term therapy with captopril. Circulation. 1985;72(2):406-12. Arq Bras Cardiol. 2015; 104(6):502-506 505 Cardoso et al. Reverse Cardiac Remodeling in HF Review Article 8. S u t t o n M G , S h a r p e N . L e f t v e n t r i c u l a r r e m o d e l i n g a f t e r myocardial infarction. Pathophysiology and therapy. Circulation. 2000;101(25):2981-8. 9. Patten RD, Udelson JE, Konstam MA. Ventricular remodeling and its prevention in the treatment of heart failure. Curr Opin Cardiol. 1998;13(3):162-7. 10. Pfeffer MA, Braunwald E, Moye LA, Basta L, Brown EJ Jr, Cuddy TE, et al. Effect of captopril on mortality and morbidity in patients with left ventricular dysfunction after myocardial infarction. Results of the survival and ventricular enlargement trial (SAVE). N Engl J Med. 1992;327(10):669-77. 11. Vasan RS, Larson MG, Benjamin EJ, Evans JC, Levy D. Left ventricular dilatation and the risk of congestive heart failure in people without myocardial infarction. N Engl J Med. 1997;336(19):1350-5. 12. Wong M, Staszewsky L, Latini R, Barlera S, Glazer R, Aknay N, et al. Severity of left ventricular remodeling defines outcomes and response to therapy in heart failure Val-HeFT echocardiographic data. J Am Coll Cardiol. 2004;43(11):2022-7. 13. Sabbah HN, Shimoyama H, Kono T, Gupta RC, Sharov VG, Scicli G, et al. Effects of long-term monotherapy with enalapril, metoprolol, and digoxin on the progression of left ventricular dysfunction and dilatation in dogs with reduced ejection fraction. Circulation. 1994;89(6):2852-9. 14. Konstam MA, Pattern RD, Thomas I, Ramahi T, La Bresh K, Goldman S, et al. Effects of losartan and captopril on left ventricular volumes in elderly patients with heart failure: results of the ELITE ventricular function sub study. Am Heart J. 2000;139(6):1081-7. 15. Cioffi G, Stefenelli C, Tarantini L, Opasich C. Prevalence, predictors and prognostic implications of improvement in left ventricular systolic function and clinical status in patients > 70 years of age with recently diagnosed sustolic heart failure. Am J Cardiol. 2003;92(2):166-72. 506 22. Bristow MR, Gilbert EM, Abraham WT, Adams KF, Fowler MB, Hershberger RE, et al. Carvedilol produces dose-related improvements in left ventricular function and survival in subjects with chronic heart failure. Circulation. 1996;94(11):2807-16. 23. Levine TB, Levine AB, Keteyian SJ, Narins B, Lesch M. Reverse remodeling in heart failure with intensification of vasodilator therapy. Clin Cardiol. 1997;20(8):697-702. 24. Matsumura Y, Hoshikawa-Nagai E, Kubo T, Yamasaki N, Furuno T, Kitaoka H, et al. Left ventricular reverse remodeling in long-term (>12 years) survivors with idiopathic dilated cardiomyopathy. Am J Cardiol. 2013;111(1):106-10. 25. Kramer DG, Trikalinos TA, Kent DM, Antonopoulos GV, Konstam MA, Udelson JE. Quantitative evaluation of drug or device effects on ventricular remodeling as predictors of therapeutic effects on mortality in patients with heart failure and reduced ejection fraction: a Meta-Analytic approach. J Am Coll Cardiol. 2010;56(5):392-406. 26. Oliveira GH, Mukerji S, Hernandez AV, Qattan MY, Banchs J, Durand JB, et al. Incidence, predictors, and impact on survival of left ventricular systolic dysfunction and recovery in advanced cancer patients. Am J Cardiol. 2014;113(11):1893-8. 28. Kramer DG, Trikalinos TA, Kent DM, Antonopoulos GV, Konstam MA, Udelson JE. Quantitative evaluation of drug or device effects on ventricular remodeling as predictors of therapeutic effects on mortality in patients with heart failure and reduced ejection fraction. J Am Coll Cardiol. 2010;56(5):392-406. 29. de Groote P, Delour P, Mouquet F, Lamblin N, Dagorn J, Hennebert O, et al. The effects of b-blockers in patients with stable chronic heart failure: predictors of left ventricular ejection fraction improvement and impact on prognosis. Am Heart J. 2007;154(3):589-95. 16. Cintron G, Johson G, Francis G, Cobb F, Cohn JN. Prognostic significance of serial changes in left ventricular ejection fraction in patients with congestive heart failure. Circulation. 1993;87(6 Suppl):VI17-23. 30. Cioffi G, Stefenelli C, Tarantini L, Opasich C. Chronic left ventricular failure in the community: prevalence, prognosis and predictors of the complete clinical recovery with return of cardiac size and function to normal in patients undergoing optimal therapy. J Card Fail. 2004;10(3):250-7. 17. Wilcox JE, Fonarow GC, Yancy CW, Albert NM, Curtis AB, Heywood JT, et al. Factors associated with improvement in ejection fraction in clinical practice among patients with heart failure: findings from IMPROVE-HF. Am Heart J. 2012;163(1):49-56.e2. 31. Konstam MA, Rousseau MF, Kronemberg MW, Udelson JE, Melin J, Stewart D, et al. Effects of the angiotensin converting enzyme inhibitor enalapril on the long-term progression of left ventricular dysfunction in patients with heart failure. Circulation. 1992;86(2):431-8. 18. Hoshikawa E, Matsumura Y, Kubo T, Okawa M, Yamasaki N, Kitaoka H, et al. Effect of left ventricular reverse remodeling on long-term prognosis after therapy with angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers and betablockers in patients with idiopathic dilated cardiomyopathy. Am J Cardiol. 2011;107(7):1065-70. 32. Chan AK, Sanderson JE, Wang T, Lam W, Yip G, Wang M, et al. Aldosterone receptor antagonism induces reverse remodeling when added to angiotensin receptor blockade in chronic heart failure. J Am Coll Cardiol. 2007;50(7):5916. 19. Dargie HJ. Effect of carvedilol on outcome after myocardial infarction in patients with left ventricular dysfunction: the CAPRICORN randomized trial. Lancet. 2001;357(9266):1385-90. 33. Cioffi G, Tarantini L, de Feo S, Pulignano G, Del Sindaco D, Stefenelli C, et al. Pharmacological left ventricular reverse remodeling in elderly patients receiving optimal therapy for chronic heart failure. Eur J Heart Fail. 2005;7(6):1040-8. 20. Steimle AE, Stevenson LW, Fonarow GC, Hamilton MA, Moriguchi JD. Prediction of improvement in recent onset cardiomyopathy after referral heart transplantation. J Am Coll Cardiol. 1994;23(3):553-9. 34. Melo D, Pereira-Barretto AC, Ramires JA. The impact of rapid use of betablockers on ventricular remodeling and mortality in end-stage heart failure. J Am Coll Cardiol. 2011;57(Suppl A):17. 21. Kawai K, Takaoka H, Hata K, Yokota Y, Yokoyama M. Prevalence, predictors, and prognosis of reversal of maladaptive remodeling with intensive medical therapy in idiopathic dilated cardiomyopathy. Am J Cardiol. 1999;84(6):671-6. 35. Swedberg K, Komajda M, Bohm M, Borer JS, Ford I, Dubost-Brama A, et al; SHIFT investigators. Ivabradine and outcomes in chronic heart failure (SHIFT): a randomized placebo-controlled study. Lancet. 2010;376(9744):875-85. Erratum in: Lancet. 2010;376(9757):1988. Arq Bras Cardiol. 2015; 104(6):502-506 Back to the Cover Letter to the Editor An Issue Waiting to be Clarified: Effects of the QT Prolonging Drugs on Tp-e Interval Omer Yiginer, Mehmet Dogan, Emrah Erdal Gulhane Military Medical Academy, Haydarpasa Training Hospital, Department of Cardiology, Selimiye – Istanbul We read the article ‘Impact of Psychotropic Drugs on QT Interval Dispersion in Adult Patients’ by Claudio et al. with great interest1. They investigated in this study the effects of psychotropic drugs on QT interval (QTI), corrected QT interval (QTc), and QT dispersion (QTd). They concluded that psychotropic drugs increased QTd and QTc interval. QTd is the most frequently used non-invasive method to quantify electrical myocardial heterogeneity. However, there are variable results in studies related to QTI due to the technical limitations in measurements2. It is well-known that the reproducibility of QTI measurements is low both in manual and automatic measurements2. In this study, the measurements were performed digitally by four cardiologists using the Preview software with a magnification of 300%. We appreciated the method used in this study in order to obtain more accurate data. It is recommended that measurements be done digitally at least by two cardiologists2. Quantifying electrical myocardial heterogeneity and transmural dispersion of repolarization (TDR) was introduced in the beginning of 2000’s3. The myocardium Keywords Psychotropic /drugs therapeutic; Electrocardiography; Cardiovascular Diseases; Torsades de Pointes; Ventricular Fibrillation; Death, Sudden. comprises 3 distinct myocyte types - namely, endocardial, epicardial, and midmyocardial M cells3. Although these myocytes are morphologically similar, they exhibit different electrophysiological characteristics. M cells have typically the longest action potential. Furthermore, when myocardium is exposed to conditions prolonging the repolarization phase, such as bradycardia or agents, the action potential duration of the M cells are more prolonged than in the other cells3. While repolarization of the epicardial region ends at the peak of T-wave, repolarization phase of M cells ends at the end of T wave3. Therefore, the time between the peak and end of the T wave is called Tp-e interval, as an index of TDR. The role of the TDR in the prediction of possible life‑threatening arrhythmic events has been demonstrated in the Brugada, short-QT and long-QT syndromes and coronary artery disease3. Previously, we showed that TDR was increased in patients with obstructive sleep apnea and chronic arsenic exposure4,5. However, there is no study investigating the effects of QT prolonging drugs on TDR. The repolarization phase of myocytes in midmyocardial and endocardial layers may be more influenced by the drugs. In this context, psychotropic drugs may be increasing QT interval duration via Tp-e interval prolongation. In conclusion, it seems that adding the data related to Tp-e interval to the study results might have completely illuminated the effects of psychotropic drugs on electrical heterogeneity of myocardium in many respects. Mailing Address: Mehmet Drogan • Gulhane Military MEdical Academy. Selimiye Uskudar. Postal Code 34688, Selimiye – Istanbul E-mail: [email protected] Manuscript received November 11, 2014; revised manuscript November 11, 2014; accepted January 19, 2015. DOI: 10.5935/abc.20150037 References 1. Claudio B de Q, Costa MA, Penna F, Konder MT, Celoria BM, Souza LL, et al. Impact of psychotropic drugs on QT interval dispersion in adult patients. Arq Bras Cardiol. 2014;102(5):465-72. 2. Malik M, Batchvarov VN. Measurement, interpretation and clinical potential of QT dispersion [Review]. J Am Coll Cardiol. 2000;36(6):1749-66. 3. Gupta P, Patel C, Patel H, Narayanaswamy S, Malhotra B, Green JT, et al. T(p-e)/QT ratio as an index of arrhythmogenesis. J Electrocardiol. 2008;41(6):567-74. 507 4. Kilicaslan F, Tokatli A, Ozdag F, Uzun M, Uz O, Isilak Z, et al. Tp-e interval, Tp-e/QT ratio, and Tp-e/QTc ratio are prolonged in patients with moderate and severe obstructive sleep apnea. Pacing Clin Electrophysiol. 2012; 35(8):966-72. 5. Yildiz A, Karaca M, Biceroglu S, Nalbantcilar MT, Coskun U, Arik F, et al. Effect of chronic arsenic exposure from drinking waters on the QT interval and transmural dispersion of repolarization. J Int Med Res. 2008;36(3):471-8. Yiginer et al. Effects of the QT prolonging drugs on Tp-e interval Letter to the Editor Answer to Letter to Editor We appreciate the authors’ interest in our study and the valuable contributions on the subject. The spatial dispersion of ventricular repolarization can occur in the transmural, trans-septal or apical-basal direction.1,2. A large number of publications has been dedicated to the study of cell diversity of the human myocardium and its heterogenic response to pharmacological agents. Researchers such as Antzelevitch et al.3 and Luo e Rudy4 have tested several models in normal hearts and individuals with congenital long-QT syndrome, concluding that the properties of the M cell action potential critically participate on QT interval dispersion, mainly in the presence of drugs with binding capacity in the IKr and IKs channels1,5. artery disease model, Karaman et al.6 found an association between increased QT dispersion and the Tp-e interval with slowed coronary flow in coronary angiography (TIMI 1) in patients with acute coronary syndrome, when compared to the control group (TIMI 3)6. In our study, we chose to measure the QT dispersion, as it is a powerful tool that can be fully incorporated by general practitioners that prescribes psychotropic drugs in the routine monitoring of a potentially fatal complication of their patients7. However, we expect the Tp-e interval, considering its solid results in the literature, also to become a routine tool in the increasingly frequent use of these drugs. Under this idea, in fact, the measurement of Tp-e is conceptually an electrocardiographic correlation truthful to the abovementioned concepts. In a recent article, in the coronary Sincerely, Bruno de Queiroz Claudio References 1. Antzelevitch C. The role of spatial dispersion of repolarization in inherited and acquired sudden cardiac death syndromes. Am J Physiol Heart Circ Physiol. 2007;293(4):H2024-38. 4. 2. Restivo M, Caref EB, Kozhevnikov DO, El-Sherif N. Spatial dispersion of repolarization is a key factor in the arrythmogenicity of long QT syndrome. J Cardiovasc Electrophysiol. 2004;15(3):323-31. 5. Antzelevitch C, Shimizu W. Cellular mechanisms underlying the long QT syndrome. Curr Opin Cardiol. 2002;17(1):43-51. 3. Antzelevitch C, Shimizu W, Yan GX, Sicouri S, Weissenburger J, Nesterenko VV, et al. The M cell: its contribution to the ECG and to normal and abnormal electrical function of the heart. J Cardiovasc Electrophysiol. 1999;10(8):1124-52. Luo CH, Rudy Y. A dynamic model of the cardiac ventricular action potential. I. Simulations of ionic currents and concentration changes. Circ Res. 1994;74(6):1071-96. 6. Karaman K1, Altunkaş F, Cetin M, Karayakali M, Arısoy A, Akar I, Zencir C, Aygüç B, Celik A. New Markers for Ventricular Repolarization in Coronary Slow Flow: Tp-e Interval, Tp-e/QT Ratio, and Tp-e/QTc Ratio. Ann Noninvasive Electrocardiol. 2014 Sep 30. [Epub ahead of print] Arq Bras Cardiol. 2015; 104(6):507-508 508 Back to the Cover Clinicoradiological Session Case 5/2015 – Late Outcome of Corrected Aortopulmonary Window in A 23-Year-Old Female Patient Who Underwent Surgery in Childhood Edmar Atik Clínica Privada Dr. Edmar Atik, São Paulo, SP – Brazil Clinical data: At 10 months of age, the patient underwent correction of a large aortopulmonary window and mitral valve regurgitation secondary to volume overload, which caused severe heart failure. The post-operative clinical outcome was favorable. Prior to operation, her clinical picture was of concern because of severe malnutrition (weight of 5,500 g), congestive heart failure (tachypnea of 60 bpm), hepatomegaly (liver palpable at 4 cm of the right costal margin), severe cardiomegaly, and increased pulmonary vasculature. Cardiovascular examination showed left ventricular (LV) enlargement; thrill and systolic murmur in the mitral area; accentuated S2; marked LV overload on electrocardiogram (ECG); mitral regurgitation due to incomplete leaflet coaptation; and pulmonary systolic pressure of 60 mmHg. At surgery, the 2-cm-diameter window between the pulmonary trunk and ascending aorta (Ao) was closed, and plication of the posterior ring of the mitral valve was performed. There was an immediate clinical response with hemodynamic stabilization, resolution of the heart murmur and heart failure, and subsequent normal weight gain. Medication for congestive heart failure was discontinued at 4 years of age, when the cardiac silhouette had returned to normal. To date, the patient tolerates routine exercises well and does not report any symptoms. Physical examination: good general state of health, normal breathing, acyanotic, normal pulses. Weight: 53 kg; height: 165 cm; blood pressure on right arm (BPRA): 105/75 mmHg; heart rate (HR): 76 bpm. Aorta not palpable on the suprasternal notch. The apical impulse was not palpable in the precordium, and there were no systolic impulses. Normal heart sounds, no heart murmurs. Liver not palpable. Laboratory tests ECG (Figure 1) at 22 years of age showed normal sinus rhythm with no signs of overload, and normal ventricular repolarization. PA = +10o, QRSA = +50o, TA = +50o (lower tracing). ECG prior to operation, at 10 months of age (upper Keywords Aortopulmonary Window/surgery; Heart Defects, Congenital/surgery; Infant. Mailing Address: Edmar Atik • Rua Dona Adma Jafet, 74, conj. 73, Bela Vista. Postal Code 01308-050. São Paulo, SP – Brazil E-mail: [email protected] ; [email protected] Manuscript received July 24, 2014; revised manuscript October 06, 2014; accepted October 06, 2014. DOI: 10.5935/abc.20150062 e55 tracing), showed marked left ventricular overload, with QRSA = +70o, PA = +20o and TA = +80o; RS morphology (amplitudes of 24 and 30 mm) from V1 to V3 and QRs (amplitudes of 10, 50 and 3 mm) from V4 to V6; Sokolow index of 90 mm; no ventricular repolarization abnormalities. Chest radiograph showed normal cardiac silhouette (cardiothoracic ratio = 0.46) and pulmonary vasculature (Figure 2). In the image prior to surgery, these parameters were markedly increased, with a cardiothoracic ratio of 0.85 (Figure 2). Echocardiogram showed normal size cardiac chambers (Ao = 34; left atrium − LA = 36, right ventricle − RV = 13, LV = 49; ejection fraction − EF = 61%, septum = posterior wall = 8 mm); no mitral regurgitation. Echocardiogram prior to surgery showed enlargement of left chambers (LA = 37, Ao = 17 and LV = 42; RV = 10, septum = posterior wall = 5 mm; EF = 82%), with marked mitral regurgitation. Clinical diagnosis: Aortopulmonary window with mitral regurgitation secondary to volume overload and severe heart failure resolved after surgical correction and favorable late outcome until adulthood. Clinical reasoning: The postoperative clinical elements were consistent with normal cardiovascular parameters, unlike in the preoperative period, in which the overt manifestations of heart failure suggested the diagnosis of congenital heart defect expressed by signs of mitral regurgitation. On that occasion, the aortopulmonary window was diagnosed during surgery, and mitral regurgitation was secondary to and resulted from the volume overload caused by the defect. LV overload on ECG confirmed the magnitude of the volume overload, which predominated over the RV pressure overload. Differential diagnosis: other defects accompanied by severe arterial left-to-right shunt, such as ductus arteriosus and arteriovenous fistulas, should be remembered in this context. Management: In view of the marked consequences of the arterial shunt, the surgery for closure of the interarterial defect not only repaired the secondary dilatation of the mitral annulus, but also resulted in cure, thus surpassing the concern about pulmonary arterial hypertension at the time. Commentaries: aortopulmonary window usually has important manifestations early in the first months of life, and cardiac surgery corrects the signs and symptoms of heart failure and associated defects such as those of secondary mitral regurgitation, which was present in the case reported1-3. Generally, pulmonary arterial hypertension also subsides, and so does the secondary dilatation of the different correlate cardiac structures. This is encouraging, given the important implications of this defect, which should be corrected right after diagnosis. The return of anatomical and functional parameters to normal, in this case, becomes of great value as an example of outcome for similar cases in an early period of life. Edmar Atik Late Outcome of Surgically Corrected Aortopulmonary Window Clinicoradiological Session Figure 1 – Electrocardiograms at two timepoints: in the preoperative period, at 10 months of age (upper tracing), and at late postoperative period at 22 years of age (lower tracing). These electrocardiograms show resolution of the left ventricular overload initially observed. Figure 2 – Chest radiographs in the preoperative period and later at 23 years of age, after surgical correction performed at 10 months of age, showing markedly enlarged and normal cardiac silhouette, respectively. Arq Bras Cardiol. 2015; 104(6):e55-e57 e56 Edmar Atik Late Outcome of Surgically Corrected Aortopulmonary Window Clinicoradiological Session References 1. Soares AM, Atik E, Cortêz TM, Albuquerque AM, Castro CP, Barbero-Marcial M, et al. Aortopulmonary window. Clinical and surgical assessment of 18 cases. Arq Bras Cardiol.1999;73(1):59-74. 2. Barnes ME, Mitchell ME, Tweddell JS Aortopulmonary window. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu. 2011;14(1):67-74. e57 Arq Bras Cardiol. 2015; 104(6):e55-e57 3. Atik E, Barbero-Marcial M, Andrade JL, Baucia JA, Iwahashi E, Aiello V, et al. [Clinical manifestation of aortopulmonary window as mitral regurgitation caused by secondary dilatation of the valvar anulus]. Arq Bras Cardiol. 1994;63(6):493-5. Back to the Cover Case Report Acute Myocardial Infarction and Severe Prosthetic Dysfunction after Bentall Procedure Viviane Tiemi Hotta, Pedro Gabriel de Melo Barros, Paulo Sampaio Gutierrez, Angela Cristina Pasiani Bolonhez, Wilson Mathias, Ricardo Ribeiro Dias InCor / Faculdade de Medicina da Universidade de São Paulo, São Paulo, SP - Brazil Introduction Coronary artery anastomotic dehiscence is a rare complication following aortic procedures. A 59-year-old male previously underwent replacement of the ascending aorta and aortic valve because of ascending aorta aneurysm and severe aortic regurgitation. Eight years after the procedure, he presented with acute myocardial infarction. Transesophageal echocardiography (TEE) and coronary angiography revealed coronary artery dehiscence. This finding rarely occurs after a Bentall procedure; however, if it does, it usually occurs in the early postoperative period and is associated with an infectious etiology. In this case, coronary dehiscence presented with myocardial infarction years after the procedure and was first suspected after TEE. Case Report A 59-year-old male presented with chest pain and breathlessness of three days’ duration, which was rapidly deteriorating. Eight years ago, he had undergone a classical Bentall procedure because of ascending aorta aneurysm and severe aortic regurgitation. He had been treated with beta blockers, angiotensin-converting enzyme inhibitors, statin for systemic arterial hypertension and dyslipidemia control, and oral anticoagulants. On physical examination, blood pressure was 130/40 mmHg and heart rate was 74 beats/minute. On cardiac auscultation, a mechanical click with a systolic murmur and a high-pitched aortic diastolic murmur at the left sternal border radiating toward the apex was noted. Electrocardiogram revealed left bundle branch block. Chest X-ray showed mild pulmonary congestion, enlarged mediastinum, and aortic mechanical prosthesis. There was an increase in myocardial necrosis markers. A thoracic computed tomography (CT) angiogram was performed to evaluate aortic dissection, which was inconclusive, and a TEE was performed. Keywords Myocardial Infarction; coronary ostium dehiscence, Bentall procedure, prosthetic aortic valve disfunction Mailing Address: Viviane Tiemi Hotta • Unidade Clínica de Miocardiopatias do InCor/FMUSP. Avenida Doutor Enéas Carvalho de Aguiar, 44. São Paulo, Postal Code 05403-000. São Paulo, SP - Brazil. Email: [email protected], [email protected] Manuscript received June 26, 2014; revised manuscript July, 23, 2014; accepted July, 28, 2014. DOI: 10.5935/abc.20140199 e58 Transthoracic echocardiogram showed moderate left ventricular systolic dysfunction due to anterior and apical akinesia and severe dysfunction of the aortic mechanical prosthesis (severe aortic regurgitation). TEE evaluation evidenced solutions of continuity causing turbulent leakage flow between the Dacron graft on the ascending aorta and the aneurismal native aorta (Figure 1) was also observed. Moreover, severe aortic central and periprosthetic regurgitation was noted. The oral anticoagulant therapy was withdrawn, and low‑molecular-weight heparin (enoxaparine) therapy was initiated. After normalization of the international normalized ratio, coronary angiography was performed and showed no significant lesions on the coronary arteries. On the 12 th day after acute myocardial infarction, the patient underwent a Cabrol procedure (Figure 2A); intraoperative findings revealed disconnection of both the left and right coronary ostium from the graft and a periprosthetic leak. The patient was discharged on the 14th postoperative day without complications. Discussion Coronary ostial anastomoses dehiscence is a rare complication following aortic procedures1-6. Regarding the etiologies related to this unusual finding, infection of aortocoronary vein graft suture lines is the most common cause of this condition and some cases may be associated with early postoperative Staphylococcus aureus superficial wound infection. In this case, the patient presented with late clinical features several years after the surgical procedure; and the anatomopathological examination7,8 revealed no signs of infection in the aorta specimen and Dacron prosthesis (Figure 2B). Dehiscence of the coronary ostial anastomoses may also occur more frequently in patients with connective tissue diseases or other genetically defined aortopathies like Marfan syndrome. In these patients, recurrence of life‑threatening cardiovascular manifestations is not uncommom. Other aspects related to dehiscence of the coronary graft concern to technical details during the Bentall procedure like increased bleeding or difficulties of hemostasis, limiting the reestablishment of coronary flow, a crucial aim of the composite graft-valve procedures like Bentall De Bono technique. In this case, the patient had an unremarkable evolution after the Bentall procedure. Subclinical manifestations of early infection after the first procedure may have passed unnoticed and may have been associated with periprosthetic Hotta et al. Cardiac complications after bentall procedure Case Report Figure 1 – TTE images showing severe regurgitation of the aortic prosthesis on continuous (A) and pulsed wave Doppler (B) mappings in the apical five-chamber view. TEE images of the color M-mode of the left ventricular outflow tract (LVOT; C) and color Doppler study (D) evidencing severe aortic prosthetic regurgitation. TEE transverse plane imaging showing the solutions of continuity between the Dacron prosthesis and native aorta (E and F, arrows). TEE imaging, at 145º, depicting the LVOT and color Doppler study (G and H). TTE: transthoracic echocardiography; TEE: transesophageal echocardiography; LA: left atrium; LV: left ventricle; RV: right ventricle; RA: right atrium; AO: Aorta; LVOT: left ventricle outflow tract; AR: Aortic regurgitation. leaks. Moreover, technical problems may have contributed to dehiscence formation. Small leaks can progress along the years and evolve late after surgery into pseudoaneurysms and other variable clinical features depending on the site of the aortic dehiscence and involvement of the surrounding structures. In this patient, dehiscence of the coronary ostium was diagnosed due to an acute myocardial infarction secondary to inadequate coronary flow resulting from graft dehiscence since atherosclerotic coronary artery disease was excluded by coronary angiography. Late postoperative aortic graft dehiscence may occur rarely after Bentall procedure and in this case, it was first suspected after TEE evaluation. Advantages of the classical Bentall technique are graft cover up using the remaining aortic tissue and immediate protection against bleeding during the perioperative period; disadvantages include pseudoaneurysm formation. This is why the modified Bentall procedure is currently the most used operation for aortic root reconstruction using a valved graft. CT aortography can be helpful in the diagnosis of this complication9, but in this case, it was inconclusive. TEE showed solutions of continuity on the Dacron graft in the ascending aorta and the native aorta, raising the suspicion of coronary ostium dehiscence that was further confirmed by intraoperative examination. The patient underwent a Cabrol procedure with no complications (Figure 2A). Complete coronary artery dehiscence is an exceptional cause of pseudoaneurysm after a Bentall procedure. So far, there are very few case reports with this disorder presenting as acute myocardial infarction. Additionally, in our case, there was no evidence of infection and diagnosis was possible by means of TEE. Arq Bras Cardiol. 2015; 104(6):e58-e60 e59 Hotta et al. Cardiac complications after bentall procedure Case Report Figure 2 – A) Post operatory aspect after Cabrol procedure. B) Histological section of a fragment of the aorta removed during surgery, showing fibrosis at the adventitia (indicated by arrows) and very mild mononuclear inflammatory infiltrate (hematoxylin & eosin staining). References 1. Haddy SM. Aortic pseudoaneurysm after Bentall procedure. J Cardiothorac Vasc Anesth. 1999;13(2):203-6. 2. Shinohara K, Ishikura F, Tanaka N, Asaoka N, Nakasone I, Masuda Y, et al. Diagnosis of coronary artery dehiscence and pseudoaneurysm after modified Bentall operation by Doppler color flow imaging: a case report. J Cardiol. 1994; 24(6):475-9. 3. Barbetseas J, Crawford ES, Safi HJ, Coselli JS, Quinones MA, Zoghbi WA. Doppler echocardiographic evaluation of pseudoaneurysms complicating composite grafts of the ascending aorta. Circulation. 1992; 85(1):212-22. e60 4. Cujec B, Bharadwaj B, Chait P, Hayton R.Dehiscence of the proximal anastomosis of aortocoronary bypass graft. Am Heart J. 1990; 120(5): 1217-20. 5. Rice MJ, McDonald RW, Reller MD. Diagnosis of coronary artery dehiscence and pseudoaneurysm formation in postoperative Marfan patient by color flow Doppler echocardiography. J Clin Ultrasound . 1989; 17(5):359-65. Arq Bras Cardiol. 2015; 104(6):e58-e60 6. Monney P, Pellaton C, Qanadli SD, Jeanrenaud X. Aortic pseudo-aneurysm caused by complete dehiscence of the left coronary artery 7 years after a composite mechanical-valved conduit aortic root replacement (Bentall operation). Eur Heart J. 2012; 33(1):60. 7. Smith P, Qureshi S, Yacoub MH. Dehiscence of infected aortocoronary vein graft suture lines. Cause of late pseudoaneurysm of ascending aorta. Br Heart J.1983;50(2):193-5. 8. Douglas BP, Bulkley BH, Hutchins GM. Infected saphenous vein coronary artery bypass graft with mycotic aneurysm. Fatal dehiscence of the proximal anastomosis. Chest. 1979;75(1):76-7. 9. Ceviz M, Becit N, Gündogdu F, Unlü Y, Kantarci M. Pseudoaneurysm of the left coronary ostial anastomoses as a complication of the modified Bentall procedure diagnosed by echocardiography and multislice computed tomography. Heart Surg Forum. 2007;10(3):E191-2.
Baixar