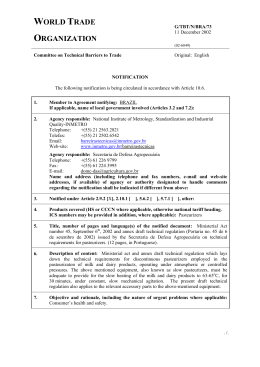
Artigo Original The demand for assistance from the nursing staff in a human milk bank and its motivations A procura por assistência da equipe de enfermagem em um banco de leite humano e suas motivações Cristiane Taís Antunes Neles Soares1, Maria Celestina Bonzanini Grazziotin2, Adriana Maria Wan Stadnik3, Eduardo Borba Neves4 Abstract A practice with a big impact on reducing child and maternal mortality, breast-feeding should be encouraged to promote physical, mental, and emotional health to the child and mother. From this consideration, the central purpose of this study was to investigate the reasons for women to seek assistance from nursing staff of a milk bank. The central objective is to seek explanations for the complaints of mothers and it suggests ways to promote this practice among women, based on the idea that the process of information, education, health promotion, and human interaction are part of the work of nursing staff. This is a retrospective study, exploratory-descriptive, quantitative, and qualitative analysis performed by individual medical records of women seen from January to December, 2009. We have identified 14 different categories of complaints in 380 consultations examined. The main reasons pointed out were: relief milking, mastitis, milk bank guidance and breast-feeding, breast engorgement, and to get wrongly. It is suggested that beyond the technical issues of how to make, professional guidance promotes human health, and the involvement of the nursing staff can be fundamental in the establishment and maintenance of the practice of exclusive breast-feeding. Keywords: milk, human; breast feeding; gift giving. Resumo Prática de grande impacto na redução da mortalidade infantil e materna, o aleitamento materno deve ser estimulado para promoção da saúde física, mental e psíquica da criança e da nutriz. Partindo-se dessa consideração, o objetivo central deste estudo foi verificar as razões que levaram mulheres a buscar a assistência da equipe de enfermagem de um banco de leite. O referencial adotado, além de procurar explicações para as queixas das nutrizes, sugere formas de promoção dessa prática entre as mulheres, partindo da ideia de que o processo de informação, educação, promoção da saúde e interação humana fazem parte do trabalho da equipe de enfermagem. Trata-se de uma pesquisa retrospectiva, exploratório-descritiva, quantiqualitativa, realizada pela análise das fichas de atendimento individual das mulheres atendidas de janeiro a dezembro de 2009. Foram identificadas 14 diferentes categorias de queixas em 380 atendimentos analisados. Os principais motivos levantados foram: ordenha de alívio, mastite, orientação sobre banco de leite e amamentação, ingurgitamento mamário e pega errada. Sugere-se que, para além das questões técnicas de como fazer, haja orientação profissional em sentido à promoção da saúde humana, e o envolvimento da equipe de enfermagem pode ser fundamental para o estabelecimento e para a manutenção da prática do aleitamento materno exclusivo. Palavras-chave: leite humano; aleitamento materno; doações. Trabalho realizado na Universidade Tecnológica Federal do Paraná – Curitiba (PR), Brasil. 1 Enfermeira da Unidade de Saúde Augusta da Prefeitura Municipal de Curitiba – Curitiba (PR), Brasil. 2 Professora do Centro Universitário Campos de Andrade – Curitiba (PR), Brasil. 3 Professora do Departamento Acadêmico de Educação Física, campus Curitiba, Universidade Tecnológica Federal do Paraná (UTFPR) – Curitiba (PR), Brasil. 4 Professor do Programa de Pós-graduação em Engenharia Biomédica, campus Curitiba, UTFPR – Curitiba (PR), Brasil. Endereço para correspondência: Eduardo Borba Neves – Rua Marquês do Paraná, 418 – apartamento 104 – Água Verde – CEP 80620-210 – Curitiba (PR), Brasil – E-mail: [email protected]. Fonte de financiamento: nenhuma. Conflito de interesses: nada a declarar. Cad. Saúde Colet., 2011, Rio de Janeiro, 19 (3): 327-33 327 Cristiane Taís Antunes Neles Soares, Maria Celestina Bonzanini Grazziotin, Adriana Maria Wan Stadnik, Eduardo Borba Neves INTRODUCTION Breast-feeding is a practice of great impact on reducing infant and on maternal mortality and it should be encouraged to promote the physical, mental, and emotional child and mother health. Although scientifically proven its superiority over artificial formulas, exclusive maternal breast-feeding (EMB) in Brazil is far from the levels agreed by the World Health Organization (WHO) and the Ministry of Health (MOH), and the trend to early weaning is still evident. The WHO together with the United Nation Children’s Fund (UNICEF) and the MOH recommend EMB for about six months and maintenance of supplemented breast-feeding by two years or more1,2. According to data from the Second Survey of the Prevalence of Breast-feeding3, the average days of EMB in state capitals in Brazil are only 54 days. The same authors, Venâcio and Monteiro4, in another study, compared national estimates of the frequency of breast-feeding (regardless of the receipt of other foods) and they observed an increasing trend of breast-feeding in Brazil between 1974 and 1989 – especially because in previous decades breast-feeding was declining in the country –, with its increasing median duration from 2.5 to 5.5 months. Importantly, this tendency was mainly seen in urban areas in South-Central region of the country and among women of higher income and education, highlighting the importance and need for education, with more than just schooling, the really crucial is access to information – that in our reality is usually easier to those who have access to school education. Breast-feeding strengthens the affective bond between mother and son; provides nutrients and important immune substances for growth and development of children. It also provides benefits to the mother, family, and society from the standpoint of biological, psychosocial, and environmental fields5,6. During the prenatal, pregnant women should be counseled on the benefits of breast-feeding for mother and baby. Education and preparation in this period are the key element to a successful breast-feeding, which should be initiated soon after birth, in the first hours after childbirth, and breast milk should be offered on free demand. While breast-feeding is a natural process, unlike what happens to other mammals, human breast-feeding is not an instinctive act – mother and baby need support to learn how to and to breastfeed7. Thus, remembering that learning is directly related to the educational process, it becomes essential, which is highlighted by the WHO as one of the criteria for a person to be considered healthy, the health knowledge and access to medical care, in other words, health education and opportunity to have and use infrastructure – human and material resources in health8. 328 Cad. Saúde Colet., 2011, Rio de Janeiro, 19 (3): 327-33 At the same time, we believe that in addition to education, there is need for adequate preparation for new social role as mothers, or mother again. Bear in mind that education is not a solitary act, it is a society demand and, according to Ferreira9, it is the engine of social transformation of individual predispositions, and it ensures the adaptation of the individual belonging to a particular society and its social groups living together. Health professionals have an important role in programs of health education in prenatal care and the postpartum/ breast-feeding. To perform these functions, technical expertise, clinical skills, listening, supporting, and helping women to make decisions on breast-feeding management are needed, because the mothers need to be assisted and supported in fulfilling their new role in society, women’s mother7,10. One of the strategies of the National Breastfeeding Policy for reducing child mortality, promoting, protecting, and supporting breast-feeding is the human milk bank (HMB), which are specialized centers necessarily tied to a hospital of maternal/child health11. Mello et al.12 suggest that deep and lasting changes will happen only if the healthy public policy operates accordingly. The HMB first appeared in Brazil in 1943, in the National Institute of Pediatrics, now called Instituto Fernandes Figueira. From 1943 to 1985, the HMB had as its main objective the collection and distribution of human milk to meet only the special cases, such as prematurity, nutritional disorders, and allergies to heterologous proteins, and it did not follow clinical priorities nor worried with stimulating (for giving encouragement) to the return to breast-feeding. Only since 1985, with the rupture of the original paradigm, there was a real expansion in the number of HMBs11,13. Currently there are approximately 199 HMB registered in the Brazilian Network of Human Milk Banks Network (HMB-BR), 28 in the Southern region and 8 in the state of Paraná, all following the laws (Board Resolution – RDC/ANVISA No. 171, September 2006), which regulate the operation11,14,15. The actions performed by nurses in promoting and encouraging breast-feeding in milk banks go beyond technical skills, because it must provide its customers the full nursing care in relation to physical, emotional, social, spiritual, and cultural wellness. “You must keep up expanding their technical, scientific and cultural benefit of customers, community and development of the profession, promoting and/or facilitating technical development, scientific and cultural staff under his guidance and supervision”, article 18 and 19 of the Ethics Codes for Professional Nursing16. According to Mello et al.12, professional skills in the areas of health are no longer unique and autonomous, in that the Nursing staff in a human milk bank variety in competency intersects and articulates. For Fujimori et al.17, who conducted a research on breast-feeding, it is necessary that health professionals know the aspects that hinder or facilitate the establishment and maintenance of breastfeeding to guide actions. Another example of the importance of health professionals’ education is seen in a survey developed by the MOH on breast-feeding, in the State capitals and Federal District3, it was found that the introduction of water, tea, juice, milk, and other supplementary foods in infant feeding generally occurred early, during which the researchers considered the fundamental role of health professionals to reduce this picture. Despite efforts made towards education and promotion of breast-feeding in Primary Care, Baby Friendly Hospitals (in supporting the ten steps to successful breast-feeding) and national initiatives, for example, the Breast-feeding Network Brazil program, HMB are being sought by many mothers, not only to make a donation, but as a source of help to solve their difficulties in breast-feeding. Currently, milk banks are no longer just a local collection and distribution to promote, protect and support breast-feeding11,15. The creation of HMB is now a global incentive and has shown that human milk, milked and fed to the baby when he/she is momentarily unable to receive it directly by sucking the breast has shortened the period of hospitalization of premature infants, showing a good gain of weight and a more rapid improvement of clinical frame11,18,19. In the view of this and the dissemination of the activities by HMB, through the media, aiming to raise donated breast milk, many mothers with babies to term, without too much milk for donation, had been looking for the HMB to receive help practice of breast-feeding and to answer their questions. Thus, this study aims at identifying the reasons for women to seek assistance from the nursing team in a HMB in Curitiba city, trying to understand also the role of health education actions. After evaluating the records of each call made and to survey the main complaints, it will be possible to know, within the researched reality, which aspects of breast-feeding, scientific knowledge and pedagogical training are needed to be trained or improved. Therefore, we hope to offer a quality service and to have results and a positive impact on the prevalence of exclusive breast-feeding in the first six months of life, which are the goals proposed by the WHO and MOH, seeking to offer a collaboration from the standpoint of a study beyond its descriptive and quantitative aspect. This is focused in checking the reality and transforming it, when it is possible, through the presentation of the results of research. METHODOLOGY This is a retrospective field, exploratory-descriptive, quantitative and qualitative study, carried out in the HMB of the Clinical Hospital of Paraná, one of the reference centers in breast-feeding, which serves the customers of Curitiba, the areas nearby, and other metropolitan cities in the State of Paraná. In the present study, the medical records of individual nursing of pregnant and lactating women, who attended the milk bank at the hospital, were selected and analyzed, from January to December, 2009. The individual medical records, standardized by the medical department, contained only the fields for the source of the patient (internal or external at the hospital), age and central complaint. For this study, all patients were selected from pregnant and lactating women outside, for a total sample of 380 attendances. The research project was submitted to the Ethics Committee on Research of the Clinics Hospital of Paraná, with protocol approval No 2278.172/2010-07. Reasons that lead women to seek a hmb The HMB at the Clinics Hospital of Paraná was initiated in 1978 and became a reference in the State. This unit carries out health promotion, protection, and support of breastfeeding and performs collection activities of human milk, collecting on average 200 L of human milk per month20. In the Milk Bank, the steps of selecting, sorting, processing, quality controlling, and distributing donated milk are carried out to meet the nutritional needs of preterm infants in hospital, to provide them a better quality of life and to reduce the infant mortality21,22. The sample consisted of pregnant and lactating women aged from 14 to 42 years, who sought care in the milk bank at the Clinics Hospital of Curitiba, in 2009, obtaining a mean age of 28.14 years-old. This study identified 14 different categories of complaints from a total of 380 visits made in 2009. All women who sought the assistance of the nursing staff were treated for aspects of guidance to health and the practice maneuvers required for relief of main complaint by nursing team, when necessary. Table 1 shows the frequency distribution of the main complaints. Relief milking In this study it was found that from the total attendance of 380 women, 22.1% sought assistance for carrying out relief milking, so this is the complaint that stood out with greater frequency. This happens due to a normal physiological response, because the rapid influx of milk, swelling, vascular congestion, and lymphedema of the breast tissues, the physiological process of milk letdown, the breasts may become painful, hot, Cad. Saúde Colet., 2011, Rio de Janeiro, 19 (3): 327-33 329 Cristiane Taís Antunes Neles Soares, Maria Celestina Bonzanini Grazziotin, Adriana Maria Wan Stadnik, Eduardo Borba Neves Table 1. Frequency distribution of the main complaints of women who sought the milk bank in Curitiba, Paraná, in 2009 Main complaint Relief milking Mastitis – Pain (signs of inflammation) Guidance on the human milk bank and breast-feeding Breast engorgement Takes the breast in a wrong way Orientation about donation Inhibition of lactation Low production of human milk Nipple injury Milking-son to return to work Twinning Flat or inverted nipples Lactose intolerance Re-lactation Total and heavy. However, even with these characteristics, a nurse targeted is capable of performing milking without difficulty to hand press, but if this practice is not carried out effectively, it will result in stasis of milk flow leading to complications, such as breast engorgement23. Importantly, when the baby cannot enter the nipple in the mouth because the breast is too full, there is an excess of milk, the baby is unable to drain both breasts at each feeding, and their infants are unable to breast-feed (premature, weak or sick), or breast-feeding women present conditions that would contraindicate it, the mothers should be advised to do the relief milking23. Mastitis The frequency of reported mastitis complaints by women seen at HMB was 21.6%, with one of the highest rates. Mastitis is characterized by an inflammation of one or more segments of the breast (the most commonly affected is the upper left quadrant), which may progress or not for a bacterial infection. Preventive measures are the same used in the breast engorgement24. The puerperal mastitis is an acute infection in the breast that affects from 2 to 6% of the breast-feeding mothers, especially new ones23. Mastitis usually occurs in the second and third weeks after birth and rarely after the 12th week. The accumulated milk, inflammatory response and tissue damage, such as cracks, allow entry of bacteria (the most common being Staphylococcus aureus and albus, Escherichia coli and Streptococcus), favoring the onset of infection. The flavor of milk is altered, becoming saltier due to increased levels of sodium and decreased levels of lactose, which can cause rejection of milk by infants. Maternal fatigue is also a risk factor for mastitis2. The breast with 330 Cad. Saúde Colet., 2011, Rio de Janeiro, 19 (3): 327-33 Frequency 84 82 44 40 32 31 17 16 16 10 5 1 1 1 380 Percent 22,1 21,6 11,6 10,5 8,4 8,2 4,5 4,2 4,2 2,6 1,3 0,3 0,3 0,3 100 Cumulative percent 22,1 43,7 82,4 54,2 62,6 70,8 91,1 86,6 95,3 97,9 99,2 99,5 99,7 100 ---- mastitis have heat, swelling, pain, hypersensitivity, increased volume, induration, pus may develop into an abscess, fever, malaise and chills25. Guidance on breast-feeding and HMB Of the 380 women who sought assistance from the milk bank, 11.6% had doubts about the management of breastfeeding and would like guidance and clarification on the criteria needed to become donors. According to ANVISA11, healthy women who have lactic secretion superior to the requirements of their child and who are willing to donate the surplus of their own free will are considered donors. According to Dias26, in a study conducted at University Hospital in Maringá city in 2006, 14.6% of women had not received any information from professionals about breast-feeding. It is considered a fundamental educational work to promote human health, and it is composed with excellence part of daily professional. Going forward, in relation to breast-feeding, according to Fujimori et al.17, even though health professionals are maintained in the EMB to provide guidance in the first six months of the baby, information is not enough, it is necessary involvement. It was found that everyday situations are specific to each woman and depends on their experiences, with particular need for quick service at the time of crises, which are more common in the first days and weeks after delivery. Furthermore, more experienced people, usually family members, have great influence on behavior related to breast-feeding, especially for being with these women in their day-to-day. It is understood that not enough women want to breastfeed and to have technical knowledge about it, so that the Nursing staff in a human milk bank practice is necessary to establish support within their peculiarities. According to Tardif e Lessard27, the profession of nursing, as many others in this line, is one of the most recognized professions as “social interaction”, which demand improvement of human relations and the ways to dealing with the other that is always a human being, in constant transformation and, usually, in care situation. By this point of view, to understand and to get involved with the patient is part of the profession and should be highly valued. Breast engorgement From the population studied, 10.5% sought by the HMB complained of breast engorgement. Breast engorgement is characterized by congestion of the breast28 and can promote the voltage of the areola and nipple flattening, damaging the handle by the baby. It can be caused by a clogged duct, accumulation of milk and non-removing of dead cells by the breast29. The predisposing factors are inadequate emptying of the breasts and the inhibition of milk letdown reflex30. The woman is at increased volume of the breasts, sensitivity to touch, redness, pain, and may or may not have fever and chills, and the milk does not flow easily. In prevention, Giugliani7 recommended to start breast-feeding as soon as possible, on free demand, using the correct techniques. According to a study conducted at the HMB from the University Hospital of Londrina city, in 2005, from donated breast milk, 65% had sought treatment at HMB by problems related to breast-feeding, especially, breast engorgement, and from this assistance becoming a donor31. Breast engorgement (the fourth most frequently complaint in this study) is related to difficulties with the handling of the breasts during the lactation period, often due to lack of guidance from professionals during prenatal care in the hospital soon after birth, whose care would help prevent it. By knowing that this change is related to excessive milk in the breast, the mother who has the problem should become a donor of milk to HMB, if properly supported and assisted. Takes the breast in a wrong way It was noted that 8.4% of women were receiving care for incorrect way to maneuver the breasts. Breast-feeding should not be a painful process, though most women feel a slight pain or discount at the beginning of it, which is considered normal. Nipple damage by improper positioning and way of touching are one of the most common causes of pain in breast-feeding. Very sore and hut nipples, though very common, they are not normal. Therefore, to solve these problems, women that are breast-feeding need support and guidance since its initiation, because if these complaints are not resolved and/ or minimized, they could cause complications and result in abandonment of breast-feeding24. Guidance for donation According to the survey, only 8.2% of pregnant women and nursing mothers looked for the milk bank to resolve their doubts concerning the donation of breast milk. According to Felipe e Almeida18, in a survey conducted in the Public Maternity Hospital of the City of Rio de Janeiro in 2003, only a percentage of 26.9% of mothers had been counseled on donated breast milk for the HMB. A study conducted in the milk bank at the University Hospital of Londrina city, in 2005, showed that from the donors interviewed 37.4% received clarification and information about donation and existence of HMB by health professionals31. Other complaints The search for nipple injury complaints showed a level of 4.2% (Table 1) and it is known that this complaint is directly related to management and may be incorrect. The percentage of complaints for flat or inverted nipples was 0.3%, as shown in Table 1, and it is known that the type of nipple, from the perspective of anatomy, has little influence on the establishment and success of breast-feeding and it assumes a secondary role in the determination of nipple trauma. Clearly, the most common cause of pain during breast-feeding is the nipple trauma by inadequate positioning and wrong way to get the breasts. The demand for assistance to inhibit lactation was 4.5%. Inhibition of lactation or ablactation is a technique usually adopted when it is necessary to stop milk production. It is recommended for lactating women after death of baby or neonatal to suppress lactation, to prevent vertical transmission of HIV and Hepatitis C, and when the infant has some pathology that would contraindicate breast-feeding, such as galactosemia32. The procedure for lactation inhibition is simple, it is made by milking of relief, if there is any excess milk, apply cold compresses for about ten minutes, bandage up the breast and guide to use tight bra and liquid restriction. The use of drug to inhibit lactation is used only in special cases, with medical prescription32,33. The average age of women presented was of 28.14 years. However, mothers who sought care for complaints of lactation inhibition obtained a significant increase, their average age was of 32.15 years and it may also be related to the physiCad. Saúde Colet., 2011, Rio de Janeiro, 19 (3): 327-33 331 Cristiane Taís Antunes Neles Soares, Maria Celestina Bonzanini Grazziotin, Adriana Maria Wan Stadnik, Eduardo Borba Neves ological weaning, when the child is already in the ideal age and the woman stops to produce milk, which prevents leaks. For complaints of low milk production, there was a 4.2% percentage. According to studies by Giugliani24 and Lana33, diseases, such as breast engorgement, nipple trauma, mastitis and low milk production, are important factors that may predispose to complications of lactation. The demand for assistance from the milk bank for milk to son, from returning to work had a frequency of 2.3 and 1.3% for twins. The percentage of mothers seeking care for re-lactation was 0.3% and for guidance on lactose intolerance, 0.3%. These attendance figures are considered as natural since it is known that health education, and in this case of new mothers, is an ongoing process and should be performed by professionals trained in the techniques of breast-feeding, in order that these women have better chances of overcoming problems and have higher rates of success in breast-feeding. FINAL CONSIDERATIONS This study revealed that the main reasons leading women to seek the HMB – in order of visit frequency –, were: relief milking, mastitis and guidance, both on breast-feeding, and on donation, triggering the importance of work and educational information on health promotion. These situations are susceptible of clarification in clinical prenatal and/or postpartum, which would provide information and involvement beyond the technical and scientific knowledge. Regarding other complaints, like child milking in order to be able to return to work, it is obviously a social issue, only raised but not discussed in this paper, which deserves further studies. For flat or inverted nipples, lactose intolerance and re-lactation were found to each of these complaints just a service, considering they should be cited, but in this study they are not considered essential. Once there are guidance and information, most questions tends to improve the quality of the experience of breast-feeding. It is essential that professionals who assist breast-feeding mothers appreciate not only the physical events and physiological, but also psychological factors arising during breast-feeding. It is up to health professionals, from primary to the hospital level, to listen to complaints and problems reported by women, respect their individuality and inspire confidence so that they can together solve the problems presented during breast-feeding. It should be reminded that not enough women want to breast-feed and have technical knowledge about it, so that the practice established is necessary to support within their peculiarities and that all health professionals must comply with this educational and informative role. Information collected in this study is useful for planning strategies at all levels of care. It is recommended continuous education to help promoting, protecting, and supporting breast-feeding in order, objectively, that the health professional knows the problems that can arise from breast-feeding and offer reliable guidance for the mother and baby to help them solve their problems. Referências 1. Venâncio SI. Dificuldades para o Estabelecimento da Amamentação: O papel das Práticas Assistenciais das Maternidades. J Pediatr. 2003;79(1): 1-2. 2. Brasil. Ministério da Saúde. Secretaria da Atenção à saúde. Departamento de Atenção Básica. Saúde da Criança: Nutrição Infantil: Aleitamento materno e alimentação complementar (Série A. Normas e Manuais Técnicos1ª, Caderno de Atenção Básica, n.23). 1ª ed. Brasília: Editora do Ministério de Saúde; 2009. 3. Brasil. Ministério da Saúde. Secretaria da Atenção à saúde. Departamento de Ações Programáticas e Estratégicas. II Pesquisa de Prevalência de Aleitamento Materno nas Capitais Brasileiras e Distrito Federal (Série C. Projetos, programas e relatórios). 1ª ed. Brasília: Editora do Ministério de Saúde; 2009. 4. Venâncio SI, Monteiro CA. A tendência da prática da amamentação no Brasil nas décadas de 70 e 80. Rev Bras Epidemiol. 1998;1(1):40-9. 5. Barros SMO, Marin HF, Abrão ACFV. Enfermagem Obstétrica e Ginecológica: Guia para a prática assistencial. 1ª ed. São Paulo: Roca; 2002. 332 Cad. Saúde Colet., 2011, Rio de Janeiro, 19 (3): 327-33 6. Campestrini S. Súmula de Aleitamento Materno. Curitiba: PUCPR; 2006. 7. Giugliani ERJ. O Aleitamento Materno na Prática Clínica. J Pediatr. 2000;76(Suppl 3): S238-52. 8. Barth NA. A saúde como ferramenta educacional estratégica na formação de cidadãos com especialidade na área tecnológica. [dissertação]. Florianópolis: UFSC; 2001. 9. Ferreira F. Para o estudo das identidades profissionais. In: Ferreira F, Monteiro M, Sarmento T. Formação e identidades. Braga: Centro de Formação das Escolas de Paredes de Coura; 2003. p. 33-53. 10. King FS. Como ajudar as mães a amamentar. Tradução de Zuleika Thomson e Orides Navarro Gordon. 4ª ed. Brasília: Ministério da Saúde; 2001. 11. Brasil. Agência Nacional de Vigilância Sanitária. Banco de leite humano: funcionamento, prevenção e controle de riscos/ Agência Nacional de Vigilância Sanitária. Brasília: ANVISA; 2008. Nursing staff in a human milk bank 12. Mello ALSF, Moysés ST, Moysés SJ. A universidade promotora de saúde e as mudanças na formação profissional. Interface. 2010;14(34): 638-92. 22. Hospital de Clínicas necessita de doadoras de leite materno. Gazeta do Povo. Caderno Vida e Cidadania. Curitiba; 2010. p. 43. [Cited 2010 Sep 18]. Available from: http://www.gazetadopovo.com.br. 13. Almeida JAG. Amamentação: um híbrido natureza-cultura. Rio de Janeiro: FIOCRUZ; 1999. 23. Corintio MN. Aleitamento Materno. Manual de Orientação. São Paulo: Ponto Febrasgo; 2006. 14. Brasil. Agência Nacional de Vigilância Sanitária. Resolução RDC nº 171, de 4 de setembro de 2006. Dispõe sobre o Regulamento Técnico para o Funcionamento de Bancos de Leite Humano. Brasília, DF: Diário Oficial da União; 2006. 24. Giugliani ERJ. Problemas Comuns na Lactação e seu Manejo. J Pediatr. 2004;80(Suppl 5):S147-54. 15. Fundação Oswaldo Cruz. Portal da Rede Brasileira de Bancos de Leite Humano. Bancos de Leite Humano no Brasil. [cited 2010 Sept 16]. Available from: http://www.fiocruz.br/rdeblh/cgi/cgilua.exe/sys/star. htm?sid=356. 16. Conselho Federal de Enfermagem. Resolução COFEN Nº 240/2000 sobre o Código de Ética dos Profissionais de Enfermagem. [cited 2010 Apr 15]. Available from: http://www.portalcoren-rs.gov.br/web/ resolucao/r240.htm. 17. Fujimori E, Nakamura E, Gomes MM, Jesus LA, Rezende MA. Aspectos relacionados ao estabelecimento e à manutenção do aleitamento materno exclusivo na perspectiva de mulheres atendidas em uma unidade básica de saúde. Interface. 2010;14(33):315-27. 18. Felipe SF, Almeida MFPV. A orientação e incentivo da doação de leite materno para os bancos de leite humano durante o pré-natal. Cuidado é fundamental. 2005;1(2):49-56. [cited 2010 May 12]. Available from: http://www.unirio.br/repef/2005.html. 19. UFPR. Semana Mundial do Aleitamento Materno. Jornal do Hospital de Clínicas – UFPR. Curitiba; 2009. Ed. 124, p. 5. [cited 2010 Sept 18]. Available at: http://www.hc.ufpr.br/. 20. Carriel P. Campanha Incentiva Doação de Leite Materno. Gazeta do Povo, Curitiba; 2009. p. 12. [cited 2010 Sept 18]. Available from: http:// www.gazetadopovo.com.br. 21. Grazziotin AL, Grazziotin MC, Letti LAJ. Disposal of human milk donated to a human milk bank before and after measures to reduce the amount of milk unsuitable for consumption. J Pediatr. 2010;86(4):290-4. 25. Bastos KCB, Peixoto MMLV, Rodrigues RCB. Manual de Qualidade dos Procedimentos em Banco de Leite; 2005. [cited 2010 Sep 17]. Available from: http://www.meac.ufc.br/blh/arquivos_pdf/normas_rotinas_blh_meac.pdf. 26. Dias RC, Baptista IC, Gazola S, Rona MSS, Matioli G. Perfil das doadoras do banco de leite humano do Hospital Universitário de Maringá, Estado do Paraná, Brasil. Acta Sci Health Sci. 2006;28(2):153-8. 27. Tardif M, Lessard C. O trabalho docente: Elementos para uma teoria da docência como profissão de interações humanas. Petrópolis: Vozes; 2005. 28. Silva JC. Manual obstétrico: um guia prático para enfermagem. 2ª ed. São Paulo: Corpus; 2007. 29. Orshan SA. Enfermagem na Saúde das Mulheres, das Mães e dos Recém nascidos: o Cuidado ao Longo da Vida. Porto Alegre: Artmed; 2010. 30. King FS. Como ajudar as mães a amamentar. Brasília: Ministério da Saúde; 1995. 31. Santos DT, Vannuchi MTO, Oliveira MMB, Dalmas JC. Perfil das doadoras de leite do banco de leite humano de um hospital universitário. Maringá. Acta Sci. 2009;31(1):15-21. 32. Meira MM, Ibarra AS, Santos EKA. Inibição da lactação: (re) visitando a literatura. Rev Eletr Enferm. 2008;10(3):805-15. 33. Lana APB. O Livro de Estímulo à Amamentação: uma visão biológica, fisiológica e psicológica: comportamental da amamentação. São Paulo: Editora Atheneu; 2001. Recebido em: 23/02/2011 Aprovado em: 21/07/2011 Cad. Saúde Colet., 2011, Rio de Janeiro, 19 (3): 327-33 333
Download