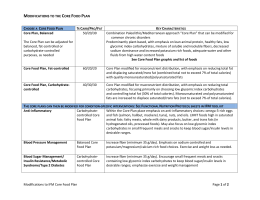
Artigo original Association of fat intake and socioeconomic status on anthropometric measurements of adults Associação do consumo de gorduras e do nível socioeconômico sobre as medidas antropométricas de adultos Katia Cristina Portero-McLellan1, Gustavo Duarte Pimentel2, Jose Eduardo Corrente3, Roberto Carlos Burini4 ABSTRACT We aimed to identify the influence of dietary fat profile on body mass index (BMI) and waist circumference (WC) in a middleclass general population sample. A cross-sectional study of 448 adults aged 35-85 years was carried out from January 2004 to December 2007. Patients were divided in two groups according to family income: Group 1 (G1) with higher income, and Group 2 (G2) with lower income. Demographic and socioeconomic status were identified, along with anthropometric data, health eating index (HEI) and dietary profile. The groups were similar with respect to gender, age, BMI and WC. HEI was higher in G1 due to a higher intake of protein (+12.8%), dairy products (p<0.001), higher intake of vegetables (p<0.01), fruit (p<0.001), and less dietary fat (-9.8%). The main contribution of fats was saturated fat for G1 (+5.0%) and polyunsaturated fat for G2 (+14.4%). Besides differences in socioeconomic status the groups had similar BMI and abdominal fatness. Only differences in fat profile were correlated with the anthropometric measures mostly explained by the lower vegetable oil intake in higher income participants. Key words: Dietary fats, anthropometry, food consumption, diet RESUMO O objetivo do estudo foi identificar a influência das gorduras dietéticas sobre o índice de massa corporal (IMC) e a circunferência abdominal (CA) em uma amostra populacional de adultos. O estudo tranversal foi realizado com 448 adultos, entre 35 e 85 anos, de janeiro de 2004 a dezembro de 2007. Os indivíduos foram divididos em dois grupos de acordo com a renda familiar: Grupo 1 (G1) com maior renda, e Grupo 2 (G2) com menor renda. Foram levantadas variáveis socioeconômicas e demográficas, juntamente com variáveis antropométricas, índice de alimentação saudável (IAS) e perfil dietético. Os grupos foram semelhantes quanto ao gênero, à idade, ao IMC, e à CA. O IAS foi maior no G1 em decorrência do maior consumo de proteínas (+12,8%), laticínios (p<0.001), maior consumo de hortaliças (p<0,01), frutas (p<0,001), e menor de gordura (-9,8%). A maior contribuição das gorduras foi a saturada para o G1 (+5,0%) e a polinsaturada para o G2 (+14,4%). Apesar das diferenças socioeconômicas os grupos foram similares quanto ao IMC e à adiposidade abdominal. As diferenças no perfil do consumo de gorduras foram correlacionadas com as medidas antropométricas e puderam ser explicadas pelo menor consumo de óleo entre os indivíduos de renda mais elevada. Palavras-chave: Gorduras na dieta, antropometria, consumo de alimentos, dieta Doutora em Ciências. Professora do Departamento de Saúde Pública da Faculdade de Medicina de Botucatu da Universidade Estadual Paulista (Unesp). End.: Rua Taiaçu, 77 - Piracicaba (SP) - CEP: 13432-506 - E-mail: [email protected] 2 Mestrando em Nutrição pela Universidade Federal de São Paulo (Unifesp). 3 Livre Docente. Professor Adjunto da Unesp. 4 Livre Docente. Professor Titular da Unesp. 1 266 Cad. Saúde Colet., 2010, Rio de Janeiro, 18 (2): 266-74 Association of fat intake and socioeconomic status on anthropometric measurements of adults Introduction Nutrition transition is a widely studied global phenomenon that is characterized by an abandonment of traditional diets that are high in fiber, grains, fruits, and vegetables; and increasing modern diets that are high in fat, sugar, and salt (Popkin, 2002). Effects of the nutrition transition include increase in obesity rates and other non-communicable chronic diseases. The most dramatic effects of this transition are found in developing countries because of the impact it has on nutrition deficiencies and the rapid growth of the population (Popkin, 2002). The ongoing increase in adult obesity in Brazil has been occurring among all groups of men and women with a higher proportion of increase among lower income families (Monteiro et al., 1995). A very noticeable change in the income-obesity relationship is indicated by the following facts: (1) income and body mass index (BMI) are inversely related among the 30% richest women; (2) a higher prevalence of female obesity (15.4%) occurs in 40% of the middle-income group; and (3) 30% of the poorest Brazilian women (9.7% prevalence) can no longer be considered to be protected from obesity (Monteiro et al., 1995). In recent years the dietary pattern of the Brazilian population has been changing (Levy-Costa et al., 2005; Molina et al., 2007). Levy-Costa et al. (2005) examined data from household budget surveys from 1974 to 2003 that showed time-trends in metropolitan areas indicating a decline in the consumption of traditional food (rice and beans); noticeable increases in the consumption of processed items such as cookies and soft drinks (Mondini & Monteiro, 1994; Monteiro et al., 2000); a continued excessive consumption of sugar; and a continued increase in total fat and saturated fat content in the diet. These changes represent an important negative dietary pattern trend in the country and may represent an important health risk factor (Monteiro et al., 2000). Patterns and trends regarding food availability in Brazilian households are consistent with the increasing presence of chronic non-communicable diseases in morbidity and mortality, and with the continuous increase in the prevalence of obesity (Levy-Costa et al., 2005). Studies on Brazilian food consumption, specifically involving adults, have been conducted preferentially in state capitals and their metropolitan regions (Fornes et al., 2000; 2002; Salvo & Gimeno, 2002; Sichieri et al., 2003; Bonomo et al., 2003; Chor et al., 2003; Newmann et al., 2007). Moreover, only a few diet studies have been performed within the Brazilian population to observe the relationship between food consumption and body composition (Fornes et al., 2002; Bonomo et al., 2003; Castanheira et al., 2003; Fisberg et al., 2006; Peixoto et al., 2007; Molina et al., 2007). For this reason, we aimed to identify the influence of dietary fat intake on BMI and WC in a Brazilian middle-town population, and the demographic and socioeconomic effects of these associations. Research design and methods The Lifestyle Changing Program (LISC) that was offered to patients with non-communicable chronic diseases consisted of regular physical exercise and nutritional counseling. TheSão Paulo State University Medical School of Botucatu, SP, Brasil, Metabolism, Exercise and Nutrition Center (CeMENutri), has been conducting this LISC program since 1992, in Botucatu, which is a city located in the center of São Paulo State, about 230 km west of the capital city of São Paulo and has a population of 121,274 (IBGE, 2006). Crops (including corn, sugarcane, beans, and fruits) grown in the region are processed in Botucatu, which also has foundries, textile mills, bakeries, and factories producing buses, auto parts, and agricultural and industrial machinery. Goods are shipped by railroad and highway to the city of São Paulo. The City Hall conducts four major food-supply programs for the lowincome population: food-kit fellowship, community garden, community bakery, and life-milk program (for every child in a public school). The inclusion criteria for LISC participants are people over the age of 35, of both genders, with at least one of the metabolic syndrome components and/or comorbities, and without metabolic or motor disabilities that would limit physical exercise. The subject data came from the baseline of people who joined the program between 2004 and 2007. Subjects gave their written consent to participate in this study, which was approved by the Medical Ethics Committee of São Paulo State University (Comitê de Ética em Pesquisa da Faculdade de Medicina de Botucatu da Universidade Estadual Paulista “Júlio de Mesquita Filho” – Unesp). Subjects and study design A cross-sectional observational study of 448 adults, aged 35-85 years (predominantly Caucasian) was carried out from January 2004 to December 2007. Patients were divided in two groups according to family income: Group 1 (G1) with higher income (n=285), and Group 2 (G2) with lower income (163). We excluded subjects with diabetes, renal, liver, or heart diseases; or chronic alcohol intake before starting this study. Demographic data and socioeconomic status Participants were classified by gender, range of age (< and ≥ 60 years), family income (measured in monthly minimal income (MI), 1 MI=U$ 250.00) and education (years of school). Cad. Saúde Colet., 2010, Rio de Janeiro, 18 (2): 266-74 267 Katia Cristina Portero-McLellan, Gustavo Duarte Pimentel, Jose Eduardo Corrente, Roberto Carlos Burini Dietary intake Usual dietary intake data was determined using a 24hour recall. The diet was documented by trained personnel, and to obtain precise information, the subjects were asked how often they usually ate during the day, what variety of food was consumed, how the food was prepared, what the serving size was, and what the brand of the food/meal was. The diets were analyzed with the software NutWin® (2002) version 1.5, and the principal nutrients of interest were energy, protein, fat (saturated, mono and polyunsaturated), cholesterol, carbohydrates, and dietary fiber. Mean individual nutrient intakes per day were computed using the NutWin database and Brazilian food tables (IBGE, 1999; Phillippi, 2002; Nepa, 2004). The Healthy Eating Index (HEI) modified for the Brazilian population was used to assess the quality of the participants’ diet (Mota et al., 2008). The original HEI was developed based on a 10component system of five food groups with a total possible index score of 100 (Kennedy et al., 1995). This method was adapted for the Brazilian population based on the Brazilian food guide (Philippi et al., 1999) that has 8 food groups and 12 components to measure the variety of food intake. Each of the 12 components has a score ranging from 0 to 10, so the total possible index score is 120. Body composition Weight and height were measured with a Filizola® electronic scale (capacity and precision in grams), and a stadiometer (precision in millimeters). WC was measured halfway between the lower rib region and the iliac crest in the recumbent position after a normal exhale. BMI and WC were evaluated according to The World Health Organization (1998a). Statistical analysis Statistical analyses were conducted with SAS software for windows (SAS version 9.1.3., SAS Institute, Inc., Cary, NC). Descriptive statistics were performed for the study and continuous variables are presented as mean±standard deviation (SD). Categorical variables are presented as absolute numbers and percentages. Continuous variables were compared by the independent test t. The percentage of total energy intake attribuited to fat: total, saturated (SFA), monounsaturated (MUFA), and polyunsaturated (PUFA), was calculated by multiplying each individual’s fat intake in grams by 9 kcal/g, dividing the product by individual energy intake, and then multiplying by 100. The nutrients of the diet were adjusted for total energy intake to control for confounding as recommended in published literature (Willett et al., 1997). Fat intake values were categorized as quintiles after adjusting for age, 268 Cad. Saúde Colet., 2010, Rio de Janeiro, 18 (2): 266-74 gender, BMI and WC and were analyzed by chi-square test. ANOVA and Tukey tests were used to compare the differences between quintiles. Simple logistic regression analyses were used to determine the association of dietary fat intake, and body composition using two models: the first was adjusted for demographic data such as age, gender, income, and education; and the second was additionally adjusted for energy intake and HEI. Results from the logistic regression are presented, and odds ratios (ODs) with 95% confidence interval (CI) were calculated. The results are discussed based on a significance level of 5% (p<0.05). Results Groups were similar statistically by gender, age, BMI, and WC (Table 1). Subjects from G1 had a higher educational level (p<0.001) and higher income (p<0.001) than subjects from G2. They also had a higher HEI (p<0.001) along with higher concentration of protein (% energy), lower total fat (% energy), and lower PUFA (% energy). The distribution of normal and elevated values for BMI between groups showed similar prevalence for overweight and obesity, and regarding WC, a slightly higher (6.2%) prevalence of values elevated in G2. Subjects from G1 showed better HEI than G2 as a result of eating more energy as protein (+12.8%) and carbohydrates (5.5%) and less as lipid (-9.8%). The main contribution for fat intake was SFA for G1 (+5.0%) and PUFA for G2 (+14.4%). Both groups exhibited poor intake of MUFA and similarly lower amounts of fibers (Table 2). Table 3 shows the distribution of the HEI components in both groups. HEI was higher in G1 due to a higher intake of protein from dairy products (1.5 servings/day versus 0.8, p<0.001), higher intake of vegetables (1.5 servings/day versus 1.0, p<0.01), and higher intake of fruit (2.5 servings/day versus 0.0, p<0.001). The lower educated and lower income group had a poor quality diet characterized by higher caloric intake as total fat and PUFA reflecting a higher vegetable oil intake. MUFA as well as fiber intake were similarly lower in both groups (Table 4). Relative risks of BMI>25 and WC>88 (female) and >102 (male) according to the quintiles of oil intake are shown in Table 5. After adjusting for age, gender, education, and income individuals from the G2 in the third quintile were 0.07 (95% CI 0.007-0.07) times more likely to have a BMI>25. Additionally adjusting for energy intake and HEI, the same group of individuals were 0.06 (95% CI 0.006-0.06) times more likely to have a BMI>25. The higher intake of oil in G1 and G2 was not significantly associated with BMI and WC. Association of fat intake and socioeconomic status on anthropometric measurements of adults Table 1 - Sociodemographic, anthropometric and dietary characteristics of the studied groups Sociodemographic Gender Male Female Age, years Education Income Anthropometric BMI WC Dietary HEI Energy, kcal Carbohydrates, % Carbohydrates, g/kg Protein, % Protein, g/kg Total Fat, % energy Total Fat, g/kg SFA, % energy SFA, g/kg MUFA, % energy MUFA, g/kg PUFA, % energy PUFA, g/kg Cholesterol, mg Vegetable Oil, serving Fiber, g G1 Groups G2 P-value* 75 (26.3) 210 (73.7) 52.47 (9.93) 3.44 (2.05) 2.58 (1.03) 41 (25.2) 122 (74.8) 53.93 (10.70) 1.39 (1.06) 1.67 (0.72) 0.7876 29.74 (6.05) 96.28 (15.02) 28.91 (5.20) 96.08 (12.42) 0.1407 0.8815 82.93 (14.60) 1624.60 (611.81) 52.28 (9.26) 3.27 (1.27) 18.68 (5.37) 1.15 (0.47) 29.03 (8.43) 0.83 (0.45) 7.99 (3.73) 0.23 (0.14) 8.82 (3.67) 0.25 (0.14) 7.08 (3.50) 0.20 (0.13) 180.28 (119.92) 2.33 (2.07) 15.15 (8.63) 77.98 (13.21) 1539.25 (609.13) 51.64 (9.29) 3.15 (1.13) 17.70 (6.18) 1.09 (0.56) 30.69 (8.04) 0.86 (0.41) 7.83 (3.38) 0.22 (0.14) 9.25 (3.53) 0.26 (0.15) 9.14 (4.20) 0.25 (0.15) 169.87 (121.68) 2.19 (1.53) 15.84 (8.67) 0.0004 0.1555 0.4863 0.2773 0.0456 0.1416 0.0418 0.4671 0.6504 0.6317 0.2214 0.3871 0.0000 0.0001 0.4140 0.4437 0.7231 0.1483 0.0000 0.0000 *student’s t-test. Values are mean (SD) or n and %. G1: Group 1 – higher income; G2: Group 2 – lower income; BMI: Body Mass Index; WC: waist circumference; HEI-ad: healthy eating index adapted; SFA: saturated fatty acids; MUFA: monounsaturated fatty acids; PUFA: polyunsaturated fatty acids. Discussion The changes in percentage of energy from dietary fat over the past 30 years in Brazil, as assessed by household food availability (1974-2003), went from 25.8% in 1974/1975 to 30.5% in 2002/2003, representing an increase in 4.7% of fat in the Brazilian diet (Levy-Costa et al., 2005). This increase is consistent with the observed rise in the prevalence of obesity in Brazil (IBGE, 2008). The role of dietary fat in weight gain and obesity has been widely studied in developed countries but remains highly controversial (Lissner & Heitmann, 1995; Willett & Leibel, 2002; Pirozzo et al., 2003) as evidenced from epidemiological studies and long term randomized trials linking fat intake and weight gain or obesity being weak (Willettt & Leibel, 2002; Pirozzo et al., 2003) and inconsistent (Sheppard et al., 1991; Heitmann et al., 1995; Carmichael et al., 1998; Westerterp-Plantenga et al., 1998; Willet & Leibel, 2002). The results of this study suggest that educational level and income may be important determinants of quality of diet but not body fatness. Total fat intake (% energy) was higher among subjects with lower educational level and lower income. This fact could be related to the intake of vegetable oil. Lower income subjects receive monthly food supplies from their employers which consist basically of vegetable oil, salt, sugar, and refined carbohydrates. The oil they receive may be used to cook food and deep fry vegetables or meat/poultry which contributes to the high percentage of fat in the diet. Dietary fat is the most energy-dense nutrient and could lead to over consumption of calories. Increased dietary energy density is associated with obesity (Mendonza et al., 1997). In our study, the amount of fat was related to energy intake. Subjects with higher dietary fat intake had higher energy intake. The higher intake of protein and SFA among subjects with higher educational levels and higher income can be explained by the high consumption of meat (important source of protein and SFA) among these individuals. Protein rich foods (meat, poultry, and milk and dairy products) are more expensive than carbohydrates and vegetable oil, and are consumed more among subjects with higher income. The rapid increase of obesity among the world’s population has become a major public health problem affecting both Cad. Saúde Colet., 2010, Rio de Janeiro, 18 (2): 266-74 269 Katia Cristina Portero-McLellan, Gustavo Duarte Pimentel, Jose Eduardo Corrente, Roberto Carlos Burini developed and developing countries. In Brazil, according to data from the Family Budget Survey (POF 2002-2003), 40.6% of adults were overweight. The increase of obesity occurred in all socioeconomic strata but was notacibly higher in lowincome families (Coitinho, 1991; IBGE, 2008). Several studies have indicated that overweight and obesity are inversely correlated with socioeconomic status in developed countries (Wamala et al., 1997; Lahti-Koski et al., 2002; Liebman et al., 2003) and have shown a negative association between educational level and BMI (Rissanen et al., 1991; Gutiérrez-Fisac et al., 1996; Mokdad et al., 2001). In Brazil, some studies show a positive relationship between income and BMI (Fisberg et al., 2006; Peixoto et al., 2007). Our study failed to show an association between body fatness (BMI and WC) and socioeconomic status (educational level and income) which may indicate that this association depends on the degree of development of the population (Gigante et al., 1997; Martorell et al., 2000; Kruger et al., 2000). WC values were not different between the groups studied but they were higher when compared to subjects from the South of Brazil (Castanheira et al., 2003). The study in the South of Brazil found a linear association of WC and income for both genders but inverse among women, indicating higher risk among men with higher income and women with lower income. The educational levels were inversely related to the central fat only among women (Castanheira et al., 2003). Socioeconomic profile and its relationship with poverty and obesity remain controversial. Monteiro et al., (2001) showed an inverse relationship between obesity and educational levels in Brazilian women in both wealthy and poor part of the country. The study also found a direct relationship with income in the poor area of the country. Our study probably underestimates the effects of dietary fat on body fatness because we used a single 24-hour dietary Table 2 - Obesity, adiposity, and dietary intake distribution between the groups G1 BMI (Kg/m2) <25 25 – 30 ≥30 WC Normal Elevated HEI <70 70 – 100 ≥100 Protein, % energy ≤15 >15 Total fat, % energy ≤30 >30 SFA, % energy <10 ≥10 MUFA, % energy <10 ≥10 PUFA, % energy <10 ≥10 Vegetable Oil, serving <2 ≥2 Fiber, g <20 ≥20 Groups G2 53 (20.0) 115 (40.3) 113 (39.7) 35 (21.5) 66 (40.5) 62 (38.0) 112 (39.3) 173 (60.7) 54 (33.1) 109 (66.9) 57 (20.1) 195 (68.7) 32 (11.2) 41 (25.2) 113 (69.3) 9 (5.5) 70 (24.6) 215 (75.4) 61 (37.4) 102 (62.6) 222 (77.9) 63 (22.1) 111 (68.1) 52 (31.9) 206 (72.3) 79 (27.7) 126 (77.3) 37 (22.7) 200 (72.2) 85 (29.8) 99 (60.7) 64 (39.3) 228 (80.0) 57 (20.0) 107 (65.6) 56 (34.4) 135 (83.3) 27 (16.7) 74 (47.1) 83 (52.9) 215 (75.7) 69 (24.3) 127 (77.9) 36 (22.1) Values are n and %. G1: Group 1 – higher income; G2: Group 2 – lower income; BMI: Body Mass Index; WC: waist circumference; HEI-ad: healthy eating index adapted; SFA: saturated fatty acids; MUFA: monounsaturated fatty acids; PUFA: polyunsaturated fatty acids. Table 3 - Health eating index and food group of the studied groups HEI Bread, cereal, rice, pasta Fruits Vegetables Legumes, beans Milk, dairy Meat, poultry, fish Sugar Oils Variety G1 Mean (SD) / Median 82.9 (14.6) / 84.3 3.5 (1.5) / 3.5 3.4 (3.2) / 2.5 2.4 (2.4) / 1.5 1.2 (1.5) / 1.0 1.7 (1.3) / 1.5 1.8 (1.4) / 1.5 1.7 (2.2) / 1.0 2.4 (2.2) / 2.0 13.7 (3.9) / 13.0 Groups G2 Mean (SD) / Median 78.0 (13.2) / 78.3 3.5 (1.6) / 3.3 1.8 (5.5) / 0.0 1.7 (2.2) / 1.0 2.2 (2.1) / 1.6 1.0 (1.2) / 0.8 1.9 (1.4) / 1.5 1.6 (2.1) / 1.0 2.2 (1.5) / 2.0 10.3 (8.2) / 9.0 *student’s t-test. G1: Group 1 – higher income; G2: Group 2 – lower income; HEI-ad: healthy eating index adapted. 270 Cad. Saúde Colet., 2010, Rio de Janeiro, 18 (2): 266-74 P-value* <0.0001 0.705 0.001 0.003 <0.0001 <0.001 0.957 0.731 0.145 <0.0001 Association of fat intake and socioeconomic status on anthropometric measurements of adults Table 4 - Characteristics and dietary intakes of the subjects according quintiles of total fat (% energy) Age, years Income Education Weight, kg BMI, kg/m2 WC, cm HEI Energy, kcal CHO, % PROT, % FAT, % SFA, % MUFA, % PUFA, % Cholesterol, mg Vegetable oil, serving Fiber, g 1 (lowest) 55.45 (11.04) 2.87 (1.17) 3.63 (2.18) 75.95 (17.16) 28.80 (5.11) 92.93 (16.30) 88.87 (12.95) 1411.88 (445.68) 61.93 (6.87) 19.64 (5.63) 18.41 (2.72) 4.69 (1.83) 5.15 (1.43) 4.47 (1.70) 129.43 (105.62) 1.63 (1.69) 17.28 (10.40) Quintiles of dietary fat intake (% energy) G1 G2 3 5 (highest) 1 (lowest) 3 54.02 (9.86) 48.50 (7.74) 58.35 (11.88) 50.61 (9.20) 2.20 (0.77) 2.38 (0.98) § 1.53 (0.74) 1.80 (0.65) 3.67 (1.93) 2.81 (1.92) 1.20 (0.77) 1.92 (1.38) 76.64 (18.55) 81.31 (20.71) 70.80 (12.90) 74.00 (15.69) 29.71 (6.33) 30.84 (7.36) 29.15 (5.27) 29.42 (6.04) 96.74 (14.96) 99.32 (15.11)§ 95.72 (12.89) 97.20 (12.34) 83.78 (12.47) 73.83 (11.86)* 83.58 (13.94) 81.48 (14.01) 1603.68 (596.68) 1708.63 (702.06) 1293.14 (392.72) 1557.48 (669.47) 51.17 (5.43) 39.88 (6.33)* 63.87 (9.65) 52.70 (5.91) 19.52 (5.16) 17.37 (4.52) 17.89 (8.18) 18.16 (5.73) 29.31 (1.22) 42.71 (5.66)* 18.25 (3.55) 29.14 (1.25) 8.62 (3.19) 11.13 (3.72) 4.45 (2.07) 7.62 (2.16) 9.09 (3.19) 13.36 (3.60)* 4.93 (1.65) 8.62 (2.02) 7.06 (2.76) 10.26 (4.07)* 5.15 (2.08) 8.67 (2.59) 191.65 (124.63) 207.78 (118.71) 139.89 (111.23) 167.01 (116.89) 2.00 (1.14) 3.68 (2.84)* 1.32 (0.72) 2.24 (1.02) 15.55 (8.98) 14.45 (7.53) 13.03 (7.62) 17.21 (10.53) 5 (highest) 54.55 (11.60) 1.64 (0.74) 1.24 (0.99) § 71.84 (14.79) 28.70 (4.88) 96.07 (12.97) 69.62 (9.95)* 1718.76 (690.13) 43.44 (5.73)* 16.20 (5.74) 40.48 (3.39)* 10.53 (3.87) 12.48 (3.27)* 12.45 (4.62)* 223.24 (142.00) 3.09 (1.53)* 13.93 (7.79) § p<0.05; * p<0.001 (chi-square test; ANOVA and Tukey test); G1: Group 1 – higher income; G2: Group 2: lower income; BMI: Body Mass Index; WC: waist circumference; HEI-ad: healthy eating index adapted; SFA: saturated fatty acids; MUFA: monounsaturated fatty acids; PUFA: polyunsaturated fatty acids. Table 5 - Relative risks of BMI>25 and WC>88 (female) and >102 (male) according to the quintiles of oil intake (serving) Quintiles of oil intake (serving) 3 1 2 OR for BMI G1 Crude Model I Model II 1.00 1.00 1.00 1.59 (0.52-4.87) 0.76 (0.13-4.25) 0.84 (0.14-4.83) G2 Crude Model I Model II 1.00 1.00 1.00 OR for WC G1 Crude Model I Model II G2 Crude Model I Model II P-value 4 5 1.80 (0.59-5.44) 1.75 (0.35-8.71) 1.92 (0.37-9.85) 1.23 (0.37-4.09) 0.76 (0.12-4.81) 1.34 (0.19-9.26) 0.86 (0.26-2.84) 0.96 (0.16-5.77) 2.57 (0.32-20.06) 0.50 0.04 0.09 0.85 (0.22-3.20) 0.65 (0.12-3.58) 0.51 (0.08-3.01) 0.26 (0.06-1.13) 0.07 (0.007-0.07) 0.06 (0.006-0.06) 1.14 (0.31-4.12) 0.92 (0.17-4.85) 0.77 (0.13-4.46) 0.97 (0.26-3.57) 0.84 (0.17-4.08) 0.81 (0.14-4.71) 0.22 0.01 0.01 1.00 1.00 1.00 0.82 (0.33-2.04) 0.35 (0.80-1.56) 0.38 (0.08-1.70) 1.81 (0.75-4.38) 1.85 (0.47-7.22) 2.11 (0.53-8.42) 1.23 (0.48-3.15) 0.90 (0.21-3.87) 0.99 (0.21-4.58) 1.04 (0.42-2.56) 0.88 (0.20-3.77) 1.55 (0.28-8.47) 0.26 0.03 0.02 1.00 1.00 1.00 0.85 (0.25-2.85) 0.35 (0.06-1.98) 0.34 (0.06-1.92) 0.47 (0.14-1.52) 0.22 (0.04-1.00) 0.21 (0.04-1.00) 1.08 (0.33-3.52) 0.36 (0.06-2.09) 0.35 (0.06-2.12) 1.08 (0.33-3.52) 0.63 (0.14-2.83) 0.61 (0.12-3.12) 0.46 0.30 0.31 Data are OR (95% IC). Model I: adjusted for age, gender, education and income; Model II: additionally adjusted for energy intake and healthy eating index. recall to obtain dietary data and this type of measurement limits the information about usual dietary intake. It is possible that a stronger relationship between dietary fat intake and body fatness exists with the use of a 7-day weighted intake, but this was not possible in our study. Although the assessment of dietary intake was based on one-day only, this method’s validity for assessing intakes of energy, protein, carbohydrates, and fat has been documented (Conway et al., 2004). Food intake is hard to measure, especially in obese subjects. Goris et al., (2000) observed in their study that 37% Cad. Saúde Colet., 2010, Rio de Janeiro, 18 (2): 266-74 271 Katia Cristina Portero-McLellan, Gustavo Duarte Pimentel, Jose Eduardo Corrente, Roberto Carlos Burini of the obese men studied underreported food intake, mainly energy-dense food with high fat content. The degree of obesity influences the dietary reporting both quantitatively and qualitatively (Heitmann & Lissner, 1995). Subjects with higher education and higher income had a higher intake of energy and protein, and a lower intake of total fat. This data differs from published literature as studies show that total fat intake may increase with higher income (Bonomo et al., 2003). Energy dense foods, often high in refined grains, added sugar, and added fat, are palatable, inexpensive and highly consumed among lower income and less educated populations. These poor quality food supplies are provided by the government. Thus, the inadequate diet lower income individuals consume may be related to the food supplies they receive and the food that they buy. They cannot afford to buy high quality food and the food they receive is not high quality either. On the other hand, while the higher income population could afford good quality food, they also have poor dietary habits as indicated by restaurant/fast food consumption, deep fried meals (fats contribuite to greater flavor and palatability of foods, which could lead to greater consumption of them), consumption of beverages with sugar added, and whole meat habits (barbecue). These behaviors are positively associated with overweight and obesity (Greenwood & Stanford, 2008). McCrory et al., (1999) showed that dietary variety, and the specific food groups that provide it, may be an important determinant of body fatness. A main difference between the foods that were positively associated with increased body fat (sweets, snacks, condiments, entrees and carbohydrates) and foods negatively associated with body fat (vegetables) is their energy density. Our study showed, both in higher and lower income groups, an adequate relative consumption of fat (29.0 and 30.7%, respectively) and a higher intake of protein (18.7 and 17.7%, respectively). Subjects with better education and higher income had higher energy and protein intake, lower SFA, and lower PUFA when compared with the Brazilian national data from the Family Budget Survey (2002-2003). Total fat intake of the subjects studied was similar to the results of the Family Budget Survey (2002-2003). The main difference between the groups studied was total fat intake and PUFA which were higher among subjects with lower educational level and income. Most of the epidemiological studies about dietary intake are based on the analysis of energy intake, macronutrients, and micronutrients (Willett, 2000; Sichieri et al., 2003). Recently the World Health Organization (1998b) suggested that studies should analyze the dietary profile instead of the nutrients. Nutrients and foods are consumed in combination, and their effects can be observed only when the entire eating pattern is considered. Dietary patterns may suggest a more comprehensive approach to disease prevention or treatment because the focus is on the entire diet and not just one food or an isolated nutrient (Fung et al., 2001). Conclusion Besides differences in socioeconomic status, educational level and (deficient) HEI the groups were similar by presenting high BMI and abdominal fatness. Only differences in fat profile were correlated with the anthropometric measures mostly explained by the lower vegetable oil intake in higher income participants. References Bonomo, E. et al. Consumo alimentar da população adulta segundo perfil socio-econômico e demográfico: Projeto Bambui. Cadernos de Saúde Pública, v. 19, p. 1461-1471, 2003. Carmichael, H. E.; Swinburn, B. A.; Wilson, W. R. Lower fat intake as a predictor of inicial and sustaind weight loss in obese subjects consuming an otherwise ad libitum diet. Journal of the American Dietetic Association, v. 98, p. 35-39, 1998. Castanheira, M.; Olinto, M. T. A.; Gigante, D. P. Associação de variáveis socio-demográficas e comportamentais com a gordura abdominal em adultos: estudo de base populacional no Sul do Brasil. Cadernos de Saúde Pública, v. 19 (sup. 1), p. S55-S65, 2003. 272 Cad. Saúde Colet., 2010, Rio de Janeiro, 18 (2): 266-74 Chor, D.; Faerstein, E.; Alves, M.G.M.; Lopes, C. S. How reproducible is self-reported information on exposure to smoking, drinking, and dietary patterns? Evidence among Brazilian adults in the Pro-Saude Study. São Paulo Medical Journal, v. 121, p. 63-66, 2003. Coitinho, D. C.; Leão, M. M.; Recine, E.; Sichieri, R. Condições nutricionais da população brasileira: adultos e idosos. Brasília: Instituto Nacional de Alimentação e Nutrição, 1991. Conway, J. M.; Ingwersen, L. A.; Moshfegh, A. J. Accuracy of dietary recall using the USDA five step multiple-pass method in men: an observational validation study. Journal of the American Dietetic Association, v. 104, p. 595603, 2004. Association of fat intake and socioeconomic status on anthropometric measurements of adults Fisberg, R. M. et al. Dietary quality and associated factors among adults living in the state of São Paulo, Brazil. Journal of the American Dietetic Association, v. 106, n. 12, p. 2067-2072, 2006. Liebman, M. et al. Dietary intake, eating behavior and physical activity-related determinants of high body mass index in rural communities in Wyoming, and Idaho. International Journal of Obesity, v. 27, p. 684-692, 2003. Fornes, N. S. et al. Food frequency consumption and lipoproteins serum levels in the population of an urban area, Brazil. Revista de Saúde Pública, v. 34, p. 380-387, 2000. Lissner, L.; Heitmann, B. L. Dietary fat and obesity: evidence from epidemiology. European Journal of Clinical Nutrition, v. 49, p. 79-90, 1995. Fornes, N. S.; Martins, I. S.; Velasquez-Melendez, G.; Latorre, M. R. D. Escores de consumo alimentar e níveis lipêmicos em população de São Paulo, Brasil. Revista de Saúde Pública, v. 36, p. 12-18, 2002. Fung, T. T. et al. Association between dietary patterns and plasma biomarkers of obesity and cardiovascular disease risk. The American Journal of Clinical Nutrition, v. 73, p. 61-77, 2001. Gigante, D. P.; Barros, F. C.; Post, C. L. A.; Olinto, M. T. A. Prevalência de obesidade em adultos e seus fatores de risco. Revista de Saúde Pública, v. 31, p. 236-246, 1997. Goris, A. H. C.; Westerterp-Plantenga, M. S.; Westerterp, K. R. Underrecording of habitual food intake in obese men: selective underreporting of fat intake. The American Journal of Clinical Nutrition, v. 71, p. 130-134,2000. Greenwood, J. L. J.; Stanford, J. B. Preventing or improving obesity by addressing specific eating patterns. Journal of the American Board of Family Medicine, v. 21, p. 135-140, 2008. Gutiérrez-Fisac, J. L.; Regidos, E.; Rodríguez, C. Trends in obesity differences by educational level in Spain. Journal of Clinical Epidemiology, v. 49, p. 351-354, 1996. Heitmann, B. L.; Lissner, L. Dietary underreporting by obese individuals – is it specific or non-specific? British Journal of Medicine, v. 311, p. 986-989, 1995. Heitmann, B. L.; Lissner, L.; Sorensen, T. I.; Bengtsson, C. Dietary fat intake and weight gain in women genetically predisposed for obesity. The American Journal of Clinical Nutrition, v. 61, p. 1213-1217, 1995. Instituto Brasileiro de Geografia e Estatística (IBGE). Estimativas da população residente em municípios brasileiros. Ministério do Planejamento, Orçamento e Estatística, 2006 Aacesso em: 12 junho 2008. Disponível em: http://www.ibge.gov.br/home/estatistica/populacao/estimativa2006/ estimativa.shtm. ______. Pesquisa de Orçamentos Familiares, 2002-2003. Excesso de peso atinge 38.8 milhões de brasileiros adultos. Acesso em 16 de junho de 2008. Disponível em: http://www.ibge.gov.br/home/estatistica/populacao/ condicaodevida/pof/2002/default.shtm ______. Tabela de composição de alimentos. 5. ed. Rio de Janeiro; 1999. Kennedy, E. T.; Ohls, J.; Carlson, S.; Fleming, K. The Healthy Eating Index: design and applications. Journal of the American Dietetic Association, v. 95, p. 1103-1108, 1995. Kruger, H. S.; Venter, C. S.; Voster, H. H.; Margetts, B. M. Physical inactivity is the major determinant of obesity in black women in the North West Province, South Africa: the THUSA study. Transition and Health During Urbanisation of South Africa. Nutrition, v. 18, p. 422-427, 2002. Lahti-Koski, M.; Pietnen, P.; Heliovaara, M.; Vartiainen, E. Associations of body mass index and obesity with physical activity, food choices, alcohol intake, and smoking in the 1982-1997 FINRISK Studies. The American Journal of Clinical Nutrition, v. 75, p. 809-817, 2002. Levy-Costa, R. B.; Sichieri, R.; Pontes, N. S.; Monteiro, C. A. Disponibilidade domiciliar de alimentos no Brasil: distribuição e evolução (1974-2003). Revista de Saúde Pública, v. 39, p. 530-540, 2005. Martorell, R.; Khan, L. K.; Hughes, M. L.; Grummer-Strawn, L. M. Obesity in women from developing countries. European Journal of Clinical Nutrition, v. 54, p. 247-252, 2000. McCrory, M. A. et al. Dietary variety within food groups: associations with energy intake and bocy fatness in men and women. The American Journal of Clinical Nutrition, v. 69, p. 440-447, 1999. Mendoza, J. A.; Drewnowski, A.; Christakis, D. A. Dietary energy density is associated with obesity and the metabolic syndrome in U. S. adults. Diabetes Care, v. 30, n. 4, p. 974-979, 2007. Mokdad, A. et al. The continuing epidemics of obesity and diabetes in the United States. JAMA: The Journal of the American Medical Association, v. 286, p. 1195-1200, 2001. Molina, M. C. et al. Food consumption by yong adults living in Ribeirao Preto, SP, 2002/2004. Brazilian Journal of Medical and Biological Research, v. 40, p. 1257-1266, 2007. Mondini, L.; Monteiro, C. A. Changes in the diet pattern of the Brazilian urban population (1962-1988). Revista de Saúde Pública, v. 28, p .433-439, 1994. Monteiro, C. A.; Mondini, L.; Souza, A. L.; Popkin, B. M. The nutrition transition in Brazil. European Journal of Clinical Nutrition, v. 49, p. 105-113, 1995. Monteiro, C. A.; Conde, W. L.; Popkin, B. M. Independent effects of income and educational on the risk of obesity in the Brazilian adult population. Journal of Nutrition, v. 131 (suppl), p. S881-S886, 2001. Monteiro, C. A.; Mondini, L.; Costa, R. B. Changes in composition and appropriate nutrition of family diet in the metropolitan areas of Brazil (19881996). Revista de Saúde Pública, v. 34, p. 251-258, 2000. Mota, J. F. et al. Adaptação do índice de alimentação saudável ao guia alimentar da população brasileira. Revista de Nutrição, v. 21, p. 545-552, 2008. Núcleo de Pesquisas em Alimentação da Universidade Estadual de Campinas (Nepa/Unicamp). Tabela brasileira de composição de alimentos. Taco. Versão 1. Campinas; 2004. Neumann, A. I. C. P.; Martins, I. S.; Marcopito, L. F.; Araujo, E. A. C. Padrões alimentares associados a fatores de risco para doenças cardiovasculares entre residentes de um município brasileiro. Revista Panamericana de Salud Pública, v. 22, p. 329-339, 2007. NutWin. Programa de apoio à nutrição. Departamento de Informática em Saúde – DIS – Universidade Federal de São Paulo – Unifesp/EPM, versão 1.5, 2002. Peixoto, Mdo R.; Benicio, M. H.; Jardim, P. C. The relationship between body mass index and lifestyle in a Brazilian adult population: a cross-sectional survey. Cadernos de Saúde Pública, v. 23, p. 2694-2740, 2007. Philippi, S. T. Tabela de composição de alimentos: suporte para decisão nutricional. 2ª ed. São Paulo; 2002. Philippi, S. T.; Latterza, A. R.; Cruz, A. T. R.; Ribeiro, L. C. Adapted food pyramid: a guide for a right food choice. Revista de Nutrição, v. 12, p. 65-80, 1999. Cad. Saúde Colet., 2010, Rio de Janeiro, 18 (2): 266-74 273 Katia Cristina Portero-McLellan, Gustavo Duarte Pimentel, Jose Eduardo Corrente, Roberto Carlos Burini Pirozzo, S.; Summerbell, C.; Cameron, C.; Glasziou, P. Should we recommend low-fat diets for obesity? Obesity Reviews, v. 4, p. 83-90, 2003. Popkin, B. M. The shift in stages of the nutrition transition in the developing world differs from past experiences! Public Health of Nutrition, v. 2, p. 205214, 2002. Rissanen, A. M. et al. Determinants of weight gain and overweight in adult Finns. European Journal of Clinical Nutrition, v. 45, p. 419-430, 1991. Salvo, V. L. M. A.; Gimeno, S. G. A. Reprodutibilidade e validade do questionário de frequência de consumo de alimentos. Revista de Saúde Pública, v. 36, p. 505-512, 2002. Sheppard, L.; Kristal, A. R.; Kushi, L. H. Weight loss in women participating in a randomized trial of low-fat diets. The American Journal of Clinical Nutrition, v. 54, p. 821-828, 1991. Sichieri, R.; Castro, J. F. G.; Moura, A. S. Fatores associados ao padrão de consumo alimentar da população brasileira urbana. Cadernos de Saúde Pública, v. 19 (sup. 1), p. S47-S53, 2003. Wamala, S. P.; Wolk, A.; Orth-Gomér, K. Determinants of obesity in relation to socioeconomic status among middle-aged Swedish women. Preventive Medicine, v. 26, p. 734-744, 1997. 274 Cad. Saúde Colet., 2010, Rio de Janeiro, 18 (2): 266-74 Westerterp-Plantenga, M. S. et al. Energy intake and body weight effects of six months reduced or full fat diets, as a function of dietary restraint. International Journal of Obesity and Related Metabolic Disorders, v. 22, p. 1422, 1998. Willett, W. C. Nutritional epidemiology issues in chronic disease at the turn of the century. Epidemiologic reviews, v. 22, p. 82-86, 2000. Willett, W. C.; Howe, G. R.; Kushi, L. H. Adjustment for total energy intake in epidemiologica studies. The American Journal of Clinical Nutrition, v. 65 (supl l), p. S1220-S1228, 1997. Willett, W. C.; Leibel, R. L. Dietary fat is not a major determinant of body fat. American Journal of Medicine, v. 113 (suppl 9B), p. 47S-59S, 2002. World Health Organization (WHO). Obesity: Preventing and managing the global epidemic. Report of a WHO Consultation on Obesity. Geneva: WHO; 1998a. ______. Report of a Joint FAO/WHO Consultation. Preparation of food-based dietary guidelines. Geneva: WHO; 1998b. Recebido em: 07/5/2009 Aceito em: 13/4/2010
Baixar