EPIDEMIOLOGIA E ONCOLOGIA: UMA
RELAÇÃO ÍNTIMA
Moysés Szklo
Professor de Epidemiologia e Medicina
Universidade Johns Hopkins
Editor-Chefe, American Journal of Epidemiology
Things have to be as
simple as possible, but
not simpler.
(Einstein)
Conceito Fundamental Para o Controle de Câncer: História Natural
Início da
exposição a
fatores de
risco
Início da
enfermidade
Detecção
precoce (se
possível),
Detecção
baseada em
sintomas ou
sinais que
ocorrem no
início da
fase clínica,
“Tempo de antecipação”
(Baseado em Gordis L. Epidemiology, 3rd
edition)
Detecção
baseada em
sintomas e
sinais, que
ocorre com
atraso depois do
início da fase
Morte,
clínica
cura ou
recidiva
As áreas de pesquisa em câncer
se “encaixam” na história natural
Início da
exposição a
fatores de
risco
Início da
enfermidade
Detecção
precoce (se
possível),
Detecção
baseada em
sintomas ou
sinais que
ocorrem no
início da
fase clínica,
Detecção
baseada em
sintomas e
sinais, que
ocorre com
atraso depois do
início da fase
Morte,
clínica
cura ou
recidiva
“Tempo de antecipação”
Estudos de avaliação de
programas de detecção
precoce (rastreamento/
prevenção secundária)
Estudos de
fatores
determinantes
de atraso
diagnóstico
Avaliação de
programas de
atenção a
pacientes
terminais
Estudos de fatores prognósticos biológicos, ambientais e
terapêuticos
Estudos de qualidade de vida
Estudos de processo e estrutura do sistema de atenção à saúde
Correspondência entre as diferentes fases da história natural do
câncer e níveis de controle
Início da
exposição a
fatores de
risco
Início da
enfermidade
Detecção
precoce (se
possível),
Detecção
baseada em
sintomas ou
sinais que
ocorrem no
início da
fase clínica,
Detecção
baseada em
sintomas e
sinais, que
ocorre com
atraso depois do
início da fase
Morte,
clínica
cura ou
recidiva
“Tempo de antecipação”
Prevenção primária:
• Prevenção de exposição
a fatores de risco
• Cessação de exposição
Prevenção
secundária
(rastreamento)
Prevenção terciária
Estudos epidemiológicos
• Estudos experimentais (ensaios clinicos) e estudos observacionais
Correspondência entre as diferentes fases da história natural do
câncer e níveis de controle
Início da
exposição a
fatores de
risco
Início “da
enfermidade
Detecção
precoce (se
possível),
Detecção
baseada em
sintomas ou
sinais que
ocorrem no
início da
fase clínica,
Detecção
baseada em
sintomas e
sinais, que
ocorre com
atraso depois do
início da fase
Morte,
clínica
cura ou
recidiva
“Tempo de antecipação”
Prevenção primária:
• Prevenção de exposição
a fatores de risco
• Cessação de exposição
Prevenção
Preven
ção
secundá
secund
ária
Prevenção
Preven
ção terci
terciá
ária
O GRANDE SUCESSO DA PREVENÇÃO PRIMÁRIA
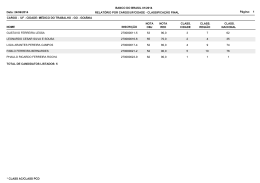
Prevalência de tabagismo entre adultos de 18 anos ou mais de idade e
estratégias nacionais de controle de tabaco implementadas entre 1986 e 2008
(Adaptado de Figueiredo VC [Tese de Doutorado]. RJ: Instituto de Medicina Social, UERJ, 2007)
Primary Prevention of Cancer Is Based on the Epidemiologic Triad of
Risk Factors
Environment
Vector
Human
host
Agent
Primary Prevention of Cancer Is Based on the Epidemiologic Triad of
Risk Factors
Three basic strategies in
primary prevention
Environment
Vector
Human
host
- Kill the agent and/or the
vector
- Make the environment hostile
to the agent
- Increase human host’s
resistance
Agent
Primary Prevention of Cancer Is Based on the Epidemiologic Triad of
Risk Factors – Example: Tobacco Exposure
Environment:
air
Example: Prohibition of indoor
smoking
Example: lobby
against tobacco
industry
Example:
Decrease in
tobacco
cultivation
Vector: tobacco
industry
Agent: tobacco
Human
Host: behavior
Example: Health education,
smoking cessation therapy
Risk Factors (Causes) for Cancer Established by Epidemiologic
Research: Some Examples
•
Estrogen replacement therapy and breast and endometrial cancers
•
Asbestos and respiratory cancer
•
Smoking and cancers
•
Ionizing radiation and cancers
•
Down’s syndrome and leukemia
•
Helicobacter pylori and gastric cancer
•
HPV and cervical cancer
•
Obesity and post-menopausal breast cancer
•
Diet low in fibers and colon cancer
COMO SÃO GERADAS AS HIPÓTESES SOBRE FATORES DE
RISCO (ETIOLOGIA) DE CÂNCER?
Epidemiologia é a arte de
olhar
A melhor estratégia de
análise de dados é olhar
os dados e pensar no que
se está vendo.
(G. W. Comstock)
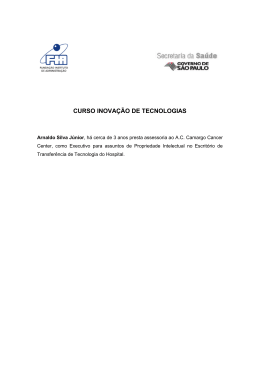
Generating Hypothesis from Descriptive (Available) Population Data: Average
Annual Breast Cancer Age-specific Incidence Rates per 100,000, USA 19972001 (based on SEER data)
100
Incidence Rates/ 100,000
90
80
70
60
3-D Column 1
3-D Column 2
3-D Column 3
50
40
30
20
10
0
Age
30-34
50-54
75+
The decrease in the slope at around menopause led to the hypothesis that breast
cancer is estrogen-dependent, which was subsequently confirmed in analytic
epidemiologic studies
O MODELO DE ROTHMAN EXPLICA DOIS
FENÔMENOS RELACIONADOS
-POPULAÇÕES COM PREVALÊNCIA ELEVADA DE
UM COMPONENTE CAUSAL OU UMA CAUSA
NECESSÁRIA (FATOR DE RISCO) TÊM RISCO
BAIXO DA ENFERMIDADE FALTAM
COMPONENTES CAUSAIS QUE COMPLETEM AS
CAUSAS SUFICIENTES;
- ELIMINAÇÃO DE UM FATOR DE RISCO
(COMPONENTE CAUSAL) DIMINUI O RISCO DA
ENFERMIDADE TODOS AS CAUSAS
SUFICIENTES QUE CONTÊM O COMPONENTE
CAUSAL SÃO ELIMINADAS
Modelo de causalidade de
Rothman
High Salt
Intake
High
intake of
processed
foods
Smoking
H. Pylori
Taxas por 100 000
Causa suficiente
Constelação de
componentes causais
que, quando presente,
causa inevitavelmente a
doença
Causa necessária,
mas não suficiente
High Salt
Intake
Taxas de mortalidade por câncer, ajustadas por idade, sexo feminino, Estados
Unidos 1930-2001
Smoking
(American Cancer Society, 2005)
(American Cancer Society, 2005)
High
intake of
processed
foods
H.
Pylori*
O MODELO DE ROTHMAN EXPLICA DOIS
FENÔMENOS RELACIONADOS
-POPULAÇÕES COM PREVALÊNCIA ELEVADA DE
UM COMPONENTE CAUSAL OU UMA CAUSA
NECESSÁRIA (FATOR DE RISCO) TÊM RISCO
BAIXO DA ENFERMIDADE FALTAM
COMPONENTES CAUSAIS QUE COMPLETEM AS
CAUSAS SUFICIENTES;
- ELIMINAÇÃO DE UM FATOR DE RISCO
(COMPONENTE CAUSAL) DIMINUI O RISCO DA
ENFERMIDADE TODOS AS CAUSAS
SUFICIENTES QUE CONTÊM O COMPONENTE
CAUSAL SÃO ELIMINADAS
Modelo de causalidade de
Rothman
High Salt
Intake
High
intake of
processed
foods
Smoking
H. Pylori
Taxas por 100 000
Causa suficiente
Constelação de
componentes causais
que, quando presente,
causa inevitavelmente a
doença
Causa necessária,
mas não suficiente
High Salt
Intake
Taxas de mortalidade por câncer, ajustadas por idade, sexo feminino, Estados
Unidos 1930-2001
Smoking
(American Cancer Society, 2005)
(American Cancer Society, 2005)
High
intake of
processed
foods
H.
Pylori*
Correspondência entre as diferentes fases da história natural do
câncer e níveis de controle
Início da
exposição a
fatores de
risco
Momento em que
a detecção
precoce se torna
possivel
Início da
enfermidade
Detecção
precoce é
feita,
Detecção
baseada em
sintomas ou
sinais que
ocorrem no
início da
fase clínica,
Detecção
baseada em
sintomas e
sinais, que
ocorre com
atraso depois do
início da fase
Morte,
clínica
cura ou
recidiva
Tempo de antecipação
Fase pré-clínica detectável (FPCD)
Prevenção primária:
• Prevenção da exposição
a fatores de risco
• Cessação de exposição
Prevenção
secundária
(rastreamento)
Prevenção
Preven
ção terci
terciá
ária
Correspondência entre as diferentes fases da história natural do
câncer e níveis de controle
Início da
exposição a
fatores de
risco
Momento em que
a detecção
precoce se torna
possivel
Detecção
baseada em
sintomas ou
sinais que
ocorrem no
início da
fase clínica,
Início da
enfermidade
Detecção
baseada em
sintomas e
sinais, que
ocorre com
atraso depois do
início da fase
Morte,
clínica
cura ou
recidiva
“Tempo de antecipação”
Fase pré-clínica detectável (FPCD)
Prevenção primária:
• Prevenção da exposição
a fatores de risco
• Cessação de exposição
Prevenção
secundária
(rastreamento)
Prevenção
Preven
ção terci
terciá
ária
Correspondência entre as diferentes fases da história natural do
câncer e níveis de controle
Início da
exposição a
fatores de
risco
Momento em que
a detecção
precoce se torna
possivel
Detecção
baseada em
sintomas ou
sinais que
ocorrem no
início da
fase clínica,
Início da
enfermidade
Detecção
baseada em
sintomas e
sinais, que
ocorre com
atraso depois do
início da fase
Morte,
clínica
cura ou
recidiva
“Tempo de antecipação”
Fase pré-clínica detectável (FPCD)
Prevenção primária:
• Prevenção da exposição
a fatores de risco
• Cessação de exposição
Prevenção
secundária
(rastreamento)
Prevenção
Preven
ção terci
terciá
ária
ANOTHER CRITICAL CONCEPT IN CANCER
CONTROL: THE CRITICAL POINT
Critical Point: A point in the natural history of the disease
before which therapy may be less difficult and/or more
effective (If this disease is potentially curable, cure may be
possible before this point, but not after)
(Baseado em Gordis L. Epidemiology, 3rd
edition)
Biologic
onset
A
Earliest
point when
diagnosis is
possible
Usual
diagnosis
based on
symptoms
Effective early diagnosis
B
D
Detectable Preclinical
Phase
Critical point
When should early
diagnosis be made?
NATURAL HISTORY OF A DISEASE
(Adapted from Gordis,
Epidemiology, 1996)
Biologic
onset
A
Earliest
point when
diagnosis is
possible
Usual
diagnosis
based on
symptoms
B
D
Detectable Preclinical
Phase
Critical point
When should early
diagnosis be made?
NATURAL HISTORY OF A DISEASE
(Adapted from Gordis,
Epidemiology, 1996)
Biologic
onset
A
Earliest
point when
diagnosis is
possible
Usual
diagnosis
based on
symptoms
B
D
Detectable Preclinical
Phase
Critical point
When should early
diagnosis be made?
NOT NECESSARY!
NATURAL HISTORY OF A DISEASE
(Adapted from Gordis,
Epidemiology, 1996)
Earliest
point when
diagnosis is
Biologic possible
onset
A
Usual
diagnosis
based on
symptoms
Effective early diagnosis
B
D
Detectable Preclinical
Phase
Critical point
IN CERVICAL CANCER, THE DPCP PRIOR TO
THE CRITICAL POINT IS LONG: SCREENING
EVERY 3 YEARS IS FAIRLY CONSERVATIVE
NATURAL HISTORY OF A DISEASE
(Adapted from Gordis,
Epidemiology, 1996)
Earliest
point when
diagnosis is
Biologic possible
onset
Effective early diagnosis
A
B
Usual
diagnosis
based on
symptoms
D
Detectable Preclinical
Phase
IN BREAST CANCER, THE DPCP PRIOR TO THE
CRITICAL POINT IS RELATIVELY SHORT:
SCREENING EVERY TWO YEARS IS
REASONABLE (DPCP ∼3.3 years for postmenopausal women; ∼1.7 years for <50 years old)
(Tabar,HISTORY
et al, Cancer
Tabar et al, Int
NATURAL
OF A1995;75:2507-17;
DISEASE
J Cancer 1996;66:413-9)
(Adapted from Gordis,
Critical point
Epidemiology, 1996)
Usual
diagnosis
based on
symptoms
Earliest
point when
diagnosis is
Biologic possible
onset
A
B
D
Detectable Preclinical
Phase
Critical point
IN LUNG CANCER, THE DPCP PRIOR TO THE
CRITICAL POINT IS SO SHORT THAT
SCREENING IS NOT EFFECTIVE
NATURAL HISTORY OF A DISEASE
(Adapted from Gordis,
Epidemiology, 1996)
Biologic
onset
A
Usual
diagnosis
based on
symptoms
Earliest
point when
diagnosis is
possible
Survival* Survival* Screening is
2 yrs
5 yrs
ineffective
cure
B
1
2
3
D
Detectable Preclinical
Phase
*corrected for lead time
Critical point
Most diseases have multiple critical
points; thus, the earlier the
diagnosis, the better the prognosis
NATURAL HISTORY OF A DISEASE
(Adapted from Gordis,
Epidemiology, 1996)
A KEY NOTION WHEN EVALUATING SURVIVAL OF PATIENTS WITH
CANCER: LEAD TIME BIAS
NATURAL HISTORY OF CANCER IN PATIENTS A AND B IS THE SAME
Patient
A
Disease
onset
Diagnosis based
on symptoms
Death
1995
2004
2010
Survival= 6 years
Patient
B
Lead time
Disease
onset
Early diagnosis
Death
1995
2002
2010
Survival= 8 years
Survival B = Survival A + lead time
Conclusion: Screening was not effective
A KEY NOTION WHEN EVALUATING SURVIVAL OF PATIENTS WITH
CANCER: LEAD TIME BIAS
NATURAL HISTORY OF CANCER IN PATIENTS A AND B IS DIFFERENT
Patient
A
Disease
onset
Diagnosis based
on symptoms
Death
1995
2004
2010
Survival= 6 years
Patient
B
Net gain
Lead time
Disease
onset
Early diagnosis
Death
1995
2002
2010
Survival= 10 years
Survival B > Survival A + lead time
Conclusion: Screening was effective
2012
Natural History of a
Disease: Lead Time Bias in Survival Analysis
(Adapted from Frank, Am J Prev
1985;1:3-9)
Cumulative Survival
100%
70%
Lead time
bias
40%
Lead Time
-2
Usual diagnosis
Early
diagnosis
3
5
10
12
5 years after usual diagnosis
5 years after early diagnosis
(Baseado em Gordis L. Epidemiology, 3rd
edition)
Lead-Time- Adjusted Five-Year Survival Among Breast Cancer Patients in
Shapiro et al’s Randomized Clinical Trial
(Shapiro et al, JNCI 1982;69:349-55)
80
70
60
50
40
30
20
10
0
Control
2nd Qtr
Total
Allocated to
Screening
Overdiagnosis Bias: Bleyer AB & Welch HG. Effect of Three Decades of
Screening Mammography on Breast Cancer Incidence. New Eng J Med
2012;367:1998-2005.
•
Effective cancer screening should increase the incidence of disease
detected at an early stage and decrease late stage disease
•
Examination of breast cancer incidence trends from 1976 through 2008,
taking into account the transient excess incidence associated with hormone
replacement therapy and adjusting for trends in the incidence of women
younger than 40 years (that is, women without screening)
•
During this period, incidence of early stage breast cancer doubled (an
absolute increase of 122 cases per 100 000 women)
•
The rate of late stage breast cancer decreased by 8% (from 102 to 94
cases per 100 000 women), corresponding to 8 cases.
•
Thus, only 8 of the 122 cases were thus expected to progress to advanced
disease
•
It is estimated that in 2008 breast cancer was overdiagnosed in more than
70 000 women (31% of all breast cancers diagnosed)
Assumptions Justifying a Screening Program
• All or most clinical cases of a disease first go through a detectable
pre-clinical phase prior to the last critical point, and
• In the absence of intervention, all or most cases in a pre-clinical
phase progress to the clinical phase.
• Prognosis (recurrence free survival and survival) improve with early
diagnosis
Causas de baixa efetividade de um programa de rastreamento
Início da
exposição a
fatores de
risco
Início da
enfermidade
Detecção
precoce (se
possível),
Detecção
baseada em
sintomas ou
sinais que
ocorrem no
início da
fase clínica,
Detecção
baseada em
sintomas e
sinais, que
ocorre com
atraso depois do
início da fase
Morte,
clínica
cura ou
recidiva
“Tempo de antecipação”
• Tempo de antecipação é curto (ex: câncer de pulmão)
• O tempo de antecipação é longo, mas a terapia não é eficaz
• A terapia é eficaz, mas o sistema de atenção à saúde é falho
Correspondência entre as diferentes fases da história natural do
câncer e níveis de controle
Início da
exposição a
fatores de
risco
Momento em que
a detecção
precoce se torna
possivel
Início da
enfermidade
Detecção
precoce é
feita,
Detecção
baseada em
sintomas ou
sinais que
ocorrem no
início da
fase clínica,
Detecção
baseada em
sintomas e
sinais, que
ocorre com
atraso depois do
início da fase
Morte,
clínica
cura ou
recidiva
“Tempo de antecipação”
Fase pré-clínica detectável (FPCD)
Prevenção primária
primária::
• Prevenção da exposição
a fatores de risco
• Cessação de exposição
Prevenção
secundária::
secundária
rastreamento
Prevenção
Preven
ção terci
terciá
ária
Designs Used in Clinical Research (Clinical Epidemiology)
EXPERIMENTAL (RANDOMIZED
CLINICAL TRIAL)
Study Sample
Random Allocation
Intervention
Control
Follow-up
Outcome
Efficacy =
Outcome
( Incidence in Control Group ) − ( Incidence in Active Intervention Group )
× 100
( Incidence in Control Group )
Experimental Epidemiology: the Randomized Clinical Trial
Randomized Clinical Trials of Screening for Prostate Cancer
Cumulative mortality. Schroder FH, et al. New Eng
J Med 2009;360:1320-8 (USA)
Cumulative number of deaths.
Andriole GL et al, New Eng J
Med 2009;360:1310-9 (Europe)
Randomized Clinical Trial: Recurrence and Breast Cancer
Mortality in 6846 Women with ER-positive Disease
Recurrence
Mortality
(Davies C, Pan H, Godwin J, et al. Long term effects of continuing adjuvant tamoxifen to 10 years versus stopping at 5 years after diagnosis of oestrogen
receptor-positive breast cancer:ATLAS, a randomised trial. Lancet 2012 [Electronic publication])
Two Designs Used in Clinical Research
(Clinical Epidemiology)
EXPERIMENTAL (RANDOMIZED
CLINICAL TRIAL)
NON-EXPERIMENTAL
(OBSERVATIONAL)
Study Sample
Study Sample
Random Allocation
Non-Random Allocation
Intervention
Control
Follow-up
Outcome
Outcome
Factor (+)
Factor (-)
Follow-up
Outcome
Outcome
Observational Study: Kaplan-Meier curves of survival after diagnosis of breast cancer.
HER2 human epidermal growth factor receptor-2-positive; HR hormone receptor
(estrogen and/or progesterone); TN triple negative (estrogen, progesterone and HER2
negative)
Stearoyl-CoA
desaturase 1
(SCD1): essential
regulator of fatty
acid synthesis.
Overexpression
increases the
growth of breast
cancer cell line.
All
HR+
TN
HER2+
(Holder AM, Gonzalez-Angulo AM, Chen H, et al. High stearoyl-CoA desaturase 1 expression is associated with shorter survival in breast cancer patients. Breast
Cancer Res Treat [epubl, Dec 2012])
Detour: A USEFUL STATISTIC: THE NUMBER OF
PEOPLE WHO HAVE TO BE TREATED TO PREVENT
ONE EVENT
How is the number that needs to be screened/treated to prevent one
death calculated?
It is the inverse of the difference in mortality between the control and the active intervention
groups. For example, if the mortality rate in the control group is 30% and in the active
intervention group it is 10%, the difference is 20% Thus, if for every 100 individuals, 20
deaths are prevented, to prevent 1 death, 1/0.2= 5.
FOR EVERY 100 TREATED/SCREENED PERSONS
20 DEATHS ARE AVOIDED
1 AVOIDED DEATH
x?
X= (100 × 1) ÷ 20= 5
Some Key Objectives of Epidemiology
(All Relevant to Cancer Control)
• Investigate the etiology (risk factors) of disease;
• Assess effectiveness of preventive and curative strategies;
• Translate epidemiologic findings into public health policies.
Some Key Objectives of Epidemiology
(All Relevant to Cancer Control)
• Investigate the etiology (risk factors) of disease;
• Assess effectiveness of preventive and curative strategies;
• Translate epidemiologic findings into public health policies.
TRANSLATIONAL EPIDEMIOLOGY
Processo de Implementação de Politicas de Controle do Câncer Baseadas em
Evidências
Políticas baseadas em
evidências
Aquisição de evidências
científicas
• Ensaios
aleatorizados
• Estudos de coorte
• Estudos de casos e
controles
• Estudos de séries
temporais
• Estudos de
processo e estrutura
• Estudos
conduzidos de
novo
(Modificado de Dickersin K)
Revisões
sistemáticas
• Colaboração
Cochrane
• Outras fontes
(meta-análises
publicadas em
revistas)
• Revisões
Sistemáticas e
meta-análises
realizadas de
novo
Custoefetividade
Análise de
sensibilidade
Aplicação da politica:
planejamento
• Evidências
• Obstáculos
• Avaliação de níveis
de evidência
• Seleção de opções
programáticas
(análise de decisão)
• Recomendações
Tradução de conhecimentos
Levels of Evidence on Effectiveness
better
• Meta-analysis of randomized trials
• Individual randomized trial of high quality
• Dramatic changes in the incidence/mortality after
introduction of a given program (e.g., St Jude protocol and
survival of acute lymphocytic leukemia in children)
• Meta-analysis of cohort studies
• Individual cohort study of high quality
• Meta-analysis of case-control studies
• Individual case-control study of high quality
worse
• Expert opinion not based on the above
Forest plot of the effect of group counselling on the incidence of smoking abstinence. Use of nicotine patch, bupropion, and
notriptyline varied among studies (Motillo S, et al. Eur Heart J 2008 [Epub ahead of print Dec 24]
Interface between epidemiology and the
decision-making process
• Meta-Analysis
Evaluation of effectiveness
• Decision Analysis
• Cost-Effectiveness Analysis
(Pettiti DB. Meta-Analysis, Decision Analysis and Cost-Effectiveness Analysis. New
York, Oxford, Oxford University Press, 1994)
Interface between epidemiology and the
decision-making process
• Meta-Analysis
Evaluation of effectiveness
• Decision Analysis
• Cost-Effectiveness Analysis
(Pettiti DB. Meta-Analysis, Decision Analysis and Cost-Effectiveness Analysis. New
York, Oxford, Oxford University Press, 1994
Relations between meta-analysis, decision analysis and costeffectiveness analysis
Decision Analysis
Meta-Analysis
Summary of the
efficacy/effectiveness of the
intervention
Assessment of the relative value of the
programmatic options, based on their
community effectiveness (ideally determined
by meta-analysis)
Cost-effectiveness Analysis
Assessment of the cost of the program, based on the relative value
of the options
Decision Analysis: uses a quantitative approach to
evaluate the relative value (effectiveness) of one or more
interventions, programs or services.
Steps in Decision Analysis
• Identification and description of the problem
• Collection of the information needed to construct the
decision tree (ideally by means of meta-analysis)
• Construction of a decision tree
• Analysis of the decision tree
High Social Class (0.10)
Mortality (0.10)
Yes
(0.70)
SC
Mortality(0.20)
Tolerance
to
intervention
Low Social Class (0.90)
High Social Class (0.10)
No
(0.30)
Mortality (0.50)
SC
Mortality (0.50)
Decision Node
Low Social Class (0.90)
High Social Class (0.10)
Mortality (0.05)
Yes
(0.30)
SC
Mortality (0.10)
Low Social Class (0.90)
Tolerance
to
intervention
No
(0.70)
High Social Class (0.10)
Mortality (0.50)
SC
Mortality (0.50)
Low Social Class (0.90)
Example of decision tree with two chance nodes
For those who tolerate the
intervention, D has a lower
mortality than C
High Social Class (0.10)
Mortality (0.10)
Yes
(0.70)
SC
Mortality(0.20)
Tolerance
to
intervention
Low Social Class (0.90)
High Social Class (0.10)
No
(0.30)
Mortality (0.50)
SC
Mortality (0.50)
Decision Node
Low Social Class (0.90)
High Social Class (0.10)
Mortality (0.05)
Yes
(0.30)
SC
Mortality (0.10)
Low Social Class (0.90)
Tolerance
to
intervention
No
(0.70)
High Social Class (0.10)
Mortality (0.50)
SC
Mortality (0.50)
Low Social Class (0.90)
Example of decision tree with two chance nodes
For those who tolerate the
interventions, D has a lower
mortality than C
High Social Class (0.10)
Mortality (0.10)
Yes
(0.70)
SC
Mortality(0.20)
Tolerance
to
intervention
Low Social Class (0.90)
High Social Class (0.10)
No
(0.30)
Mortality (0.50)
SC
Mortality (0.50)
Decision Node
Low Social Class (0.90)
High Social Class (0.10)
Mortality (0.05)
Yes
(0.30)
SC
Mortality (0.10)
Low Social Class (0.90)
Tolerance
to
intervention
High Social Class (0.10)
Mortality (0.50)
SC
No
Thus,
(0.70)higher mortality
C: better tolerance,
Low Social Class (0.90)
D: worse tolerance, lower mortality
Mortality (0.50)
Example of decision tree with two chance nodes However, tolerance is better for
Program C
Table 2a – Program C: less efficacious but
better drug tolerance (70%)
Table 2b – Program D: more efficacious, but
less drug tolerance (only 30%)
Tolerance?
Joint probability of death
Tolerance?
Joint probability of death
Yes
0.70 × 0.10 × 0.10= 0.007
Yes
0.30 × 0.10 × 0.05= 0.0015
0.70 × 0.90 × 0.20= 0.126
No
0.30 × 0.10 × 0.50= 0.015
0.30 × 0.90 × 0.10= 0.027
No
0.70 × 0.10 × 0.50= 0.035
0.30 x 0.90 x 0.50= 0.135
0.70 × 0.90 × 0.50= 0.315
0.007 + 0.126 + 0.015 +
0.135= 0.283 or 28.30%
0.0015+ 0.027 + 0.035 +
0.315= 0.3785 or 37.85%
Conclude: Program D is more efficacious (i.e., those who tolerate the drug have a
lower mortality than in Program C), but because tolerance to Program C is higher, its
community effectiveness is higher.
Community effectiveness of C (compared with D)= {[37.85% - 28.30%] ÷ 37.85%} ×
100= 25.2%
THE END
Objectives of Epidemiology
(All Relevant to Cancer Control)
• Describe the magnitude of the disease burden in the population
• Examine the distribution of the disease in the population using
vital statistics data according to factors related to persons (e.g.,
age, gender), time and place;
• Investigate the etiology (risk factors) of disease;
• Assess effectiveness of preventive and curative strategies;
• Translate epidemiologic findings into public health policies.
Who, 2010. Global status report on noncommunicable diseases 2010
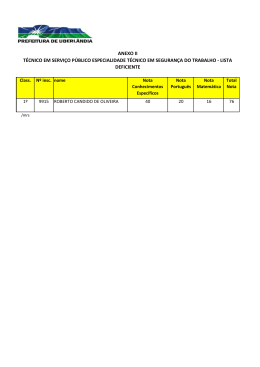
Número estimado de casos novos, por sexo,
Brasil, 2012
Homens
195190
Mulheres
189150
Localização Primária
Casos
novos
%
Próstata
60180
30,8
Traqueia, Brônquios e
Pulmão
17210
8,8
Cólon e reto
14180
7,3
Estômago
12670
6,5
Cavidade oral
9990
Esôfago
Localização Primária
Casos
novos
%
Mama
52680
27,9
Colo do útero
17540
9,3
Cólon e reto
15960
8,4
Tireoide
10590
5,6
5,1
Traqueia, Brônquios e
Pulmão
10110
5,3
7770
4,0
Estômago
7420
3,9
Bexiga
6210
3,2
Ovário
6190
3,3
Laringe
6110
3,1
Corpo do útero
4520
2,4
Linfoma Não-Hodgkin
5190
2,7
Cérebro, Sistema Nervoso
4450
2,4
Cérebro, Sistema Nervoso
4820
2,5
Linfoma Não-Hodgkin
4450
2,4
*Fonte:: MS/INCA/ Estimativa de Câncer no Brasil, 2012
MS/INCA/Conprev/Divisão de Informação
Distribuição das taxas brutas por 100 000 habitantes de incidência
estimadas para o ano de 2008, em homens e mulheres, segundo os
principais tipos de câncer.
52,43
Próstata
50,71
Mam a Fem inina
9,72
Colo do Útero
14,88
Traquéia, Brônquio e Pulm ão
18,86
7,93
Estôm ago
14,92
13,23
19,18
Cólon e Reto
11,00
3,88
Cavidade Oral
2,72
Esôfago
8,35
5,52
4,44
Leucem ias
3,09
3,03
Pele Melanom a
60
40
Fonte: MS/INCA/Conprev/Divisão de Informação
20
0
20
40
60
Registros de Câncer de Base
Populacional (RCBP)
*
*
*
*
*
*
*
*
Situação atual
Dos 32 implantados
27 RCBP estão ativos
*
*
*
*
*
*
* *
*
* *
*
**
*
*
*
*
Registro Hospitalar de Câncer - RHC
40-75% das informações da bases de
dados dos RHC já são transferidas
automaticamente para os RCBP por
meio da exportação do sistema
SisRHC/importação pelo BPW
Situação atual
241 RHC em atividade operacional em
CACON/UNACON
UNACON 87% tem RHC
CACON 100% tem RHC
Objectives of Epidemiology
(All Relevant to Cancer Control)
• Describe the magnitude of the disease burden in the population
• Examine the distribution of the disease in the population using
vital statistics data according to factors related to persons
(e.g., age, gender), time and place;
• Investigate the etiology (risk factors) of disease;
• Assess effectiveness of preventive and curative strategies;
• Translate epidemiologic findings into public health policies.
PLACE and PERSON (MEN)
Taxas de incidência estimadas (não ajustadas) para os tipos de
câncer mais frequentes (exceto câncer de pele não melanoma) em
homens, Brasil e regiões geográficas, 2012*
Brasil
Região
Norte
Região
Nordeste
Região
Centro-Oeste
Região
Sudeste
Região
Sul
1º
Próstata
(62,54)
Próstata
(29,72)
Próstata
(43,08)
Próstata
(74,65)
Próstata
(77,89)
Próstata
(68,36)
2º
Traqueia, Brônquio
e Pulmão
(17,90)
Estômago
(10,67)
Estômago
(8,99)
Traqueia, Brônquio
e Pulmão
(16,64)
Cólon e Reto
(22,12)
Traqueia, Brônquio
e Pulmão
(37,02)
3º
Cólon e reto
(14,75)
Cólon e Reto
(14,30)
Traqueia, Brônquio
e Pulmão
(19,73)
Cólon e Reto
(18,07)
4º
Estômago
(13,20)
Cólon e Reto
(3,99)
Cavidade Oral
(6,15)
Estômago
(13,84)
Estômago
(15,52)
Estômago
(15,72)
5º
Cavidade Oral
(10,41)
Leukaemia
Leucemias
Cólon e Reto
(5,31)
Cavidade Oral
(8,58)
Cavidade Oral
(14,61)
Esôfago
(15,27)
Traqueia, Brônquio Traqueia, Brônquio
e Pulmão
e Pulmão
(8,11)
(8,52)
(3,54)
*por 100.000 habitantes
Fonte: MS/INCA/ Estimativa de Câncer no Brasil, 2011/2012
MS/INCA/Conprev/Divisão de Informação e Análise de Situação
PLACE and PERSON (WOMEN)
Taxas de incidência estimadas (não ajustadas) para os tipos de câncer mais
frequentes (exceto câncer de pele não melanoma) em mulheres, Brasil e
regiões geográficas, 2012*
Brasil
Região
Norte
Região
Nordeste
Região
Centro-Oeste
Região
Sudeste
Região
Sul
1º
Mama feminina
(52,50)
Colo do útero
(23,62)
Mama feminina
(31,90)
Mama feminina
(47,56)
Mama feminina
(68,93)
Mama feminina
(64,80)
2º
Colo do útero
(17,49)
Mama feminina
(19,38)
Colo do útero
(17,96)
Colo do útero
(27,71)
Cólon e Reto
(23,01)
Cólon e Reto
(19,85)
3º
Cólon e Reto
(15,94)
Thyroid
Glândula
Tireoide
(7,34)
Cólon e Reto
(6,66)
Cólon e Reto
(14,71)
Colo do útero
(15,53)
Traqueia, Brônquio
e Pulmão
(18,58)
4º
Glândula Tireoide
(10,59)
Estômago
(5,83)
Glândula Tireoide
(6,01)
Traqueia, Brônquio
e Pulmão
(9,13)
Glândula Tireoide
(15,02)
Colo do útero
(13,88)
Estômago
(6,76)
Traqueia, Brônquio
e Pulmão
(11,22)
Glândula Tireoide
(10,28)
5º
Breast
Traqueia, Brônquio Traqueia, Brônquio Traqueia, Brônquio
e Pulmão
e Pulmão
e Pulmão
(10,08)
(5,12)
(5,64)
*por 100.000 habitantes
Fonte: MS/INCA/ Estimativa de Câncer no Brasil, 2011/2012
MS/INCA/Conprev/Divisão de Informação e Análise de Situação
Objectives of Epidemiology
(All Relevant to Cancer Control)
• Describe the magnitude of the disease burden in the population
• Examine the distribution of the disease in the population using
vital statistics data according to factors related to persons (e.g.,
age, gender), time and place;
• Investigate the etiology (risk factors) of disease:
• Case-control studies
• Cohort studies
• Assess effectiveness of preventive and curative strategies;
• Translate epidemiologic findings into public health policies.
Objectives of Epidemiology
(All Relevant to Cancer Control)
• Describe the magnitude of the disease burden in the population
• Examine the distribution of the disease in the population using
vital statistics data according to factors related to persons (e.g.,
age, gender), time and place;
• Investigate the etiology (risk factors) of disease;
• Assess effectiveness of preventive and curative strategies;
• Translate
• Pre-post studies
• Quasi-experimental studies
epidemiologic
findings into public
• Follow-up studies
- Prognostic studies
- Randomized Clinical Trials
health policies.
ESTUDOS BASEADOS EM SÉRIES TEMPORAIS UTILIZANDO DADOS
DE VIGILÂNCIA
Mortalidade
1. Estudo Pré-Pós
Inferências causais relacionadas a esse
desenho são robustas no caso de
“experimentos naturais” (exemplo: insulina,
estreptomicina)
Tempo
Introdução do programa
Outros programas? Mudanças nas características da população alvo?
ESTUDOS BASEADOS EM SÉRIES TEMPORAIS UTILIZANDO DADOS
DE VIGILÂNCIA
2. Estudo Quasi-experimental (Pré-Pós com Controles)
Mortalidade
A= intervenção
B= controle
A
B
A
Seguimento
B
(Adapted by Ibrahim M from D. Gillings et al. Am J Pub Hlth 71(1)38-46)
50
(1)
(2)
(3)
40
(4)
30
Taxas de
mortalidade
perinatal
(5)
20
Antes de o programa ser implementado,
a área que recebeu a intervenção tinha
taxas the mortalidade perinatal mais
elevadas do que a área controle, o que
pode explicar porque foi selecionada para
receber a intervenção
10
0
1935
1945
Intervenção
Controle
1955
Year
1965
Programa
1975
1985
(Adapted by Ibrahim M from D. Gillings et al. Am J Pub Hlth 71(1)38-46)
50
(1)
(2)
O aspecto mais importante
no estudo quasi-experimental
é a comparação dos ângulos
(3)
40
(4)
30
Taxas de
mortalidade
perinatal
(5)
20
10
0
1935
1945
Intervenção
Controle
1955
Year
1965
Programa
1975
1985
Follow-up Studies (Prognostic Studies and RCTs)
Losses to follow-up
Events (death, recurrence)
Factor (+)
INCIDENCEFACTOR (+)
Initial
sample
time
Final
sample
= RR
Losses to follow-up
Events (death, recurrence)
Factor (-)
INCIDENCEFACTOR (-)
Initial
sample
time
Final
sample
Age-Adjusted Death Rates/100 000, Relative Risks, and Attributable Risks for Lung Cancer—
Current Cigarette Smokers Vs Nonsmokers, Cancer Prevention Study I and CPS-II*
CPS-I (1959-1965)
CPS-II (1982-1988)
Nonsmoker
Current
Smoker
Nonsmoker
Current
Smoker
Rate
15.7
187.1
14.7
341.3
Relative Risk
1.0
11.9
1.0
23.2
Rate
9.6
26.1
12.0
154.6
Relative Risk
1.0
2.7
1.0
12.8
Men
Women
Age-Adjusted Death Rates/100 000, Relative Risks, and Attributable Risks for Lung Cancer—
Current Cigarette Smokers Vs Nonsmokers, Cancer Prevention Study I and CPS-II*
CPS-I (1959-1965)
CPS-II (1982-1988)
Nonsmoker
Current
Smoker
Nonsmoker
Current
Smoker
Rate
15.7
187.1
14.7
341.3
Relative Risk
1.0
11.9
1.0
23.2
Rate
9.6
26.1
12.0
154.6
Relative Risk
1.0
2.7
1.0
12.8
Men
Women
Age-Adjusted Death Rates/100 000, Relative Risks, and Attributable Risks for Lung Cancer—
Current Cigarette Smokers Vs Nonsmokers, Cancer Prevention Study I and CPS-II*
CPS-I (1959-1965)
CPS-II (1982-1988)
Nonsmoker
Current
Smoker
Nonsmoker
Current
Smoker
Rate
15.7
187.1
14.7
341.3
Relative Risk
1.0
11.9
1.0
23.2
Rate
9.6
26.1
12.0
154.6
Relative Risk
1.0
2.7
1.0
12.8
Men
Women
Às vezes, resultados de estudos epidemiológicos de prevenção
primária desapontam...
BC= beta carotene
AT= alpha tocopherol
Cumulative Incidence of Lung Cancer by Intervention Allocation
(Albanes D, et al. JNCI 1996;88:1560-70)
Forest plot of the effect of group counselling on the incidence of smoking abstinence. Use of nicotine patch, bupropion, and
notriptyline varied among studies (Motillo S, et al. Eur Heart J 2008 [Epub ahead of print Dec 24]
Interface between epidemiology and the
decision-making process
• Meta-Analysis
• Decision Analysis
Evaluation of community
effectiveness
• Cost-Effectiveness Analysis
(Pettiti DB. Meta-Analysis, Decision Analysis and Cost-Effectiveness Analysis. New
York, Oxford, Oxford University Press, 1994)
Interface between epidemiology and the
decision-making process
• Meta-Analysis
• Decision Analysis
Evaluation of community
effectiveness
• Cost-Effectiveness Analysis
(Pettiti DB. Meta-Analysis, Decision Analysis and Cost-Effectiveness Analysis. New
York, Oxford, Oxford University Press, 1994
Relations between meta-analysis, decision analysis and costeffectiveness analysis
Decision Analysis
Meta-Analysis
Summary of the
efficacy/effectiveness of the
intervention
Assessment of the relative value of the
programmatic options, based on their
community effectiveness (ideally determined
by meta-analysis)
Cost-effectiveness Analysis
Assessment of the cost of the program, based on the relative value
of the options
Decision Analysis: uses a quantitative approach to
evaluate the relative value (effectiveness) of one or more
interventions, programs or services.
Steps in Decision Analysis
• Identification and description of the problem
• Collection of the information needed to construct the
decision tree (ideally by means of meta-analysis)
• Construction of a decision tree
• Analysis of the decision tree
High Social Class (0.10)
Mortality (0.10)
Yes
(0.70)
SC
Mortality(0.20)
Tolerance
to
intervention
Low Social Class (0.90)
High Social Class (0.10)
No
(0.30)
Mortality (0.50)
SC
Mortality (0.50)
Decision Node
Low Social Class (0.90)
High Social Class (0.10)
Mortality (0.05)
Yes
(0.30)
SC
Mortality (0.10)
Low Social Class (0.90)
Tolerance
to
intervention
No
(0.70)
High Social Class (0.10)
Mortality (0.50)
SC
Mortality (0.50)
Low Social Class (0.90)
Example of decision tree with two chance nodes
For those who tolerate the
intervention, D has a lower
mortality than C
High Social Class (0.10)
Mortality (0.10)
Yes
(0.70)
SC
Mortality(0.20)
Tolerance
to
intervention
Low Social Class (0.90)
High Social Class (0.10)
No
(0.30)
Mortality (0.50)
SC
Mortality (0.50)
Decision Node
Low Social Class (0.90)
High Social Class (0.10)
Mortality (0.05)
Yes
(0.30)
SC
Mortality (0.10)
Low Social Class (0.90)
Tolerance
to
intervention
No
(0.70)
High Social Class (0.10)
Mortality (0.50)
SC
Mortality (0.50)
Low Social Class (0.90)
Example of decision tree with two chance nodes
For those who tolerate the
interventions, D has a lower
mortality than C
High Social Class (0.10)
Mortality (0.10)
Yes
(0.70)
SC
Mortality(0.20)
Tolerance
to
intervention
Low Social Class (0.90)
High Social Class (0.10)
No
(0.30)
Mortality (0.50)
SC
Mortality (0.50)
Decision Node
Low Social Class (0.90)
High Social Class (0.10)
Mortality (0.05)
Yes
(0.30)
SC
Mortality (0.10)
Low Social Class (0.90)
Tolerance
to
intervention
High Social Class (0.10)
Mortality (0.50)
SC
No
Thus,
(0.70)higher mortality
C: better tolerance,
Low Social Class (0.90)
D: worse tolerance, lower mortality
Mortality (0.50)
Example of decision tree with two chance nodes However, tolerance is better for
Program C
Table 2a – Program C: less efficacious but
better drug tolerance (70%)
Table 2b – Program D: more efficacious, but
less drug tolerance (only 30%)
Tolerance?
Joint probability of death
Tolerance?
Joint probability of death
Yes
0.70 × 0.10 × 0.10= 0.007
Yes
0.30 × 0.10 × 0.05= 0.0015
0.70 × 0.90 × 0.20= 0.126
No
0.30 × 0.10 × 0.50= 0.015
0.30 × 0.90 × 0.10= 0.027
No
0.70 × 0.10 × 0.50= 0.035
0.30 x 0.90 x 0.50= 0.135
0.70 × 0.90 × 0.50= 0.315
0.007 + 0.126 + 0.015 +
0.135= 0.283 or 28.30%
0.0015+ 0.027 + 0.035 +
0.315= 0.3785 or 37.85%
Conclude: Program D is more efficacious (i.e., those who tolerate the drug have a
lower mortality than in Program C), but because tolerance to Program C is higher, its
community effectiveness is higher.
Community effectiveness of C (compared with D)= {[37.85% - 28.30%] ÷ 37.85%} ×
100= 25.2%
Sensitivity Analysis: a Tool for Public
Health Policy
• Approach to examine the changes in the output
(results) of a given model resulting from varying
certain model parameters (or assumptions) over
a reasonable range (Szklo & Nieto. Epidemiology: Beyond the Basics.
2nd Edition, Jones & Bartlett, 2006).
Sensitivity Analysis: Assume that tolerance to the intervention in
Program D is increased to 50%
Table 2a – Program C: less efficacious, but
with better tolerance (70%)
Tolerance?
Joint probability of death
Yes
0.7 × 0.10 × 0.10= 0.007
0.70 × 0.90 × 0.20= 0.126
No
0.30 × 0.10 × 0.50= 0.015
0.30 x 0.90 x 0.50= 0.135
0.007 + 0.126 + 0.015 +
0.135= 0.283 or 28.30%
Sensitivity Analysis: Assume that tolerance to the intervention in
Program D is increased to 50%
Table 2a – Program C: less efficacious, but
with better tolerance (70%)
Table 2c – Program D with tolerance
improved to 50%
Tolerance?
Joint probability of death
Tolerance?
Joint probability of death
Yes
0.7 × 0.10 × 0.10= 0.007
Yes
0.50 × 0.10 × 0.05= 0.0025
0.70 × 0.90 × 0.20= 0.126
No
0.30 × 0.10 × 0.50= 0.015
0.50 × 0.90 × 0.10= 0.045
No
0.50 × 0.10 × 0.50= 0.025
0.30 x 0.90 x 0.50= 0.135
0. 50 × 0.90 × 0.50= 0.225
0.007 + 0.126 + 0.015 +
0.135= 0.283 or 28.30%
0.0025 + 0.045 + 0.025 +
0.225= 0.2975 or 29.75%
(Before: 37.85%)
Community effectiveness of C (vis-a-vis D)= {[29.75% - 28.30%] ÷ 29.75%} × 100= 4.9%
Program C is still a bit more effective than Program D, but if the cost
of D is lower, it may be cost-effective to implement Program D
FIM
Risk Factors for Brain Tumors in Subjects Aged <20 years: A Case-Control
Study
(Gold et al, Am J Epidemiol 1979;109:309-19)
•
Exploratory study of risk factors for brain tumors
•
Subjects < 20 yrs old
•
Cases: primary malignant brain tumors in Baltimore in 1965-75
•
Normal controls: chosen from birth certificates on file, and matched on cases by sex,
date of birth (±1 year) and race
•
Interviews with parents of children
•
Exposed: children with birthweight equal or above the median (3629 g)
•
Unexposed: children with birthweight below the median
•
Odds ratio= 2.6
Cohort (prospective) study
2009
= RR
INCIDENCEUNEXP
Unexposed
(2) Follow-up from
present to future
INCIDENCEEXP
(1) Investigator
selects
Exposed
2029
Non-concurrent cohort (prospective) study (also
known as historical cohort study
Follow-up from past to present:
Unexposed
1989
“Follow-up”
from ’89-’09
INCUNEXP
Exposed
INCEXP
(2) Investigator
reconstructs
cohort:
(1) At present
investigator has
access to database
created in 1988
2009
Unexposed
2009
Follow-up from
present to future
2029
1989
INCUNEXP
Unexposed
Follow-up
from ’89-’09
INCEXP
NON-CONCURRENT
Exposed
2009
INCUNEXP
Exposed
INCEXP
CONCURRENT
Both studies start
in year 2009
Unexposed
2009
Follow-up from
present to future
INCUNEXP
Exposed
INCEXP
CONCURRENT
2029
Unexposed
1989
Follow-up
from ’89-’09
INCUNEXP
Exposed
INCEXP
NON-CONCURRENT
2009
In both studies, the initial
selection (or classification)
is based on the exposure,
and the outcome (unknown
variable) is incidence
Example of Non-concurrent Prospective Study (Yeh et
al, Am J Epidemiol 2001;153:749-56)
• Study subjects identified by investigators in 2000 as having
been seen in a Clinic for Prevention of Deafness in
Washington County, MD, from 1940-60, for elimination of
nasopharyngeal lymphoid tissues.
• Exposed: Individuals who had nasopharyngeal radium
treatment (n=808).
• Unexposed: Individuals who received other treatments (e.g.,
tonsillectomy) (n=1819).
• Outcome: Cancer Incidence
• Follow-up through 1995.
Design of Study Done by Yeh et al, Am J
Epidemiol 2001;153:749-56
FOLLOW-UP:35 YEARS
FOLLOW-UP THROUGH 1995
Adjustment for variable
follow-up times: Rate per
person-years and
Survival analysis
FOLLOW-UP: 55 YEARS
1940
1960
Reconstruction
of cohort
1995
Time
Study done in 2000
Relative Risk of Cancer Incidence (95% Confidence Interval)
According to Exposure to Nasopharyngeal Radium Therapy,
Washington County, Maryland 1940-95
Cancer type
All neoplasms,
except skin
Oral cavity,
pharynx, and
thyroid
No. cases in
exposed group
(PY= 31,005)
No. cases in
unexposed group
(PY= 65,502)
Adjusted Relative
Risk (95% CI)
41
83
1.02 (0.7, 1.5)
4
2
4.22 (0.38, 46.6)
Biologically plausible
(Yeh et al, Am J Epidemiol 2001;153:749-56)
Confounding variable:
Intervention
800
200
500
500
No. Deaths: 80
100
50
250
Mortality:
Absent, mortality = 10%
No intervention
180
300
18%
30%
Present, mortality = 50%
One of the solutions to eliminate
confounding: stratify
Mortality according to the intervention, stratified by the confounder
Confounding
variable:
Present
Absent
Intervention:
N
No. of
deaths
Mortality
Yes
200
100
50.0%
No
500
250
50.0%
Yes
800
80
10.0%
No
500
50
10.0%
CONFOUNDING EFFECT
Exposure
Confounder
Outcome
` and not in the causality pathway between
exposure and outcome:
Exposure
Confounder
Outcome
Sensitivity Analysis: a Tool for Public
Health Policy
• Approach to examine the changes in the output
(results) of a given model resulting from varying
certain model parameters (or assumptions) over
a reasonable range (Szklo & Nieto. Epidemiology: Beyond the Basics.
2nd Edition, Jones & Bartlett, 2006).
Sensitivity Analysis: Assume that tolerance to the intervention in
Program D is increased to 50%
Table 2a – Program C: less efficacious, but
with better tolerance (70%)
Tolerance?
Joint probability of death
Yes
0.7 × 0.10 × 0.10= 0.007
0.70 × 0.90 × 0.20= 0.126
No
0.30 × 0.10 × 0.50= 0.015
0.30 x 0.90 x 0.50= 0.135
0.007 + 0.126 + 0.015 +
0.135= 0.283 or 28.30%
Sensitivity Analysis: Assume that tolerance to the intervention in
Program D is increased to 50%
Table 2a – Program C: less efficacious, but
with better tolerance (70%)
Table 2c – Program D with tolerance
improved to 50%
Tolerance?
Joint probability of death
Tolerance?
Joint probability of death
Yes
0.7 × 0.10 × 0.10= 0.007
Yes
0.50 × 0.10 × 0.05= 0.0025
0.70 × 0.90 × 0.20= 0.126
No
0.30 × 0.10 × 0.50= 0.015
0.50 × 0.90 × 0.10= 0.045
No
0.50 × 0.10 × 0.50= 0.025
0.30 x 0.90 x 0.50= 0.135
0. 50 × 0.90 × 0.50= 0.225
0.007 + 0.126 + 0.015 +
0.135= 0.283 or 28.30%
0.0025 + 0.045 + 0.025 +
0.225= 0.2975 or 29.75%
(Before: 37.85%)
Community effectiveness of C (vis-a-vis D)= {[29.75% - 28.30%] ÷ 29.75%} × 100= 4.9%
Program C is still a bit more effective than Program D, but if the cost
of D is lower, it may be cost-effective to implement Program D
Decision Analysis: uses a quantitative approach to
evaluate the relative value (effectiveness) of one or more
interventions, programs or services.
Steps in Decision Analysis
• Identification and description of the problem
• Collection of the information needed to construct the
decision tree (ideally by means of meta-analysis)
• Construction of a decision tree
• Analysis of the decision tree
• (Optional): Sensitivity analysis
DECISION TREE
• Decision node: under the investigator’s control
• Chance (or probability) node: not under the investigator’s control
Example of a Decision Tree
High Social Class
Outcome*
Program A
Chance node
Low Social Class
Decision Node
High Social Class
Outcome*
Outcome*
Chance node
Program B
Low Social Class
*For example, mortality
Outcome*
Example of Decision Tree (Probabilities)
Mortality (0.20)
High Social Class
Program A
(0.10)
Chance node
Mortality (0.40)
Low Social Class
(0.90)
Decision Node
Mortality (0.90)
High Social Class
Program B
(0.10)
Chance node
Mortality (0.90)
Low Social Class
(0.90)
Note that the distribution of social class is same in both programs, as they are being
considered for the same target population
Example of Decision Tree (Probabilities)
Mortality (0.20)
High Social Class
Program A
(0.10)
Chance node
Decision Node
Death (0.90)
High Social Class
Survival (0.10)
Program B
Chance node
Death (0.90)
What is the joint probability of high socialLow
class
(HSC)
and mortality in program A?
Social
Class
Survival (0.10)
Proportion HSC × Mort. A = 0.10 × 0.20= 0.02
Example of Decision Tree (Probabilities)
Program A
Chance node
Mortality (0.40)
Low Social Class
(0.90)
Decision Node
Death (0.90)
High Social Class
(0.10)
Survival (0.10)
Program B
Chance node
Death (0.90)
What is the joint probability of low social Low
class
(LSC)
and mortality
in program A?
Social
Class
(0.90)
Survival (0.10)
Proportion LSC × Mort. A = 0.90 × 0.40= 0.36
Example of Decision Tree (Probabilities)
Mortality (0.20)
High Social Class
Program A
(0.10)
Chance node
Mortality (0.40)
Low Social Class
(0.90)
Decision Node
Death (0.90)
High Social Class
(0.10)
Survival (0.10)
Program B
Chance node
Death (0.90)
What is the joint mortality of Low
all individuals
A?
Social Classin program
(0.90)
Survival (0.10)
Mort. HSC + LSC= (0.10 × 0.02) + (0.90 × 0.40)= 0.02 + 0.36= 0.38
Example of Decision Tree (Probabilities)
Mortality (0.20)
High Social Class
Program A
(0.10)
Chance node
Mortality (0.40)
Low Social Class
(0.90)
Decision Node
Mortality (0.90)
High Social Class
Program B
(0.10)
Chance node
Mortality (0.90)
Low Social Class
(0.90)
Decision Tree: Program A versus Program B
Program A
Social Class
Proportion in Each
Social Class
Mortality in Each
Social Class
Overall Mortality
High
0.10
0.20
0.10 × 0.20 = 0.02
Low
0.90
0.40
0.90 × 0.40 = 0.36
Total
0.02 + 0.36 = 0.38
Program B
Social Class
Proportion in Each
Social Class
Mortality in Each
Social Class
Overall Mortality
High
0.10
0.90
0.10 × 0.90 = 0.09
Low
0.90
0.90
0.90 × 0.90 = 0.81
Total
0.09 + 0.81 = 0.90
Community effectiveness of A versus B*= [(0.90 – 0.38) / 0.90] × 100 = 57.8%
* That is, treating program A as the “experimental” program and program B as the “control” program
INTERFACE BETWEEN EPIDEMIOLOGY AND PUBLIC HEALTH POLICY
1. BURDEN OF ILLNESS
Determine health status
(mortality, prevalence,
incidence, years of
potential life lost, etc.
6. REASSESSMENT
Reassessment of magnitude of
burden of illness or risk factor
INTERFACE BETWEEN
EPIDEMIOLOGY AND PUBLIC
HEALTH POLICY
2. ETIOLOGY
Identify and assess possible
causes of disease and risk
factor burden
5. MONITORING OF PROGRAM
Ongoing monitoring using markers
selected to indicate success
4. COST-EFFECTIVENESS
Determine relationships between
costs and effectiveness of options
within and across programs
Modified from: Tugwell et al, J Chron Dis 38(4)
3. COMMUNITY EFFECTIVENESS
Assess benefit/harm ratio of potentially
feasible interventions and estimate
reduction of burden of illness if programs
are effective
Odds ratio= (ad) / (bc)
Other Cancer Controls
Case
Control
Smokers
236(a)
666 (b)
Nonsmokers
122(c)
722 (d)
Lung,
Non-tumor Controls
Case
Control
Smokers
236
124
Nonsmokers
122
110
Other,
Non-cancer Controls
Case
Control
Smokers
236
481
Nonsmokers
122
612
OR= (236 × 722) ÷ (666 × 122)= 2.10
OR = 1.72
OR = 2.46
95% CI: 1.6-2.7
95% CI: 1.2-2.4
95% CI: 1.9-3.2
Levin ML, Goldstein H and Gerhardt PR: Cancer and Tobacco Smoking. A Preliminary Report. JAMA,
143:336-338, 1950.
Objectives of Epidemiology
• Describe the magnitude of the disease burden in the population
• Examine the distribution of the disease in the population using
vital statistics data according to factors related to persons (e.g.,
age, gender), time and place;
• Investigate the etiology (risk factors) of disease;
• Assess effectiveness of preventive strategies;
• Translate epidemiologic findings into public health policies
(INCA-MS Estimativas 2006 – Incidencia de Cancer no Brasil)
Objectives of Epidemiology
• Describe the magnitude of the disease burden in the population
• Examine the distribution of the disease in the population
using vital statistics data according to factors related to
persons (e.g., age, gender), time and place;
• Investigate the etiology (risk factors) of disease;
• Assess effectiveness of preventive strategies.
Decision Tree with Multiple Chance Nodes
Decision tree for the treatment of high blood pressure based on 52 hypertensive patients. Values besides each
outcome health state are median and inter-quartile range. CVE, cardiovascular event (newly diagnosed angina,
myocardial infarction, coronary heart disease, stroke or transient ischemic attack)
(Montgomery AA, et al. Shared decision making in hypertension. Family Practice 2001;18:309-313).
INTERFACE BETWEEN EPIDEMIOLOGY AND CANCER CONTROL POLICY
1. BURDEN OF ILLNESS
Determine health status
(mortality, incidence,
etc.)
6. REASSESSMENT
Reassessment of magnitude of
burden of illness or risk factor
INTERFACE BETWEEN
EPIDEMIOLOGY AND PUBLIC
HEALTH POLICY
5. MONITORING OF PROGRAM
(SURVEILLANCE)
Ongoing monitoring
4. COST-EFFECTIVENESS
Determine relationships between
costs and effectiveness across
programs
Modified from: Tugwell et al, J Chron Dis 38(4)
2. ETIOLOGY AND
EFFICACY
Identify risk factors and
assess efficacy of primary
and secondary prevention
strategies
3. COMMUNITY EFFECTIVENESS
Assess effectiveness in the target
community
INTERFACE BETWEEN EPIDEMIOLOGY AND CANCER CONTROL POLICY
1. BURDEN OF ILLNESS
Determine health status
(mortality, incidence,
etc.)
6. REASSESSMENT
Reassessment of magnitude of
burden of illness or risk factor
INTERFACE BETWEEN
EPIDEMIOLOGY AND PUBLIC
HEALTH POLICY
5. MONITORING OF PROGRAM
(SURVEILLANCE)
Ongoing monitoring
4. COST-EFFECTIVENESS
Determine relationships between
costs and effectiveness across
programs
Modified from: Tugwell et al, J Chron Dis 38(4)
2. ETIOLOGY AND
EFFICACY
Identify risk factors and
assess efficacy of primary
and secondary prevention
strategies
3. COMMUNITY EFFECTIVENESS
Assess effectiveness in the target
community
INTERFACE BETWEEN EPIDEMIOLOGY AND CANCER CONTROL POLICY
1. BURDEN OF ILLNESS
Determine health status
(mortality, incidence,
etc.)
6. REASSESSMENT
Reassessment of magnitude of
burden of illness or risk factor
INTERFACE BETWEEN
EPIDEMIOLOGY AND PUBLIC
HEALTH POLICY
5. MONITORING OF PROGRAM
(SURVEILLANCE)
Ongoing monitoring
4. COST-EFFECTIVENESS
Determine relationships between
costs and effectiveness across
programs
Modified from: Tugwell et al, J Chron Dis 38(4)
2. ETIOLOGY AND
EFFICACY
Identify risk factors and
assess efficacy of
primary and secondary
prevention strategies
3. COMMUNITY EFFECTIVENESS
Assess effectiveness in the target
community
INTERFACE BETWEEN EPIDEMIOLOGY AND CANCER CONTROL POLICY
1. BURDEN OF ILLNESS
Determine health status
(mortality, incidence,
etc.)
6. REASSESSMENT
Reassessment of magnitude of
burden of illness or risk factor
INTERFACE BETWEEN
EPIDEMIOLOGY AND PUBLIC
HEALTH POLICY
5. MONITORING OF PROGRAM
(SURVEILLANCE)
Ongoing monitoring
4. COST-EFFECTIVENESS
Determine relationships between
costs and effectiveness across
programs
Modified from: Tugwell et al, J Chron Dis 38(4)
2. ETIOLOGY AND
EFFICACY
Identify risk factors and
assess efficacy of primary
and secondary prevention
strategies
3. COMMUNITY EFFECTIVENESS
Assess effectiveness in the target
community
INTERFACE BETWEEN EPIDEMIOLOGY AND CANCER CONTROL POLICY
1. BURDEN OF ILLNESS
Determine health status
(mortality, incidence,
etc.)
6. REASSESSMENT
Reassessment of magnitude of
burden of illness or risk factor
INTERFACE BETWEEN
EPIDEMIOLOGY AND PUBLIC
HEALTH POLICY
5. MONITORING OF PROGRAM
(SURVEILLANCE)
Ongoing monitoring
4. COST-EFFECTIVENESS
Determine relationships
between costs and
effectiveness across programs
Modified from: Tugwell et al, J Chron Dis 38(4)
2. ETIOLOGY AND
EFFICACY
Identify risk factors and
assess efficacy of primary
and secondary prevention
strategies
3. COMMUNITY EFFECTIVENESS
Assess effectiveness in the target
community
INTERFACE BETWEEN EPIDEMIOLOGY AND CANCER CONTROL POLICY
1. BURDEN OF ILLNESS
Determine health status
(mortality, incidence,
etc.)
6. REASSESSMENT
Reassessment of magnitude of
burden of illness or risk factor
INTERFACE BETWEEN
EPIDEMIOLOGY AND PUBLIC
HEALTH POLICY
5. MONITORING OF PROGRAM
(SURVEILLANCE)
Ongoing monitoring
4. COST-EFFECTIVENESS
Determine relationships between
costs and effectiveness across
programs
Modified from: Tugwell et al, J Chron Dis 38(4)
2. ETIOLOGY AND
EFFICACY
Identify risk factors and
assess efficacy of primary
and secondary prevention
strategies
3. COMMUNITY EFFECTIVENESS
Assess effectiveness in the target
community
INTERFACE BETWEEN EPIDEMIOLOGY AND CANCER CONTROL POLICY
1. BURDEN OF ILLNESS
Determine health status
(mortality, incidence,
etc.)
6. REASSESSMENT
Reassessment of magnitude
of burden of illness or risk
factor
INTERFACE BETWEEN
EPIDEMIOLOGY AND PUBLIC
HEALTH POLICY
5. MONITORING OF PROGRAM
(SURVEILLANCE)
Ongoing monitoring
4. COST-EFFECTIVENESS
Determine relationships between
costs and effectiveness across
programs
Modified from: Tugwell et al, J Chron Dis 38(4)
2. ETIOLOGY AND
EFFICACY
Identify risk factors and
assess efficacy of primary
and secondary prevention
strategies
3. COMMUNITY EFFECTIVENESS
Assess effectiveness in the target
community
Processo de Implementação de Politicas de Controle do Câncer Baseadas em
Evidências
Magnitude das DCNT
Políticas baseadas em
evidências
Vigilância
Aquisição de evidências
científicas
• Ensaios
aleatorizados
• Estudos de coorte
• Estudos de casos e
controles
• Estudos de séries
temporais
• Estudos de
processo e estrutura
• Estudos
conduzidos de
novo:: análise de tendências
Revisões
sistemáticas
• Colaboração
Cochrane
• Outras fontes
(meta-análises
publicadas em
revistas)
• Revisões
Sistemáticas e
meta-análises
realizadas de
novo
Custoefetividade
Análise de
sensibilidade
• Evidências
• Obstáculos
• Avaliação de níveis
de evidência
• Seleção de opções
programáticas
(análise de decisão)
• Recomendações
• Hipóteses causais
• Avaliação de intervenções, políticas e programas
• Avaliação de niveis epidêmicos (inclusive “clusters)
(Modificado de Dickersin K)
Aplicação da politica:
planejamento
Tradução de conhecimentos
Cumulative incidence
Prostate Cancer Deaths in the European Randomized
Study of Screening for Prostate Cancer (Schroder FH, et
al. New Eng J Med 2009;360:1320-8)
Prostate Cancer Deaths in the Prostate, Lung,
Colorectal and Ovarian Cancer Screening Trial
(Andriole GL et al, New Eng J Med 2009;360:1310-9)
(Holder AM, Gonzalez-Angulo AM, Chen H, et al. High
stearoyl-CoA desaturase 1 expression is associated with
shorter survival in breast cancer patients. Breast Cancer
Res Treat [epubl, Dec 2012])
Assumption Justifying a Screening Program
•
In the absence of intervention, all or most cases in a pre-clinical phase progress to
the clinical phase (may not be true for certain cancers; e.g., prostate)
Início da
exposição a
fatores de
risco
Momento em que
a detecção
precoce se torna
possivel
Início da
enfermidade
Detecção
baseada em
sintomas ou
sinais que
ocorrem no
início da
fase clínica,
Fase pré-clínica detectável (FPCD)
Cura ou Morte
Fase clinica
Fase pré-clínica não
detectável
(INSERT DATA FROM BREAST CANCER (Bleyer A, Welch HG. Effect of three decades of screening mammography on breast
cancer incidence. New Eng J Med 2012;367:21)
•
•
•
•
•
•
•
•
•
•
•
•
•
•
Algumas atividades de prevenção primária
custo-efetivas sugeridas por estudos epidemiologicos (OMS)
Proteção contra a fumaça do tabaco e proibição de fumo em
ambientes públicos
Alertas com relação aos perigos do uso de tabaco
Implementação da proibição de propaganda, promoção e patrocínio
de eventos por tabaco
Aumento de impostos de produtos de tabaco
Restrição de acesso a álcool em negócios
Implementação de proibição de propaganda de bebidas alcólicas
Aumento de impostos de bebidas alcólicas
Redução de consumo de sal e quantidade de sal em alimentos
processados
Substituição de gorduras “trans” por gorduras poli-não saturadas
Conscientização do público sobre importância de dieta saudável e
atividade física, inclusive através de meios de comunicação
Controle de glicemia em pacientes com 30 anos ou menos com
diabetes se o risco de eventos agudos cardiovasculares for ≥30%
nos próximos 10 anos
Aspirina para prevenção de infarto agudo do miocárdio
Mamografia a cada 2 anos para mulheres de 50 a 70 anos
Detecção precoce de câncer colo-retal
•
•
•
•
•
•
•
•
•
•
•
•
•
•
Algumas atividades de prevenção primária
custo-efetivas sugeridas por estudos epidemiologicos (OMS)
Proteção contra a fumaça do tabaco e proibição de fumo em
ambientes públicos
Alertas com relação aos perigos do uso de tabaco
Implementação da proibição de propaganda, promoção e patrocínio
de eventos por tabaco
Aumento de impostos de produtos de tabaco
Restrição de acesso a álcool em negócios
Implementação de proibição de propaganda de bebidas alcólicas
Aumento de impostos de bebidas alcólicas
Redução de consumo de sal e quantidade de sal em alimentos
processados
Substituição de gorduras “trans” por gorduras poli-não saturadas
Conscientização do público sobre importância de dieta saudável e
atividade física, inclusive através de meios de comunicação
Controle de glicemia em pacientes com 30 anos ou menos com
diabetes se o risco de eventos agudos cardiovasculares for ≥30%
nos próximos 10 anos
Aspirina para prevenção de infarto agudo do miocárdio
Mamografia a cada 2 anos para mulheres de 50 a 70 anos
Detecção precoce de câncer colo-retal
•
•
•
•
•
•
•
•
•
•
•
•
•
•
Algumas atividades de prevenção primária
custo-efetivas sugeridas por estudos epidemiologicos (OMS)
Proteção contra a fumaça do tabaco e proibição de fumo em
ambientes públicos
Alertas com relação aos perigos do uso de tabaco
Implementação da proibição de propaganda, promoção e patrocínio
de eventos por tabaco
Aumento de impostos de produtos de tabaco
Restrição de acesso a álcool em negócios
Implementação de proibição de propaganda de bebidas alcólicas
Aumento de impostos de bebidas alcólicas
Redução de consumo de sal e quantidade de sal em alimentos
processados
Substituição de gorduras “trans” por gorduras poli-não saturadas
Conscientização do público sobre importância de dieta saudável e
atividade física, inclusive através de meios de comunicação
Controle de glicemia em pacientes com 30 anos ou menos com
diabetes se o risco de eventos agudos cardiovasculares for ≥30%
nos próximos 10 anos
Aspirina para prevenção de infarto agudo do miocárdio
Mamografia a cada 2 anos para mulheres de 50 a 70 anos
Detecção precoce de câncer colo-retal
Download