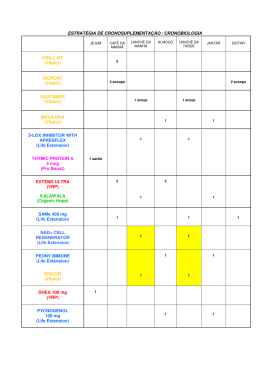
MINIATURIZED BLOOD PUMP FOR HEART ASSIST OR VENTRICULAR ASSIST DEVICE: PROJECT AND INITIAL IN VITRO TESTS Bruno Silva1,2, Adib Jatene1, Juliana Leme1,2, Eduardo Bock1,2, Cibele Silva1,2, Jeison Fonseca1, Pedro Antunes1, Beatriz Uebelhart1,2, Aron Andrade1, Carlos Suzuki2 1 Bioengineering Department, Engineering Center for Circulatory Support, Institute Dante Pazzanese of Cardiology, São Paulo (SP), Brazil 2 Materials Department, Faculty of Mechanical Engineering, State University of Campinas, Campinas (SP), Brazil E-mail: [email protected] Abstract. A miniaturized blood pump to help a diseased heart, have been developed. This work shows the first in vitro tests to determine the geometric characteristics of the pump. A hydrodynamic test was conduced, and the results showed that a pump with a medium displacement of the center axis and a tangent outlet cannula, would be able to achieve higher flow and pressure. But the hydrodynamic test with different impeller channels appointed no difference in performance of the pump. To obtain data of physical interaction of the pump with the blood and of the trauma caused by the impeller configuration on the blood cells, the Normalized Index of Hemolisys was determined for two pumps. A pump with a cross channel impeller presented a NIH of 0.06 g/100l, and the pump with a swastika impeller configuration presented a NIH of 0.003 g/100l. The results indicated that a pump with a medium displacement of the center axis, a tangent outlet cannula and an impeller with a swastika channel configuration, would give a higher hydrodynamic performance and a less traumatic feature to the blood cells. Background. Cardiovascular diseases were responsible for 30% of the deaths in the world, in 2008, 56 millions of deaths by cardiovascular diseases worldwide were registered (WHO, 2008). In some end-stage cardiac diseases, the best treatment is heart transplantation. However, a transplant involves many conditions that must be satisfied, for the procedure to be successful, like a perfect biological compatibility and a planned logistics for organ transport, etc. In the US, in 2007, 2140 heart transplants were realized and 3112 patients entered in the waiting list (HRSA/OPTN/SRTR, 2008). The mortality rate in the waiting list was 170 per 1000 patients/year at risk (JOHNSON, 2010). In Brazil, cardiovascular diseases represents 27.9% of the deaths (Secretary of Health Surveillance, 2004). In 2008, 200 heart transplants were performed in Brazil and 381 patients were in the waiting list in the end of the year, and death rates in the waiting list are still not available (BAOT, 2008). An option for the transplant is the use of a blood pump, implanted with the diseased natural heart, to keep the cardiac output (blood flow) and the arterial pressure in the cardiovascular system. When a blood pump is implanted to assist one ventricle, it is called Ventricular Assist device (VAD). The objective of the present research is to develop and to make initial in vitro test of a miniaturized centrifugal blood pump for ventricular assistance. Description of the pump. The pump principle is based on the impulsion of the blood by a centrifugal force, generated by the rotation of an impeller. There are in the impeller four isolated magnets (equidistant 45 degree from each other) that are responsible for the coupling with the stator. The diminished dimensions of the pump are projected to present a faster, easier and less traumatic implantation. The pump implantation is intended to be with an apex-aortic cannulation, where the inlet of the pump is connected, to the left ventricle apex and the pump outlet is connected to the ascending aorta (BOCK, 2011). The pump inlet is put directly in the ventricle and the pump remains fixed with the natural heart, as showed in figure 1. B A Figure 1 – Picture of a heart model showing the device position when implanted. Arrows indicate the flow path. A – Inlet cannula remains inside the ventricle. B - Device outlet connected to the aorta. Methods and results Hydrodynamic performance of the device. This study followed the methodology proposed by Nosé in 1998, called “step by step”, which is based on the experiments and further progression through preliminary results (NOSÉ, 1998). The dimensions of the device were defined considering the anatomical position of the device when implanted. To obtain the hydrodynamic data a circuit was assembled (Figure 2) composed by two pressure transducers (one in the device inlet and the other one in the device outlet) (Dome, GabMed, São Paulo, Brazil), a Polygraph (SP12, TEB, São Paulo, Brazil), a reservoir (Vital, Edwards, São Paulo, Brazil) and an ultrasonic flowmeter (HT110,Transonic System, Ithaca, US). A drive module (Bioconsole 540, Meditronic, Minneapolis, US) was used instead of a stator, for pump actuation., pressure was adjusted by a clamp positioned in the device outlet. Pump Clamp Flowmeter Reservoir Drive module Polygraph Figure 2 – Circuit used for hydrodynamic testing. The curve in figure 4 shows graph (pressure mmHg x Flow l/min) with a comparison between different center points of the internal wall of the pump cover in different rotation speeds (2500 rpm, 3000 rpm and 3500 rpm), the displaced center points cause a non continuous gap among the rotor and the cover. Three different displacements were tested, 3mm (high displacement Figure 3a), 1mm (medium displacement Figure 3b) and a pump with no displacement (Figure 3c). a b c Figure 3 – Schematic drawing showing the displacement of the pump cover from the center axis (cross point of the lines), the arrows indicate the movement of the impeller (central circle in white). 3a - high displacement. 3b – medium displacement. 3c – no displacement. Figure 4 – Graph with hydrodynamic curves for different center axis displacements. Using the same circuit another hydrodynamic study were performed to define the positioning of the outlet cannula, two prototypes were compared, one with the outlet cannula in the center line and other prototype with the outlet cannula tangent to the pump cover. Figure 5 show the positioning of the two cannulas and Figure 6 presents the graph comparing the curves of both prototypes. a b Figure 5 – Schematic drawing of different positioning of the outlet cannula, the arrows indicate the movement of the impeller. 5a – Cannula tangent to the pump cover. 5b – Cannula in the center of the cover (90º outlet cannula). Figure 6 – Graph comparing the hydrodynamic performance from different cannula positioning. The third hydrodynamic test was done with two different impeller channel configuration (cross and swastika Figures 7a and 7b respectively), the graph in Figure 8 shows the hydrodynamic performance curve for the rotation speeds of 2500 rpm and 2000 rpm, as in the other tests only one characteristic was changed. a b Figure 7 – Schematic drawing of the impeller channel configuration. 7a – Channels in “Cross”. 7b – Channels in “swastika”. Figure 8 – Hydrodynamic performance curve for different impeller channel configuration. Atraumatic feature pre-test. The physical interaction of the pump with the blood characterization is evaluated by determining the Normalized Index of Hemolysis (NIH), which indicated the destruction of red blood cells by mechanical action of the pump (NOSÉ, 1997). The NIH is calculated through equation (1) and (2), by determining the free Hemoglobin in plasma. Hemoglobin a red blood cells protein, which is important for carrying oxygen and when a red cell is destructed the hemoglobin is released in plasma. ( ) , Equation 1 where: PFH is the free hemoglobin in plasma (mg/dl), 83.6 is a reference factor, A 405 is a value read from the filter of 405nm, A 340 is a value read from the filter of 340nm and A 505 is a value read from the filter of 505nm. – , Equation 2 where: NIH is the normalized Index of Hemolysis (g/100l), ΔPFH is the variation of the free hemoglobin in plasma (mg/dl), V is the total volume of pumped blood (l), Ht is the hematocrit (%). Q corresponds to flow (l/min.) and Δt is the time between samples (min). The test followed the standards ASTM F1841 and ASTM F1830. Two pumps were tested, medium displacement, with the outlet tangential and outlet cannula. Each pump used a different impeller (channels in cross and channels in swastika, see Figure 7a and 7b).Table 1 shows the NIH and PFH for both of the pumps. Sample Table 1 – PFH and NIH for the tested pumps. PFH (mg/dl) NIH (g/100l) Cross Swastika Cross Swastika 0 4,5 2,4 - - 1 25,1 6,1 0,04 0,001 2 3 48,9 7,5 0,05 0,001 90,5 8,3 0,09 0,002 4 113,3 9,0 0,05 0,007 Standard deviation 0,02 0,002 0,02 0,002 Media 0,06 0,003 0,06 0,003 Discussions For all hydrodynamic tests, every pump tested showed that the estimated values of pressure and flow (75 to 100 mmHg and 3 to 5 l/min) needed for a blood pump to be used as a DAV, were achieved. Also, the hydrodynamic tests appointed that a pump with a medium displacement of the center axis, an outlet cannula tangent to the pump cover would present a higher hydrodynamic performance (Figures 4 and 6). However, in the hydrodynamic test of the impeller channels (Figure 8), no significant difference occurred, even though the impeller with channels in cross showed a slightly higher performance. To obtain data from the interaction of the pump with the blood cells the NIH were determinated for two pumps each one with an impeller channel configuration. A study conducted by Nosé in 1998 revealed that the design objective of the blood pump would be to obtain a NIH lower than 0.01g/100l, but a VAD could be implanted for long term with a NIH of 0.06 g/100l (NOSÉ, 1998). The NIH of the pumps were 0.06 g/100l for the pump with the impeller with the channels in cross, and 0.003 g/l for the pump with the impeller channels in swastika. Conclusion Based on the hydrodynamic tests and the NIH of the prototypes, the combination of a medium displacement, a tangent outlet cannula and a swastika channeled impeller presented a higher hydrodynamic performance and a less traumatic feature on the blood cells. The next step for the pump development is to use a cardiovascular simulator to study the performance of the pump and the response of a diseased cardiovascular system when the pump is implanted. Keywords Blood pump, in vitro testing, ventricular assist device. Acknowledgments The authors would like to acknowledge: CNPq, FAPESP, HCor, Adib Jatene Foundation, Brazilian Ministry of Heath – Secretary of Science, Technology and Strategic Inputs – Department of Science and Technology, for their support in this study. B.U. Silva also acknowledges the scholarship form CNPq. References. BAOT – Brazilian Association of Organs Transplantation. Brazilian Registry of Transplants – year xiv number 2, January - December, 2008. BOCK, E; et al. Implantable Centrifugal Blood Pump with Dual Impeller ad Double Pivot Bearing System: Electromechanical Actuator, Prototyping and Anatomical Studies. Artificial Organs, v.35(5), pp. 437-442, 2011. HRSA – Health Resources and Services Administration – OPTN – Organ Procurement and Transplantation Network – SRTR – Scientific Registry of Transplants Recipient. OPTN/SRTR annual report: Transplant data 1999-2008, 2008 <http://optn.transplant.hrsa.gov/ar2009/> accessed in: 29/08/2011 17h00. JOHNSON, M. R; MEYER, K. H; HAFT, J; KINDER, D; WEBBER, S. A; DYKE, D. B. Heart Transplantation in United States, 1999-2008. American Journal of Transplantation. Wiley Periodicals. v.10(2), pp.1035-1046, 2010. NOSÉ, Y. Design and Development Strategy for the Rotary Blood Pump. Artificial Organs, v.22, pp.438-446, 1998. NOSÉ, Y; KAWAHITO, K. Development of a non-pulsatile permanent rotary blood pump. European Journal of Cardio-thoracic Surgery. v.11, pp. S32-S38, 1997. Secretary of Health Surveillance – Brazilian Ministry of Health. An analysis of the death tares in Brazil and regions, 2004. WHO – World Health Organization. World Health Statistics 2008. World Health Organization, 2008.
Download