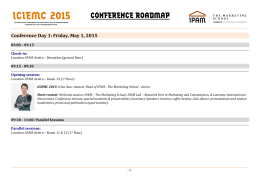
QOPNA Departamento de Química Universidade de Aveiro BOOK OF ABSTRACTS rd 3 WORKSHOP OF IMMUNOLOGY th 20 MAY 2015 – UNIVERSITY OF AVEIRO PROGRAM 13:45 Registration 14:15 Bruno Neves, QOPNA UA Vacinas de Células Dendríticas no combate ao cancro: estado atual e perspetivas futuras 14:45 Alexandre Salvador, ENZIfarma S.A. Resposta imunológica monitorizada por citometria de fluxo 15:15 Virgínia Carvalhais, CBE UM Immunoproteomics to identify Proteins involved in Host-Pathogen Interaction: Example of Staphylococcus epidermidis Biofilms 15:30 Elisabete Maciel, QOPNA UA Oxidized phosphatidylserine downregulate inflammatory signals in macrophages 15:45 Ana Campos, QOPNA UA and Cell 2B. Lipidomics of Mesenchymal Stromal Cells, powerful immunosuppressive agents 16:15 Coffee break funded by Reagente 5 16:45 Andreia Monteiro, FCS UBI O linfócito T na Esclerose Múltipla 17:15 João Martins, CNC UC Dendritic cells surrogates for chemicals’ allergenecity screenning 17:30 Marta Duque, QOPNA UA The Immunosuppresive Potential of Human Amniotic Membrane Extract 17:45 Luciele Minuzzi, FCDEF UC Estudo da senescência em células T reguladoras de desportistas seniores 18:15 Closing ceremony ORGANIZING COMMITTEE Rosário Domingues Pedro Domingues Elisabete Maciel Cláudia Simões Ana Reis João Martins Rui Vitorino Núcleo de estudantes de Química Mass Spectrometry Center, QOPNA, Department of Chemistry, University of Aveiro 3rd Workshop of Immunology VACINAS DE CÉLULAS DENDRITICAS NA TERAPIA ANTI TUMORAL: ESTADO ATUAL E PERSPETIVAS FUTURAS NEVES B.M. 1 Faculty of Pharmacy and Centre for Neuroscience and Cell Biology, University of Coimbra 3000-548, Coimbra – Portugal 2 Mass Spectrometry Centre, Department of Chemistry and QOPNA, University of Aveiro, Campus Universitário de Santiago, 3810-193 Aveiro – Portugal E-mail: [email protected] Abstract As células dendríticas (CDs) são células apresentadoras de antigénio com um papel central na interligação entre imunidade inata e adaptativa. Possuem uma capacidade inigualável de modular as respostas imunes, sendo responsáveis quer pela indução de imunidade quer pela manutenção de tolerância a auto antigénios. Por esta razão tornaram-se nas últimas duas décadas alvos preferenciais no desenvolvimento de imunoterapias, nomeadamente nas que se centram no combate ao cancro. Os resultados experimentais extremamente promissores nesta área não foram muitas das vezes acompanhados por similar sucesso na transposição para aplicação clinica. Este facto levou a que se instalasse alguma desconfiança acerca do real valor terapêutico das vacinas anti tumorais baseadas em CDs. No entanto, o aumento do nosso conhecimento acerca da imunobiologia destas células e o estabelecimento das características ótimas para a imunoterapia anti tumoral, permitiram nos últimos anos desenvolver novas abordagens de uma forma muito mais racional. Contrariamente aos primeiros ensaios clínicos que testavam as vacinas de CDs em monoterapia, atualmente estas são combinadas com outros tratamentos, nomeadamente quimioterapia e radioterapia, no intuito de se obter um efeito sinergístico. Em termos de desenvolvimento muito está ainda por fazer, no entanto novas abordagens como por exemplo o direcionamento in vivo e o uso de implantes com capacidade para recrutar, carregar e maturar as CDs, afiguram-se como tecnologias bastante promissoras que irão num futuro próximo afirmar-se como armas efetivas no combate ao cancro. Aveiro | 20th May 2015 3rd Workshop of Immunology RESPOSTA IMUNOLÓGICA MONITORIZADA POR CITOMETRIA DE FLUXO Salvador A. 1,2 1 Enzifarma S.A 2 ESTES-L E-mail: [email protected] Abstract Sendo a citometria de fluxo uma metodologia que permite a análise individual e individualizada de células em suspensão, rapidamente se percebeu a utilidade da mesma, na interpretação do papel de cada célula no contexto do órgão e do individuo. Assim, cada célula tem interações com as demais células e neste contexto, a forma como recebe informação ou estimulo, desencadeia em si uma resposta. Esta resposta vai condicionar, moldar ou potenciar a resposta de outras células. Disto o sistema imunológico é um bom exemplo. Normalmente podemos estimular as células do sistema imunológico “in vitro” de forma a verificarmos a capacidade de resposta a um estímulo. Com a simples estimulação com Ionomicina ou PMA, podemos verificar a capacidade de resposta de um determinado individuo e comparar com a resposta “normal”. Com a citometria de fluxo, podemos identificar o tipo de interleucina ou citoquina que cada célula está a produzir. Também com a citometria, se pretendermos, podemos quantificar as citocinas que são libertadas para o meio extra-celular. Sabendo que, as citocinas ou interleucinas ao serem libertadas, vão produzir um efeito ao se ligarem a recetores celulares específicos, podemos ainda usar a citometria para responder às perguntas: que citocina estimula cada célula? Que quantidades de citocina são necessárias? O estímulo é específico, ou existem mais células que respondem ao mesmo estímulo? Até hoje, e por limitações destas metodologias, como sensibilidade e reprodutibilidade, a quantificação de uma proteína por célula era apenas possível por outras técnicas. Hoje em dia podemos dizer que estimulo sofreu, de que célula se trata e ainda dizer qualitativamente ou de forma quantitativa a(s) proteína(s) que tiverem intervenção no processo de sinalização celular. Com o objetivo de verificar a resposta imunológica, pretendemos com a citometria de fluxo, identificar as células que participam nessa resposta, que citocinas ou interleucinas são secretadas e com que células interagem. Será que a resposta imunológica ou a sua intensidade é dependente de todo este processo? A metodologia está ai! Os reagentes e protocolos estão disponíveis! Será apenas necessário obter amostras e ter imaginação! O espirito científico, aliado à nossa curiosidade e necessidade de compreensão dos processos biológicos leva-nos a crer que a citometria é uma das melhores formas para compreender a resposta imunológica. Aveiro | 20th May 2015 3rd Workshop of Immunology IMMUNOPROTEOMICS TO IDENTIFY PROTEINS INVOLVED IN HOSTPATHOGEN INTERACTION: EXAMPLE OF Staphylococcus epidermidis BIOFILMS CARVALHAIS V1,2, CERVEIRA F3, VILANOVA M4, CERCA N2, VITORINO R1,5 1 QOPNA, Mass Spectrometry Center, Department of Chemistry, University of Aveiro, 3810-193, Aveiro, Portugal 2 CEB - Centre of Biological Engineering, LIBRO - Laboratory of Research in Biofilms Rosário Oliveira, University of Minho, Campus de Gualtar, 4710-057, Braga, Portugal 3 Anatomia Patológica, Centro Hospitalar Baixo-Vouga, Avenida Artur Ravara, 3814-501 Aveiro, Portugal. 4 Laboratory of Immunology, Department of Immuno-Physiology and Pharmacology, Institute of Biomedical Sciences Abel Salazar (ICBAS), University of Porto, 4050-313 Porto, Portugal 5 iBiMED, Institute for Biomedical Research, University of Aveiro, Aveiro, Portugal E-mail: [email protected] Abstract Immunoproteomics allows the identification of immunogenic and immunoreactive proteins that may participate in host-pathogen interactions and in the host immune response [1]. Therefore, immunoproteomics improves the understanding of infection pathogenesis and unravels novel therapeutic targets based on the repertoire of immunogens [2,3]. Here, we intended to identify immunogenic proteins of Staphylococcus epidermidis biofilms associated with dormancy condition. For that, we separated whole proteins from S. epidermidis biofilms with induced and prevented dormancy using two-dimensional electrophoresis (2-DE). Then, immunoblotting was performed with human sera and proteins were identified by mass spectrometry (MS). A total of 19 bacterial proteins recognized by human serum samples were identified. Differences in the reactivity pattern were found between biofilms with prevented and induced dormancy. CodY and GpmA proteins were reactive to sera only when biofilm dormancy was induced, while FtnA and ClpP were only reactive when dormancy was prevented. Further evaluation of these proteins can provide insights into the mechanisms related to dormancy and help to improve current understanding on how dormancy affects the host immune response. These proteins may represent promising candidates as biofilm markers allowing discrimination of physiological condition displayed by biofilm bacteria and will be worth to consider in further studies. References [1] Fulton, KM. et al. Immunoproteomics: current technology and applications. Methods Mol. Biol. 2013, 1061, 21 [2] Dennehy, R. et al. Immunoproteomics: the key to discovery of new vaccine antigens against bacterial respiratory infections. Curr Protein Pept Sci., 2012, 13, 807 [3] Fulton, KM. et al. Methods and applications of serological proteome analysis. Methods Mol. Biol. 2013, 1061, 97 Aveiro | 20th May 2015 3rd Workshop of Immunology OXIDIZED PHOSPHATIDYLSERINE SIGNALS IN MACROPHAGES DOWNREGULATE INFLAMMATORY MACIEL E.1, MARTINS J.D.2, NEVES B.M. 1, CRUZ M.T. 2, DOMINGUES P. 1, DOMINGUES M.R1 1 Mass Spectrometry Centre, Chemistry Department, University of Aveiro, 3810-193 Aveiro, Portugal Faculty of Pharmacy and Center for Neuroscience and Cell Biology (CNC), University of Coimbra, 3000-548 Coimbra, Portugal E-mail: [email protected] 2 Abstract In the last years phosphatidylserine (PS) has been the focus of many studies and some antiinflammatory properties were attributed to this phospholipid. The development of analytical methods for lipid hydroperoxides has revealed the important role of oxidized PS (oxPS) during apoptosis as well as the novel roles of oxPS under pathophysiological conditions [1]. The present work aimed to clarify whether PS and oxPS differentially modulate the functional responses of macrophages by evaluating the influence of oxPS on the macrophages inflammatory status. Thus, we determined the effects of oxidized 1-palmitoyl-2-linoleoyl-phosphatidylserine (oxPLPS) and PLPS on the RAW 264.7 macrophages production of the pro-inflammatory mediator nitric oxide (NO) and on the levels of the inducible NO synthase (Nos2) and Il1 mRNA. The ability of PLPS and oxPLPS to modulate the lipopolysaccharide (LPS)-triggered macrophage activation was also analyzed. Finally, the effects of PLPS species over canonical inflammation-associated signaling pathways, such as nuclear factor (NF)-ĸB and mitogen-activated protein kinases (MAPKs) were also disclosed. The results obtained showed that both PLPS and oxPLPS species are deprived of intrinsic proinflammatory activity. However, only oxPLPS were found to significantly inhibit NO production and iNos and IL1β genes transcription induced by LPS. At a molecular level, these effects were partially due to attenuation of LPS-induced c-Jun-N-terminal kinase (JNK) phosphorylation and p65 NF-ĸB nuclear translocation. Overall our data suggest that oxPLPS, but not native PLPS, mitigates proinflammatory signaling in macrophages, contributing to containment of inflammation during apoptotic cell engulfment. References [1] Matsura T. Oxidized Phosphatidylserine: Production and Bioactivities. Yonago Acta medica 2014;57:119–127. Aveiro | 20th May 2015 3rd Workshop of Immunology LIPIDOMICS OF MESENCHYMAL IMUNOSSUPRESSIVE AGENTS STROMAL CELLS, POWERFUL CAMPOS A.1, MACIEL E.1, MOREIRA A.1, MELO T.1, DOMINGUES P.1, DOMINGUES M.1, SANTOS F.2, CURADO L.2, ANTUNES B.2 1 Mass Spectrometry Centre, QOPNA, Department of Chemistry, University of Aveiro, 3810-193 Aveiro, Portugal 2 Cell2B Advanced Therapeutics SA, Biocant Park Núcleo 04 Lote 4 A, 3060-197 Cantanhede, Portugal E-mail: [email protected] Abstract In the last years, mesenchymal stromal cells (MSCs) have been successfully applied in many clinical trials (1). MSCs are primitive cells with origin in the mesodermal germ layer. They are considered adult stem cells, once these cells are characterized as capable of self-renewal and directed differentiation (1). MSCs have drawn the interest of researchers and they have been used as a biologic therapeutic for several clinical applications (1). In fact, MSCs interfere with immune cells and inhibit the proliferation of activated allogeneic lymphocytes either in vitro as in vivo, crossing histocompability barriers. MSCs also act upon most major components of the innate and adaptive immune system and they show proangiogenic, cytoprotective and antifibrotic effects. In addition, MSCs have proven capable of migrating towards tissues experiencing inflammatory events (2). For these reasons, most recently there has been a rising interest in applying these cells as a treatment for inflammatory and autoimmune diseases (2), such as Graft versus Host Disease (GvHD), multiple sclerosis and Crohn’s disease (CD). However, despite the wide use of these cells in clinical trials the mechanisms employed by these cells are not totally understood. Further and more extensive applications of MSCs in other inflammatory and autoimmune diseases require a deeper knowledge about their behaviour, phenotypic characteristics and mechanisms. Lipidomics approach can provide some of the needed information. Lipidomics refers to ‘the systems-level analysis of lipids and their interacting moieties’. There has been an increasing interest in Lipidomics once each lipid class has specific functions and take part in different metabolic and signalling processes. Moreover, it is know accepted lipids trigger immune responses. So it becomes important to analyse differences of specific lipid species in different pathways. Only a few and very recent studies around MSCs’ lipidomics have been conducted. However, none of them analysed differences in MSCs’ phospholipid profile between MSCs subjected to proinflammatory stimulus and non-stimulated MSCs. In this study, we cultured MSCs both in a standard culture medium and in a culture medium supplemented with pro-inflammatory stimulus, namely TNF- and IFN-. Then we analysed differences in the phospholipid profile of MSCs from both conditions, in order to understand which phospholipid molecular species take part in MSCs’ immunosuppressive mechanism. References [1] Salem HK, Thiemermann C. Mesenchymal Stromal Cells : Current Understanding and Clinical Status. Stem Cells. 2010;28(3):585–96. [2] Griffin MD, Elliman SJ, Cahill E, English K, Ceredig R, Ritter T. Concise Review : Adult Mesenchymal Stromal Cell Therapy for Inflammatory Diseases : How Well Are We Joining the Dots ? Stem Cells. 2013;31(10):2033–41. Aveiro | 20th May 2015 3rd Workshop of Immunology THE T CELL IN MULTIPLE SCLEROSIS MONTEIRO A. 1, CRUTO C.2, ROSADO P.2, FONSECA M.1, ROSADO L.2, CARVALHEIRO T. 3, PAIVA A. 3 1 Faculdade Ciências da Saúde-Centro de Investigação em Ciências da Saúde, Universidade da Beira Interior, Covilhã 2 Serviço Neurologia, Centro Hospitalar Cova da Beira, Covilhã 3 Laboratório citometria de fluxo, Instituto Português do Sangue e da Transplantação, Coimbra, Portugal E-mail: [email protected] Abstract Multiple sclerosis (MS) is a complex autoimmune demyelinating disease of the central nervous system (CNS) of unknown etiology. MS is characterized by CNS inflammation, demyelination, axonal injury and axonal loss. Autoreactive T cells activated outside the CNS cross the blood-brain barrier and are reactivated by local antigen-presenting cells. Secretion of proinflammatory cytokines stimulates microglial cells and astrocytes, recruits additional inflammatory cells, and induces antibody production by plasma cells. This inflammatory process finally leads to tissue damage within the plaque. It is generally accepted that myelin-specific Th cells play a central role in initiating and orchestrating CNS inflammation in MS. Initially, Th1 cells where considered the subset responsible for the MS pathogenesis, although others subsets has been shown to be also involved in this process, like Th17, regulatory Th (Treg) and γσT cells. Considerable evidence exist that points toward an important pathogenic and/or regulatory role for cytotoxic CD8 T cells(Tc) in MS. In this context, the aim of the present work was to quantify and functional characterize Th(c)1, Th(c)17, Treg and γσT cells populations in the peripheral blood from patients diagnosed with MS, according to the MacDonald criteria 2010. 38 patients, subdivided in 2 subgroups, according to the phase of the disease, stable (n=30, 26 female/ 4 male, mean age 41±15) or relapse (n=8, 5 female/ 3male, mean age 44±11) and a control group (n=20, 16female/4male, mean age 50±9) were evaluated in this study. Th(c)1, Th(c)17 and Tγσ cells characterization was done by intracellular cytokine staining after in vitro stimulation with PMA/ionomycin, in the presence of Brefeldin A during 4 hours. The expression of cell surface markers and intracellular production of IL-17, TNFα, IFNγ and IL-2 were assessed by flow cytometry (FACSCanto; BD), and the obtained results were analyzed using Infinicyt software (Cytognos). Statistical evaluation of data were analysed using the non-parametric Mann-Whitney U test. We observed a significant increase in the frequency of Th17 cells in stable MS group when compared with relapse or control groups. Moreover, an increased expression of TNFα was observed in those cells. The frequency of Tc17cells, and among them, those that concomitant produced IL-17 and IFN-γ were also increased in stable MS, as well as TNFα expression. A same pattern was observed in relapse MS when compared with control group. Concerning the frequency of Th1, Tc1 and Treg cells no statistically significant differences were observed between the studied groups. In the stable group of patients with RRMS naive γσT were increased when compared with control group. The patients in relapse phase only exhibit statistically significant differences when compared with stable group, namely a decreased in effector γσT subset and an increase in the frequency of γσT producing IFNγ. In summary, it seems that Th17, Tc17 and γσT cells could play an important role in the pathophysiology of MS, since increased frequencies of those cells were observed in MS patients. We also may speculate that the decreased frequencies of those cells observed in relapse patients could reflect a specific migration from blood to CNS. We believe that a more comprehensive knowledge of the plasticity of these cells in MS is highly pertinent for future therapeutic interventions. References [1] Kamm CP, Uitdehaag BM, Polman CH. Multiple Sclerosis: Current Knowledge and Future Outlook. Eur Neurol. 2014;72:132–41. [2] Raphael I, Nalawade S, Eagar TN, Forsthuber TG. Cytokine T cell subsets and their signature cytokines in autoimmune and inflammatory diseases. Cytokine. Elsevier Ltd; 2014; [3] Maddur MS, Miossec P, Kaveri S V., Bayry J. Th17 cells: Biology, pathogenesis of autoimmune and inflammatory diseases, and therapeutic strategies. Am J Pathol. 2012;181(1):8–18. Aveiro | 20th May 2015 3rd Workshop of Immunology DENDRITIC CELLS SCREENING SURROGATES FOR CHEMICALS’ ALLERGENICITY MARTINS J. D. 1,2, SILVA A. 2, MACIEL E. A. 3, FERREIRA I. 2, DOMINGUES P. 3, NEVES B. M. 1,3, DOMINGUES M. R. M. 3, CRUZ M. T. 1,2 1 Faculty of Pharmacy University of Coimbra, 3000-548 Coimbra, Portugal for Neuroscience and Cell Biology (CNC), University of Coimbra, 3004-517 Coimbra, Portugal 3 Mass Spectrometry Centre, Chemistry Department, University of Aveiro, 3810-193 Aveiro, Portugal E-mail: [email protected] 2 Center Abstract Dermal and inhalation toxicity are important toxicological endpoints that should be determined to all chemicals for which human exposure is foreseeable. European Union legislations such as REACH (Registration, Evaluation, Authorisation and Restriction of Chemicals; EC nº 1907/2006) and the cosmetics regulation (EC nº 1223/2009) have reinforced that obligation and strongly encouraged the reduction/avoidance of animals’ use in toxicity tests. Allergic contact dermatitis and respiratory allergies caused by low molecular weight electrophilic reactive chemicals are particular cases of dermal and inhalation toxic reactions, respectively. The complexity of these adaptive immune reactions hinders the in vitro determination of chemicals’ propensity to trigger such reactions. One promising strategy towards the development non-animal alternative approaches relies on the utilization of in vitro models based on dendritic cells (DC) surrogates. In such models, the crucial role played by DC in the orchestration of T-cell mediated immune responses is used as a premise to predict the allergenic potential of chemicals. In our presentation we will briefly highlight the common and unique immune features involved in contact and respiratory allergies triggered by chemicals and shortly review the utilization of ‘DC like’ cells in toxicological predictive tests for skin and airway sensitization. We will also present some of the results obtained in our lab with the DC-like cell line THP-1, a dendritic cell surrogate thoroughly used in the above mentioned toxicity tests. Funding This work is funded by The Johns Hopkins Center for Alternatives to Animal Testing [2014-07], by FEDER funds through the Operational Programme Competitiveness Factors - COMPETE and Quadro de Referência Estratégico Nacional, and by national funds by FCT -Foundation for Science and Technology under the projects QREN – Empresas em co-promoção project ref: 38977, PEstC/SAU/LA0001/2013 and strategic projects UID / NEU / 04539 / 2013, REDE/1504/REM/2005 (that concerns the Portuguese Mass Spectrometry Network), and the projects PEst-C/QUI/UI0062/2013 and FCOMP-01-0124-FEDER-037296 (that concern QOPNA research unit), and the fellowships SFRH/BD/73065/2010 and SFRH/BPD/104165/2014. Aveiro | 20th May 2015 3rd Workshop of Immunology THE IMMUNOSUPPRESIVE POTENTIAL OF HUMAN AMNIOTIC MEMBRANE EXTRACT DUQUE M.1, JESUS M.2, SILVA I2, MAMEDE AC3,4,5,6, LARANJO M3,5,6, CARVALHO MJ3,5,6,7, MOURA P7, ABRANTES AM 3,5,6, MAIA CJ4, ROSÁRIO D.1, BOTELHO MF3,5,6. TRINDADE H2, PAIVA A.2 1Department of Chemistry, University of Aveiro, Aveiro, Portugal and Transplantation Center of Coimbra, Portuguese Institute of the Blood and Transplantation, Coimbra, Portugal 3Biophysics Unit, Faculty of Medicine, University of Coimbra, Coimbra, Portugal 4CICS-UBI, Health Sciences Research Center, University of Beira Interior, Covilhã, Portugal 5CIMAGO, Faculty of Medicine, University of Coimbra, Coimbra, Portugal 6CNC-IBILI, Faculty of Medicine, University of Coimbra, Coimbra, Portugal 7Obstetrics Service, Coimbra Hospital and University Center, Coimbra, Portugal E-mail: [email protected] 2Blood Abstract Introduction: The human amniotic membrane (hAM) is thought to possess an active immunosuppressive mechanism responsible for its ability to inhibit innate and adaptive immune responses, including T cell proliferation and cytokine production. Several hAM-derived factors, potentially responsible, have already been identified but the exact underlying mechanism of action is yet unknown. Furthermore, there is little information regarding the exact influence over individual T cell subpopulations. Thus the proposed objective was to evaluate the influence of hAM extract over the production of different inflammatory cytokines by different T helper (Th or CD4) and T cytotoxic (Tc or CD8) cell subsets. Methods: Peripheral blood mononuclear cells (MNC) were cultured during 24 hours, with or without (negative control) the addition of hAM extract to the culture medium, and then stimulated with phorbol 12-myristate 13-acetate (PMA) for the analysis of intracellular cytokine production by flow cytometry. The frequency of IL-2, IL-9 IL-17, TNFα and IFNγ-producing Th (CD3+CD4+CD8-) and Tc (CD3+CD4CD8+) cells were determined among naïve (CD45RA+CD27+), CM (CD45RA-CD27+), EM (CD45RACD27-) and effector (CD45RA+CD27-) T cell compartments. Evaluation of cell proliferation was performed after mitogen stimulation, through thymidine incorporation assay, either in presence or absence of extract. Results: Overall, T cells showed lower frequencies of cytokine producing cells in the presence of hAM extract. The percentage of inhibition varied according to the cytokine understudy and T cell compartment, still, significant inhibition was observed for all cytokine-producing cells, with the possible exception of IFNγ-producing CD8 T effector cells. For the most part, the percent inhibition was very similar between CD4 and CD8 cells, however, CD4 TNFα- and IFNγ-producing cells were clearly more susceptible to inhibition than the CD8 cells. On the other hand, a strong inhibitory effect over cell proliferation was observed for PHA-stimulated cells, being slightly lower for PWM and absent for SpAstimulated cells. Additionally, the same pattern of experiments were performed with amniotic membrane derived cells, in a ratio MNC-to-hAM cells of 10:1 and 2:1, although a significant reduction in the frequency of cytokine producing cells was only observed for IL-2 producing CD4 and CD8 T cells. Conclusions: hAM extract exhibits a strong potential to suppress T cell activation and proliferation. On the other hand, hAM cells do not exert the same effect, which could be due, at least in part, to the lower frequency of mesenchymal stromal cells detected in cells suspensions from amniotic membrane. Aveiro | 20th May 2015 3rd Workshop of Immunology ACUTE EXERCISE EFFECTS ON TREG CELLS IN MASTER ATHLETES MINUZZI L.1, RAMA L.1, ROSADO F.1, PEREIRA S.2, SILVA I.2, INACIO M.2, PAIVA A.2, TEIXEIRA A.1 1 Faculty of Sport Sciences and Physical Education, University of Coimbra, Coimbra, PORTUGAL Portuguese Institute for Blood and Transplantation, São Martinho do Bispo, Coimbra, PORTUGAL [email protected] 2 Abstract Human aging is associated with a progressive decline in immune function. Among these changes are alterations in T-cell subpopulations size, cytokine secretion pattern, cell replicative capacity and antibody production, all of which culminate in a pro-inflammatory state and diminished capacity to respond to new antigens, alterations are closely related to the increased mortality and morbidity rates observed in this population (1). A feature of immunosenescence is the change in the cellular composition of the T-cell compartment, including a decrease in the number of naïve T cells and an increase in the number of memory T cells. T-cells that have reached terminal differentiation are known to have overly eroded and critically short telomeres (2). These erode progressively with each round of cell division as in T-cell clonal expansion as in response to persistent viral infections. Excessive telomere erosion triggers mechanistic pathways for senescence causing the cell to undergo proliferative arrest. Elderly individuals are known to have shorter leukocyte telomeres than their younger counterparts (3). However, analysis of human peripheral blood after exercise has revealed an increase in regulatory T cells (Tregs) (4). These are CD4+CD25+ cells that express the transcription factor FOXP3, the main function appearing to be the downregulation of adaptative immune responses (5) and the minimization of inflammation-induced tissue damage. Studies have shown that antigen stimulated IL-10 production highest in the athletes with the higher training loads (6). In trained rats, high intensity exercise resulted in increased numbers of regulatory T cells, and was also associated an increased expression of anti-inflammatory cytokines (7). These results imply that high intensity exercise training may be more beneficial than moderate training in reducing risk of cardiovascular and metabolic chronic diseases as a result of its anti-inflammatory effects (8). Studying immunosenescence by looking at master athletes, a population characterized by a longlife exposure to exercise, could prove to be a valuable tool in understanding how exercise could improve life expectancy. Preliminary results will be show about responses of Tregs and KLRG1 expression, a marker associated a T cell activation and senescence (9), in naïve and memory Tregs to exercise in master athletes. References [1] de Araujo AL. et al. Preventing or reversing immunosenescence: can exercise be an immunotherapy? Immunotherapy. 2013, 5, 8. [2] Simpson RJ. et al. Senescent T-lymphocytes are mobilised into the peripheral blood compartment in young and older humans after exhaustive exercise. Brain Behav Immun. 2008, 22, 4. [3] Andrews NP. et al. Telomeres and immunological diseases of aging. Gerontology. 2010, 56, 4. [4] Yeh SH. et al. Regular tai chi chuan exercise enhances functional mobility and CD4CD25 regulatory T cells. Br J Sports Med. 2006, 40, 3. [5] Maynard CL. et al. Diversity in the contribution of interleukin-10 to T-cell-mediated immune regulation. Immunol Rev. 2008, 226. [6] Gleeson M. et al. Respiratory infection risk in athletes: association with antigen-stimulated IL-10 production and salivary IgA secretion. Scand J Med Sci Sports. 2012, 22, 3. [7] Wang J. et al. Effect of exercise training intensity on murine T-regulatory cells and vaccination response. Scand J Med Sci Sports. 2012, 22, 5. [8] Gleeson M. et al. The anti-inflammatory effects of exercise: mechanisms and implications for the prevention and treatment of disease. Nat Rev Immunol. 2011;11(9):607-15. [9] Voehringer D. et al. Viral infections induce abundant numbers of senescent CD8 T cells. J Immunol. 2001, 167, 9. Aveiro | 20th May 2015 3rd Workshop of Immunology NOTES Aveiro | 20th May 2015
Baixar