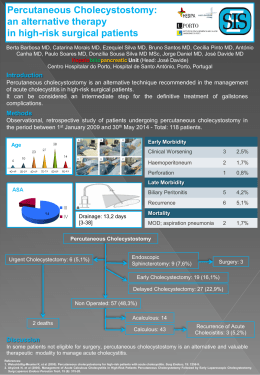
278 Neto PP, Kihara EN, Fontoura EAF, Andrioli MS, Andrade Junior A, Romaldini H, Nóbrega JL ORIGINAL ARTICLE Percutaneous vertebroplasty with polymethylmethacrylate Analysis and results in 57 treated patients Vertebroplastia percutânea com polimetilmetacrilato Análise e resultados de 57 pacientes tratados Pascoal Passarelli Neto1, Eduardo Noda Kihara2, Emilio Afonso França Fontoura3, Mario Sergio Andrioli4, Ary de Andrade Junior5, Helio Romaldini6, João Luiz Nóbrega7 ABSTRACT Objective: The aim of this study is to show percutaneous vertebroplasty as a safe procedure for pain management in diseases such as osteoporosis, benign and malignant spinal tumors, whether primary or secondary, by relieving localized pain and strengthening vertebral body structure. Methods: Percutaneous injection of polymethylmethacrylate under high-resolution fluoroscopy, inside the fractured vertebral body, rebuilding and stabilizing its structure with little sedation and local anesthesia. Results: Ninety-five percent of patients felt immediate pain relief and recovered movement and walking. We verified that only one patient presented mild and transient respiratory insufficiency, probably due to microembolism. No other complications were observed. Three patients returned for another vertebroplasty in vertebral bodies close to those previously treated. Conclusion: Percutaneous vertebroplasty is a safe and efficient procedure in pain and immobility management associated with vertebral compression – fractures that require much pain relief and stability. Injeção percutânea de polimetilmetacrilato, sob visão fluoroscópica de alta resolução, dentro do corpo vertebral fraturado, refazendo sua estrutura de sustentação, ou seja, recuperando sua função, com leve sedação e anestesia local. Resultados: Em 93% dos pacientes houve alívio imediato da dor com recuperação da movimentação e da própria deambulação. Constatamos um único caso de insuficiência respiratória leve e transitória, provavelmente conseqüente à microembolia. Não houve outras complicações. Três pacientes retornaram para nova vertebroplastia em corpos vertebrais vizinhos aos anteriores, devido a novas fraturas; os demais pacientes permaneceram estáveis em acompanhamento ambulatorial sem apresentar novos colapsos vertebrais. Conclusão: Vertebroplastia percutânea é um procedimento seguro e eficiente no tratamento da dor e da imobilidade associadas à fratura da coluna vertebral; visa acabar com a dor e a instabilidade dos fragmentos intracorpóreos. Descritores: Osteoporose; Vertebroplastia; Fratura de corpo vertebral Keywords: Osteoporosis; Vertebroplasty; Vertebral fracture RESUMO Objetivo: Mostrar uma nova técnica de tratamento percutâneo para ablação da dor devido a fraturas ocasionadas por doenças como a osteoporose, tumores benignos e malignos primários e secundários da coluna vertebral, eliminando o quadro álgico localizado e reforçando a estrutura óssea intracorpórea. Métodos: INTRODUCTION Percutaneous vertebroplasty consists of injecting polymethylmethacrylate (PMMA), an acrylic cement, through a needle in the interior of a fractured vertebral body to manage pain and strengthen its bone structure. Pain related to fracture by vertebral body compression affects from 700,000 to 1 million Radiology and Intervention Neuroradiology Service - Hospital Albert Einstein - São Paulo - 2004. 1 Neurosurgeon. Full Member of the Sociedade Brasileira de Neurocirurgia and Effective Member of the European Federation of Spine Surgery. 2 Neuroradiologist at the Intervention Neuroradiology Service of the Hospital Israelita Albert Einstein. 3 Neurosurgeon. Head of the Neurosurgery Service at Complexo Hospitalar do Mandaqui. 4 Neurosurgeon and Neuroradiologist of the Hospital Israelita Albert Einstein. 5 Internal Medicine specialist and Cardiologist. Coordinator of the course Physical Therapy in Internal Medicine at UNIFESP- Escola Paulista de Medicina. 6 Chest physician. Adjunct Professor at UNIFESP - Escola Paulista de Medicina. 7 Rheumatologist, Internal Medicine specialist and Intensivist. Corresponding author: Pascoal Passarelli Neto - Av. Albert Einstein, 627 - 10º andar - sala 1013. CEP 05651-901 - São Paulo (SP), Brazil - e-mail: [email protected] Received on April 15, 2004 – Accepted on August 20, 2004 einstein. 2004; 2(4):278-81 Percutaneous vertebroplasty with polymethylmethacrylate Analysis and results in 57 patients treated individuals per year in the U.S.(1) and its major cause is osteoporosis. Primary osteoporosis caused by demineralization and resulting in age-related bone loss accounts for approximately 85% of vertebral compression fracture and affects roughly 200 million women aged over 50 years. Secondary osteoporosis observed in patients taking steroids, anticonvulsants, chemotherapeutic agents and heparin, as well as in vertebral tumors, accounts for 15% of vertebral compression fractures. Approximately 20-30% of patients with vertebral compression fracture observed in plain radiographs present restricted daily activities and pain intensity 3 and 4, according to the verbal scale (VS) - McGill-Melzack scoring system(2) (table 1). Table 1. Verbal scale - McGill-Melzack Scoring System 0-6 0 1 2 3 4 5 - No pain Mild pain Troublesome pain Severe pain Very severe pain Excruciating pain The traditional treatment for vertebral compression fracture is analgesic medication, bed rest and bracing. Surgical treatment is performed in cases of neurological deficit related to compression of the nerve root or spinal cord(3). Approximately one third of patients with vertebral compression fracture do not respond to conservative treatments, resulting in prolonged inactive periods and increased bone mass loss with higher risk of new fractures(4). In 1987, Galibert et al.(5) were the pioneers in using acrylic cement in a C2 vertebral body with hemangioma, in a 50-year patient who suffered from cervical pain. This study aimed to assess the results of treating vertebral body compression fractures in osteoporotic patients by means of percutaneous injection of polymethylmethacrylate. METHODS Fifty-seven patients aged 60-89 years, 8 males and 49 females, were treated from January 2001 to July 2004. A total of 118 fractured vertebral bodies were treated, 62 lumbar and 56 thoracic vertebrae, most of them located close to the thoracolumbar transition. (Table 2) After clinical assessment and magnetic resonance imaging (MRI) study, the patients were submitted to 279 vertebroplasty under high-resolution fluoroscopic guidance and ensuring maximum asepsis. Thoracic vertebroplasties were performed with patients in prone position, whereas in lumbar procedures, patients were in lateral decubitus or prone position. For unilateral or bilateral transpedicular approach of the vertebral body we used 13G to 18G needles. The mean volume of PMMA mixed with to barium sulfate was 2-3 ml per vertebral body; it was injected at several levels, taking care for PMMA not reaching the posterior wall. Phlebography is performed before injecting acrylic cement to determine localization and venous drainage. Patients were treated under mild sedation, local anesthesia and prophylactic antibiotic therapy. After injection, they remained in decubitus for 20 minutes for safety reasons. Figures 1 and 2 show the results of PMMA injection. RESULTS No patient in our series developed neurological deficit simultaneously with or after PMMA injection. One patient presented another fracture of the vertebral body six months after a vertebroplasty performed with a 13-G-needle by unilateral transpedicular approach. The patient was submitted to another procedure with resolution of pain. Immediate clinical improvement was observed in 54 patients (112 vertebrae), and three patients (6 vertebrae) returned for another vertebroplasty in close vertebral bodies. One patient had mild transient respiratory failure probably due to migration of material (microembolism?) but had no sequela. Fifty-four patients presented total resolution of pain in the follow-up. DISCUSSION Approximately 95% of patients had significant improvement of pain and strengthening of the vertebral body. All individuals recovered mobility due to pain relief. The literature reports only 1% of complications, and the most often observed are radicular pain by nerve root compression, discitis, osteomyelitis, spinal infection, spinal compression and pulmonary embolism(6-9). Several retrospective and prospective studies tried to explain improvement in painful symptoms(10-11). The possible mechanisms involved in relief of pain include Table 2 - Number of patients and sex distribution. Number of treated vertebrae and causes of fractures Patients Female Male Total number of vertebrae Lumbar vertebrae Thoracic vertebrae Fractures Osteoporosis Fractures Tumor Improvement 57 49 8 118 62 56 85% 15% 95% einstein. 2004; 2(4):278-81 280 Neto PP, Kihara EN, Fontoura EAF, Andrioli MS, Andrade Junior A, Romaldini H, Nóbrega JL Figure 1. Results of PMMA injection. Figure 2. Results of PMMA injection. thermal and chemical reactions and mechanical factors, such as stabilization after acrylic cement injection(12-13). Exothermal polymerization reaction releasing heat occurs in the transition from paste form to solid state, in solidification of PMMA. This heat release may be the cause of pain relief(10), but recent studies do not support this theory due to the small amount of PMMA used(14). The chemical reaction by the presence of methylmetacrylate cannot be proved until concentration measurements of this material be performed in vivo(12). Mechanical stability after PMMA injection reduces movement and nerve stimuli of pain receptors located in the periosteum, and may be the major cause of pain relief. Today we standardize the procedure according to the level involved. For thoracic vertebra, we systematically perform bilateral transpedicular approach, whereas for lumbar fractures, we preferentially use a posterior-lateral approach, with intravertebral injection and pedicular approach. In some cases we observed failures related to re-fractures are more likely in the area with acrylic cement. In our opinion this is due to insufficient injection of material (0.5-1.0 ml), and it is necessary to inject PMMA again in the areas adjacent to that already stable (2.0-4.0 ml). It is possible to simultaneously inject PMMA in several vertebral bodies by means of unilateral or bilateral transpedicular approach. Currently, vertebroplasty may also be used for spinal bone lesions secondary to primary or metastatic tumors(15-16). The literature reports vertebroplasty is indicated to treat vertebrae with hemangioma in the vertebral body(5). There are rare complications (1%)(17). einstein. 2004; 2(4):278-81 CONCLUSION Patients with osteoporosis and pain intensity 3, according to McGill Melzack scale, as well as restricted movements due to vertebral compression fracture could be treated by means of percutaneous vertebroplasty, with acrylic cement injected under high-resolution fluoroscopy guidance, maximum asepsis and sedation. Percutaneous vertebroplasty is an efficient procedure to treat disabling pain that is secondary to fractures related to osteoporosis and primary or secondary/metastatic tumors. Improved painful symptoms initiate after injection of acrylic cement by strengthening the structure and stabilizing the vertebral body, thus recovering its functionality. REFERENCES 1. Melton LJ 3rd. Epidemiology of spinal osteoporosys. Spine. 1997;22(24Suppl):2S-11S. Review. 2. Cortet B, Cotten A, Boutry N, Dewatre F, Flipo RM, Duquesnoy B, et al. Percutaneous vertebroplasty in patients with osteolytic metastases or multiple myeloms. Rev Rhum Engl Ed. 1997;64(3):177-83. 3. Barr JD, Barr MS, Lemley TJ. Percutaneous vertebroplasty for pain relief and spinal stabilization. Spine. 2000; 25(8):923-8. 4. Bostrom MP, Lane JM. Future directions. Augmentation of osteoporotic vertebral bodies. Spine.1997; 22(24Suppl):38S-42S. 5. Galibert P, Deramond H, Rosat P, Le Gars D. Note preliminaire sur le traitement des angiomes vertebraux par vertebroplastie acrylique percutanee. Neurochirurgie. 1987;33(2):166-8. Percutaneous vertebroplasty with polymethylmethacrylate Analysis and results in 57 patients treated 6. Cohen LD. Fractures of osteoporotic spine. Orthop Clin North Am.1990; 21(1):143-50. 7. Cyteval C, Sany J, Sarrabere MP, Roux JO, Thomas E, Jorgensen C et al. Acute osteoporotic vertebral collapse: open study on percutaneous injection of acrylic surgical cement in 20 patients. AJR am J Roentgenol. 1999;173(6):1685-90. 8. Deramond H, Depriester C, Galibert P, Le Gars D. Percutaneous vertebroplasty with PMMA. Technique, indications and results. Radiol Clin North Am.1998; 36(3):533-46. 9. Deramond H, Wright NT, Belkoff SM. Temperature elevation caused by bone cement polymerization during vertebroplaty. Bone.1999; 25(2Suppl):17S-21S. 10. Garfin SR, Yuan HA, Reiley MA. New Technologies in spine: kyphoplasty and vertebroplasty for the treatment of painful osteoporotic compression fractures. Spine. 2001; 26(14):1511-5. 11. Hardouin P, Grados F, Cotton A. Should percutaneous vertebroplasty be used to treat osteoporotic fractures? An update. Joint Bone Spine.2001; 68(3):216-21. 281 12. Heaney RP. The natural history of vertebral osteoporosis. Is low bone mass an epiphenomenon? Bone. 1992;13 Suppl2:S23-6. 13. Heini PF, Walchli B, Berlemann U. Percutaneous transpedicular vertebroplasty with PMMA: operative technique and early result. A prospective study for the treatment of osteoporotic compression fractures. Eur Spine. 2000; 9(5):445-50. 14. Jensen ME, Evans AJ, Kallmes DS, Cloft HJ, Dion JE. Percutaneous PMMA vertebroplasty in the treatment of osteoporotic vertebral body compression fractures: technical aspects. AJNR Am J Neuroradiol. 1997;18(10):1897-904. 15. Mathis JM, Barr JD, Belkoff SM, Barr MS, Jensen ME, Deramond H. Percutaneous vertebroplasty: a developing standard of care for vertebral compression fractures. AJNR Am J Neuroradiol. 2001;22(2):373-81. 16. Ratliff J, Nguyen T, Heiss J. Root spinal cord compression from methylmethacrylate vertebroplasty. Spine. 2001;26(13):AND 300-2. 17. Padovani B, Kasriel O, Brunner P, Peretti-Viton P. Pulmonary embolism caused by acrylic cement: a rare complication of percutaneous vertebroplasty. AJNR Am J Neuroradiol. 1999; 20(3):375-7. einstein. 2004; 2(4):278-81
Baixar