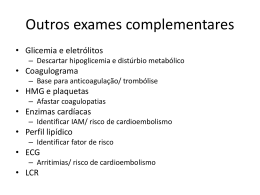
Research Past, present, and future of stroke in middle-income countries: the Brazilian experience Sheila Cristina Ouriques Martins1,2*, Octávio Marques Pontes-Neto3, Cloer Vescia Alves4, Gabriel Rodriguez de Freitas5, Jamary Oliveira Filho6, Elza Dias Tosta7, and Norberto Luiz Cabral8 on behalf of Brazilian Stroke Network Background Stroke is one of the major public health challenges in middle-income countries. Brazil is the world’s sixth largest economy but was clearly behind the milestones in the fight against stroke, which is the leading cause of death and disability in the country. Nevertheless, many initiatives are now reshaping stroke prevention, care, and rehabilitation in the country. Aims The present article discusses the evolution of stroke care in Brazil over the last decade. Methods We describe the main characteristics of stroke care before 2008; a pilot study in a Southern Brazilian city between 2008 and 2010, the Brazilian Stroke Project initiative; and the 2012 National Stroke Policy Act. Results The National Stroke Project was followed by a major increased on the number of stroke center in the country. The key elements of the 2012 National Stroke Policy Act included: definition of the requirements and levels of stroke centers; improved reimbursement for stroke care; promotion of stroke telemedicine; definition of the Line of Stroke Care (to integrate available resources and other health programs); increased funding for stroke rehabilitation; funding for training of healthcare professionals and initiatives to increase awareness about stroke within the population. Conclusions The evolution of stroke care in Brazil over the last decade is a pathway that exemplifies the challenges that middle-income countries have to face in order to improve stroke prevention, treatment and rehabilitation. The reported Brazilian experience can be extrapolated to understand the past, present, and future of stroke care in middle-income countries. Key words: middle-income country, organized stroke care, stroke, stroke management, stroke systems, stroke unit Correspondence: Sheila Cristina Ouriques Martins*, Rua Engenheiro Olavo Nunes, 99/ 703. Bela Vista., Porto Alegre, RS 90440-170, Brazil. E-mail: [email protected] Facebook: www.facebook.com/CampanhaAVC 1 Hospital de Clínicas de Porto Alegre, Porto Alegre, Brazil 2 Hospital Moinhos de Vento, Porto Alegre, Brazil 3 Hospital das Clínicas de Ribeirão Preto, Ribeirão Preto, Brazil 4 General Coordination of Urgency and Emergency, Ministry of Health 2007–2009, Brasília, Brazil 5 D’Or Institute for Research and Education (IDOR), Rio de Janeiro, Brazil 6 Stroke Service, Federal University of Bahia, Salvador, Brazil 7 Hospital de Base do Distrito Federal, Brasília, Brazil 8 Joinville Stroke Register- Univille, Joinville, Brazil Funding: None. Conflict of interest statement: The author declares no potential conflict of interest. DOI: 10.1111/ijs.12062 © 2013 The Authors. International Journal of Stroke © 2013 World Stroke Organization Introduction Brazil is a multiethnic country with almost 200 million people that has been growing at an average annual rate of 1·7% since 1990. In the last two decades, the growing economy and the implementation of major social programs have shifted 50% of population of this middle-income country above the extreme poverty line (1). Recent news also suggests that the Brazilian population is reassessing its battle against stroke, still the country’s number one killer (2). Since the 1988 Brazilian Constitution, which reshaped the country after more than 20 years of military dictatorship, all Brazilians have granted access to the public healthcare system. However, the deep and historical social inequality (one of the most pronounced in the planet) and the growing prevalence of obesity, diabetes, and hypertension are barriers that challenge the national public health agenda (3). Only one fourth of the population can afford the benefits of additional private healthcare insurance (3). As in other middle-income countries, stroke care follows the social disparities that divide Brazil into two different ‘countries’: the more wealthy part that shares the same profile of developed countries and is able pay for high-quality stroke care resources; and the majority of the population that has several limitations to access stroke prevention, acute treatment, and rehabilitation. In this article, our aim is to describe the evolution of stroke care in Brazil over the last decade: the main characteristics of stroke care before 2008; the pilot study in a Southern Brazilian city between 2008 and 2010, which generated the Brazilian Stroke Project; finally, the key points of the 2012 National Stroke Policy Act. We believe that the reported Brazilian experience can be extrapolated to understand the past, present, and future of stroke care in middle-income countries. Stroke care before 2008 The burden of stroke for Brazilian society is huge. Stroke has been the leading cause of death in the last 30 years (4). In 2006, cardiovascular diseases were the third main reason for all national hospital admissions, and in 2007, the World Bank estimated that Brazil lost US$ 2·7 billion of gross domestic product on health care related to cardiac diseases, stroke, and diabetes (4,5). Since 1980, stroke mortality has been decreasing all over the country (6). The 30-day case fatality for all strokes ranged from 20% to 25% in population-based studies (7). The actual trends of stroke incidence in the country are still unknown. One population-based study undertaken in the city of Joinville located Vol ••, •• 2013, ••–•• 1 Research S. C .O. Martins et al. in the more developed southern region of Brazil showed a onethird decrease in incidence of first-ever stroke from 1995 to 2005·(7). Whether those results can be extrapolated to the poorest regions of the country is questionable. In fact, Joinville was the first city of the country to have a stroke unit, which was created by 1997·(8). Intravenous thrombolytic therapy for ischemic stroke was approved in the country in 2001 by the National Agency of Sanitary Vigilance (2). Since then, some academic hospitals started to organize stroke teams and units across the country. Nevertheless, when we consider Brazil’s continental size, the availability of stroke units and access to stroke intravenous thrombolysis were still incipient until 2008. In fact, until June 2008, only 35 stroke centers were active and they were working largely isolated (Fig. 1a). At a national level, programs to control arterial hypertension and diabetes were underpowered and did not focus on adherence for high-risk patients. Therefore, those programs had questionable impact in stroke incidence and mortality. Despite the effort of the Federal Government to provide essential medications for preventive treatment of cardiovascular diseases among patients within the public health system, those resources were irregularly distributed to the population. Important aspects of acute stroke care, secondary prevention, and rehabilitation were still largely neglected (9). Alarming lack of awareness about stroke among the population and also healthcare professionals was the rule (10). Despite several attempts by the Brazilian Academy of Neurology and the Brazilian Stroke Society to mobilize the Federal Government about the problem, there were no concrete actions to improve the hospital provision of care and most of the resources were used to pay for the treatment of complications and disability after stroke (11). Other problems that challenged the implementation of acute stroke care in the country include: overcrowded emergency a b Fig. 1 (a) Distribution of stroke centers before the Brazilian stroke program. (b) Distribution of stroke centers after the Brazilian stroke program. 2 Vol ••, •• 2013, ••–•• © 2013 The Authors. International Journal of Stroke © 2013 World Stroke Organization S. C .O. Martins et al. rooms; the low availability of intensive care unit (ICU) beds; paucity of physicians adequately trained to treat stroke; poor awareness about stroke symptoms in the population; and low availability of recombinant tissue plasminogen activator (rtPA) in the majority of public hospitals (11). The Brazilian Stroke Project: 2008–2010 In June 2008, the Department of Urgency and Emergency Care of the Brazilian Ministry of Health started a project to improve the care of patients with stroke and myocardial infarction, the first and second causes of death in Brazil, respectively. The National Stroke Project included a task force of stroke neurologists who founded the Brazilian Stroke Network, aimed at providing scientific support to the establishment of a nationwide network to improve the education, care, and research about stroke in the country. This nongovernmental organization would soon after expand and incorporate other medical specialties, nurses, nurse assistants, physiotherapists, psychologists, speech therapists, occupational therapists, health authorities, and patients and their caregivers working together to decrease the impact of stroke in Brazil. A task force framed by the Brazilian Stroke Network, the Brazilian Stroke Society, the Brazilian Academy of Neurology, the Research Brazilian Medical Association, the Brazilian Society of Cardiology, and the Brazilian Emergency Network created a National Stroke Project that included five main components: (a) educational campaigns; (b) training emergency medical services; (c) development of stroke centers inside secondary and tertiary hospitals across the country; (d) improvement on prevention of cerebrovascular risk factors in public outpatients’ clinics; (e) implementation of programs for early rehabilitation and family support. The implementation of the National Stroke Project started with the organization of acute stroke care in the country (Table 1). The initial focus was placed on the development of acute stroke centers and training of the components of prehospital, hospital acute care, and transport. The SAMU, which stands for Serviço de Atendimento Móvel de Urgência, is a prehospital emergency medical system in Brazil that covers approximately 70% of the population and can be activated by a free call to a unique nationwide phone number (192) (12). The involvement of SAMU into the stroke care was a decisive step to raise the awareness about stroke among health professionals. Stroke research also contributed to increase awareness about stroke in Brazil (10). An important research landmark was the confirmation of safety and efficacy of thrombolytic therapy for stroke in the Brazilian population by a collaborative effort Table 1 Steps for organization of acute stroke care in Brazil Step 1. Acknowledgment and assess of the situation of stroke assistance in the country 1. Visits to every state to meet with the State Secretary of Health and the City Secretaries, directors of hospitals, chief of the emergency services, coordinator of local prehospital. 2. Assessment of which hospitals were already responsible for the stroke assistance in each main city. 3. Face-to-face visits to every hospital to evaluate physical structure of emergency room, ICU, diagnostic resources, local staff, number of stroke patients assisted, and number of hospital beds. Step 2. Development of the stroke centers After visiting all hospitals, plans for the local networks were established according to the needs and available resources, including suggestion for changes on structure and facilities of the local hospitals, when necessary. Each hospital had to be equipped with an organized emergency room, 24 h laboratory and CT scanner, ICU, and a stroke team including multidisciplinary rehabilitation professionals. 1. The place, the number of beds, and the staff for acute stroke care were defined in the emergency room of each hospital. Whenever possible, the organization of a stroke unit was recommended. 2. Alternatively, to attenuate the problem of overcrowded emergency rooms, mixed vascular units were organized – defined as a geographic area of the emergency department with several monitored beds for all kinds of acute vascular diseases such as stroke, myocardial infarction, aortic diseases, and pulmonary embolism. The vascular units combine the benefits of acute stroke units and chest pain units. The aim was to have a trained emergency team activating the stroke protocol and calling the neurologist available 24 h a day, seven-days a week, to evaluate and treat the stroke patients. Step 3: Training for stroke care 1. Training of stroke teams, emergency services, and ICU staff of all hospitals with implementation of basic stroke care protocols. 2. Training of all staff for intravenous thrombolysis in level A, B, and C hospitals (see text for definitions). 3. Training of staff for advanced stroke protocols in level A hospitals. 4. Training of SAMU and organization of the local network for faster triage to the appropriate level hospital. 5. Training of level C hospitals for the use of telemedicine. 6. Training of the basic health professionals to activate the SAMU after recognizing the acute stroke signs. 7. Training of the healthcare professionals to improve primary and secondary prevention of stroke. Step 4. National stroke registry In order to ensure quality and minimal standards during the development of the stroke network, hospitals of the National Stroke Program were invited to participate in a national stroke registry, linked to the Ministry of Health (MH), and Sociedad Iberoamericana de Enfermedad Cerebrovascular and Safe Implementation in Treatments in Stroke (SIECV-SITS) Stroke Registry. Step 5. Stroke educational campaigns Campaigns to improve stroke awareness among the population were started after the organization of the acute stroke care in each center. ICU, intensive care unit; CT, computed tomography. © 2013 The Authors. International Journal of Stroke © 2013 World Stroke Organization Vol ••, •• 2013, ••–•• 3 Research S. C .O. Martins et al. between three stroke centers in the cities of Porto Alegre and Salvador (13). After adjusting for stroke severity, etiology, and time of stroke onset, the results showed that Intravenous (IV) thrombolysis for stroke increased 2·54-fold the odds of independent outcome with no increase on death rates and a rate of hemorrhagic transformation that was similar to clinical trials (5·8%). Another relevant motivation for health authorities was the demonstration of the cost-effectiveness of this treatment in the country (14). Pilot study and Porto Alegre stroke network Once the feasibility, safety, and cost-effectiveness of thrombolytic therapy were confirmed in different academic medical centers in the country, a critical step was to evaluate the actual impact of introducing the new therapy in the public health system. A pilot intervention was then planned to provide data for the National Stroke Project. Porto Alegre, a Southern Brazilian city with population of four million inhabitants living in the metropolitan and suburban area of 9800 km (2) was selected for the pilot intervention, which was performed between June 2008 and June 2009. A prehospital team for rescue and transport of stroke patients (SAMU) and five stroke centers were trained on acute stroke protocols including thrombolysis. With the pilot intervention, the proportion of stroke patients treated with IV thrombolysis increased from 1·7% (65/3824) to 5·3% (206/3860). Moreover, in Porto Alegre stroke centers, the mean thrombolysis rate was 14% (range from 12% to 18%) and after three-months, 53% (109/206) of treated patients had minimal or no disability (modified Rankin scale: 0–1), the rate of symptomatic intracranial hemorrhage (SIH) was 4% and the mortality rate was 11% (15,16). Telemedicine As part of the pilot intervention, stroke telemedicine was introduced in the country. The first hospital supported by stroke telemedicine was Hospital de Pronto Socorro in Canoas, a city near Porto Alegre, covering a population of 323 827 inhabitants. Within the first year, 35 patients with the median baseline NIHSS score of 10 (IQR 7–13) were treated and after three-months, 57% (20/35) of the patients were independent (modified Rankin scale: 0–2), 2·9% (1/35) had SIH, and 5·7% (2/ 35 patients) died. Practical lessons from the pilot project in Porto Alegre • The organization of a regional network to assist stroke increased the number of thrombolysed patients. • The establishment of a program to assist stroke, including thrombolytic treatment in the public health, is feasible, safe, and effective and can be expanded to other regions of the country, including neurology evaluation by telemedicine. The project in the whole country The acute stroke project in Brazil included many cities. In each one, the program was tailored according to the local conditions and was developed together with local health authorities. Over three-years, 15 stroke neurologists visited, organized, and classified 90 hospitals in 21 of 26 Brazilian states. Even though those hospitals were already providing treatment to stroke patients, most of them had only a minimal structure and no defined protocols before the National Project. Table 2 shows the improvement in the Brazilian stroke system, and Fig. 1 shows the distribution of stroke centers before (Fig. 1a) and after (Fig. 1b) the Brazilian Stroke Project. National actions 2011–2012 In February 2011, the Federal Government started a new program to control hypertension and diabetes, increasing the distribution of medications for these conditions to the population without cost in more than 20 000 popular pharmacies. After one-year, the number of people that received free medication increased 264% (from 853 thousand per month to 3·2 million per month) (17). In 2011, the Brazilian Ministry of Health started a negotiation to reduce the amount of salt in the processed food. During the 2011 World Stroke Awareness Campaign, an important mobilization was seen all over the country. The campaign created by the World Stroke Organization and organized in the country by the Brazilian Stroke Society, Brazilian Stroke Network, Brazilian Academy of Neurology, and Brazilian Stroke Association involved a common agenda of activities in 51 cities, spread over 22 out of the 26 states, mainly support by nongovernmental organizations. During that campaign, for the first time, the Brazilian Minister of Health addressed the nation on TV and radio specifically about stroke (video is available at: http://www.youtube.com/ watch?v=ZTIeWkDEwoM&feature=youtu.be). Motivated by the repercussion of the campaign, the Minister of Health emphasized the social burden of stroke and announced a new policy for stroke care in the country. The Brazilian National Stroke Policy Act Published by the Brazilian Ministry of Health in April 12, 2012, the act establishes the battle against stroke as a national health Table 2 Structure of the Brazilian stroke system before and after the implementation of the National Stroke Program Number of states with active stroke center Number of stroke centers Private Public Number of stroke units or vascular units 4 Vol ••, •• 2013, ••–•• Before program (May 2008) After program (April 2012) Increase 10 35 20 15 5 19 82 37 45 17 1·9¥ 2·3¥ 1·9¥ 3¥ 3·4¥ © 2013 The Authors. International Journal of Stroke © 2013 World Stroke Organization Research S. C .O. Martins et al. Table 3 Project targets before and after the National Stroke Policy Act Hospitals Stroke reimbursement supported by the MH rtPA Costs of rtPA treatment Education for health professionals Before national policy After national policy (today) No investments in hospitals from the MH. Investments in some cities were from the hospitals or from the health secretaries US$400 – 7–14 days hospitalization included two CT scans plus echocardiogram and carotid duplex Investment in stroke units from the MH Paid by local health authorities and hospitals (no reimbursement by MH) US$2000 per patient Brazilian Stroke Society US$190 per day of hospitalization for patients assisted in stroke units + separate reimbursement for CT and echocardiogram and carotid duplex Reimbursed by MH US$540 per patient MH + Brazilian Stroke Society, Brazilian Academy of Neurology, Brazilian Stroke Network, and Brazilian Medical Association MH, Ministry of Health; CT, computed tomography; rtPA, recombinant tissue plasminogen activator. priority (18). The main elements of the policy can be summarized as follows: • The creation of stroke centers classified in three types according to the hospital complexity. All acute stroke patients have to be assisted in the stroke centers; • Improved reimbursement rates for stroke patients assisted in stroke units; • Centralized reimbursement of rtPA by the Ministry of Health; • Telemedicine support for hospitals without neurologist available 24 h; • The creation of the Line of Stroke Care (a local network) where each city/region has to organize the whole assistance for stroke including primary/secondary prevention, prehospital care, and acute and postacute assistance in the hospital and rehabilitation; • The stroke patients assisted in any component of the network will be transferred to the stroke center by SAMU, which is responsible for acute stroke network regulation; • The dispatcher doctor in the Regulation Centre of SAMU will be the responsible to dispatch the ambulances and to coordinate the distribution of the cases to the stroke centers; • Establishment of home care assistance; • Training for all healthcare professionals together with medical societies; • Improvement of the rehabilitation system with a budget to establish new centers; and • Education for the population. Table 3 summarizes the objectives and targets planned by the Brazilian Ministry of Health regarding stroke care in the near future. What has already been implemented? (July 2012) All over the country, free medication for hypertension and diabetes are now available by a federally funded program in over 20 000 popular drugstores nationwide. The regulation for the reimbursement of rtPA in public hospitals was approved and launched. The cost of the 50 mg ampoule of rtPA was decreased by half. Since May 2012, ampoules of 10 and 20 mg of rtPA are available in Brazil after an agreement between the government and the pharmaceutical company. © 2013 The Authors. International Journal of Stroke © 2013 World Stroke Organization The current classification of stroke centers stratifies centers in three major categories according to the complexity of stroke care: Type I, as the primary stroke center, which has the basic conditions for thrombolysis, neurologist available 24 h a day (in the local, on call or by telemedicine); Type II, which additionally requires an acute stroke unit, with exclusive beds to stroke care; and Type III, with an integral stroke unit, which includes exclusive beds to acute care and rehabilitation until 14 days. A budget of around US$ 200 million was approved to establish new stroke centers in 25 main cities in Brazil and their metropolitan area. The National Educational Program was launched in June 20, 2012, starting in the 10 main cities in Brazil in July. By the time of the submission of this manuscript, 82 stroke centers were active in Brazil (all with thrombolytic therapy), including 45 public hospitals. In November 2011, Porto Alegre became the first city to establish the Line of Stroke Care. This system, which is responsible for 70% of all patients assisted in stroke centers, including three public and two private hospitals, has been working integrated with prehospital transport (SAMU). All hospitals in the city (including the nonstroke centers) and all nonhospital emergency care units (called UPA, which stands for Unidade de Pronto Atendimento) were trained to assist stroke and to call the SAMU. The basic healthcare units started the training for primary and secondary prevention. Three other Brazilian cities have their emergency medical network already organized. The future Brazil is a country of continental dimensions and widespread social inequalities. Universality and equity are among the constitutional principles that provide the foundations for its public health care system. To decrease the social burden of stroke, interventions need to be coordinated among society, healthcare professionals, and public health administration. Guided by an evidence-based medicine approach, those interventions also need to be integrated with local reality and available resources. In Brazil, public resources should be targeted to improve public stroke awareness; to improve primary and secondary prevention; and to increase the numbers of stroke units, which are, from the standpoint of public health, the most cost-effective interventions Vol ••, •• 2013, ••–•• 5 Research of contemporary neurology. In addition, the Brazilian Stroke Society understands that population-based studies are necessary in all major regions of the country, from Amazonia to the south, in order to provide more reliable information about the impact of stroke care policies. Case-fatality proportions and Disability Adjusted Life Years (DALY’S) could be used to measure the impact of stroke units and thrombolysis implementation. One additional aspect that needs to be addressed is stroke rehabilitation within the Brazilian public health. In general wards or in stroke units, each day, doctors are faced with the dilemma of what is the best time to discharge their patients. The problem will grow in the next decades, as the prevalence of stroke patients and life expectancy increases. Historically, Brazilian medicine does not have the option of nursing home hospitals. Stroke medicine also needs be more integrated among different health professionals, encompassing all issues from university training, basic and clinical research support to reimbursement of all healthcare professionals. Conclusions The evolution of stroke care in Brazil over the last decade is a pathway that exemplifies how creativity and perseverance can be used to face the challenges of stroke care in middle-income countries, in order to implement substantial improvement in stroke prevention, treatment, and rehabilitation. The Brazilian experience reported here can be used as an example of how to understand the past, present, and future of stroke care in middleincome countries. Acknowledgements We thank Dr Werner Hacke and Dr Vladimir Hachinski for the official advice given to the Brazilian National Stroke Project and for the support in the Organization of the Brazilian Stroke Network. We thank Dr Bo Norrving for the continuous support to improve stroke in Brazil on behalf of the World Stroke Organization. We thank Dr Nils Wahlgren and Dr Nikolaos Kostulas for the support in the Safe Implementation of Treatments in Stroke (SITS) Registry in Brazil and we thank Dr Pablo Lavados for reviewing this manuscript and for all those who supported the Brazilian Stroke Network and Brazilian Academy of Neurology. 6 Vol ••, •• 2013, ••–•• S. C .O. Martins et al. References 1 Ferreira FHG, Leite PG, Ravallion M. Poverty reduction without economic growth? Explaining Brazil’s poverty dynamics, 1985–2004. J Dev Econ 2010; 93:20–36. 2 DATASUS. Sistemas de informação sobre mortalidade (SIM). Ministério da Saúde, 2012. Available at http://tabnet.datasus.gov.br/cgi/ tabcgi.exe?sim/cnv/obt10uf.def. Accessed 14 July 2012. 3 Schmidt MI, Duncan BB, Azevedo e Silva G et al. Chronic noncommunicable diseases in Brazil: burden and current challenges. Lancet 2011; 377:1949–61. 4 Mansur AD, Favarato D. Mortality due to cardiovascular diseases in Brazil and in the metropolitan region of Sao Paulo: a 2011 update. Arq Bras Cardiol 2012; 99:755–61. 5 Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet 2006; 367:1747–57. 6 Lotufo PA, Goulart AC, Fernandes TG, Bensenor IM. A reappraisal of stroke mortality trends in Brazil (1979–2009). Int J Stroke 2012. doi: 10.1111/j.1747-4949.2011.00757.x. 7 Cabral NL, Goncalves AR, Longo AL. et al. Trends in stroke incidence, mortality and case fatality rates in Joinville, Brazil: 1995–2006. J Neurol Neurosurg Psychiatry 2009; 80:749–54. 8 Cabral NL, Moro C, Silva GR, Scola RH, Werneck LC. Study comparing the stroke unit outcome and conventional ward treatment: a randomized study in Joinville, Brazil. Arq Neuropsiquiatr 2003; 61:188–93. 9 Lotufo PA. Stroke in Brazil: a neglected disease. Sao Paulo Med J 2005; 123:3–4. 10 Pontes-Neto OM, Silva GS, Feitosa MR et al. Stroke awareness in Brazil: alarming results in a community-based study. Stroke 2008; 39:292–6. 11 Massaro AR. Stroke in Brazil: a South America perspective. Int J Stroke 2006; 1:113–5. 12 Timerman S, Gonzalez MMC, Zaroni AC, Ramires JAF. Emergency medical services: Brazil. Resuscitation 2006; 70:356–9. 13 Oliveira Filho J, Martins SCO, Jesus PAP et al. Safety and efficacy of thrombolysis in acute ischemic stroke: experience from three stroke centres in Brazil. In: 15th European Stroke Conference, Bruxelas. Cerebrovasc Dis 2006; 21:141. 14 Araújo DV, Teich V, Passos RBF, Martins SCO. Analysis of the costeffectiveness of thrombolysis with alteplase in stroke. Arq Bras Cardiol 2010; 95:12–20. 15 Martins SCO. The Brazilian Stroke Network: a task force to establish the national stroke program. Int J Stroke 2010; 5:56. 16 Hachinski V, Donnan GA, Gorelick PB et al. Stroke: working toward a prioritized world agenda. Stroke 2010; 41:1084–99. 17 Farmácia popular do Brasil. portaldasaude.saude.gov.br/ portaldasaude. 2012. Available at http://portal.saude.gov.br/portal/ saude/area.cfm?id_area=1095. Accessed in 14 July 2012. 18 Ministério da saúde. Protocolos clínicos e diretrizes terapêuticas. 2012. Available at: http://portal.saude.gov.br/portal/arquivos/pdf/pcdt_ trombolise_avc_isq_agudo.pdf Accessed in 14 July 2012. © 2013 The Authors. International Journal of Stroke © 2013 World Stroke Organization
Download