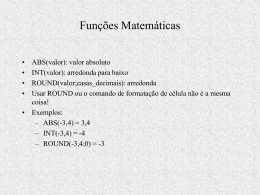
Neisseria Características Gerais do Gênero Neisseria Aeróbico Cocos Gram-negativos com arranjo aos pares (diplococos) com os lados adjacentes planos (forma de rim ou feijão) Oxidase positiva Catalase positiva Imóveis Formam ácido a partir da oxidação de carbohidratos (não da fermentação) Patógenos Humanos Neisseria gonorrhoeae Neisseria meningitidis Outras espécies colonizam as mucosas do orofaringe, nasofaringe e anogenitais Doenças Associadas a Neisseria (ophthalmia neonatorum) Características Diferenciais das Espécies de Neisseria spp. Neisseria gonorrhoeae (gonococcus) Aspectos Gerais da Infecção por Neisseria gonorrhoeae Transmitida por contato sexual Cocos Gram-negativos aos pares com morfologia característica Fastidiosos, capnofílicos e susceptíveis a baixas temperatures, ressecamento e ácidos graxos Meios complexos pré-aquecidos a 35-37C Amido solúvel adicionado para neutralizar ácidos graxos Crescem melhor em atmosfera suplementada com CO2 Produzem ácido a partir da glucose, mas não a partir de outros açúcares Exsudato Uretral - Neisseria gonorrhoeae Epidemiologia da Gonorréia DST com sub notificação Acomete apenas seres humanos com aspectos epidemiológicos diferentes em homens e mulheres Portador assintomático é reservatório Transmissão por contato sexual Possibilidade de re-infecção pela diversidade antigênica das cepas Alto risco de disseminação em pacientes com deficiência de complemento Incidência de Gonorréia nos EUA Diferenças da Epidemiologia entre Homens e Mulheres Homens: Uretrite; Epididimite A maioria das infecções são agudas e simtomáticas com descarga purulenta e disúria após 2-5 dias de período de incubação Homens procuram tratamento precocemente, previnindo sequelas, mas não tão cedo a ponto de previnir a transmissão a outros parceiros sexuais Agentes bacterianos responsáveis por uretrite em homens: N. gonorrhoeae , Chlamydia trachomatis e Mycoplasma genitalium Diferenças da Epidemiologia entre Homens e Mulheres Mulheres: Cervicite; Vaginite; Doença Inflamatória Pélvica (DIP); Infecção gonocóccica Disseminada Mulheres frequentemente assintomáticas ou com manifestações atípicas; Não tratadas até outras complicações se desenvolverem, como DIP • Pode levar a lesões nas trompas de Falópio levando a infertilidade ou gravidez ectópica Diferenças da Epidemiologia entre Homens e Mulheres Mulheres: Infecção Gonocóccica Disseminada: • • • • • • • Resultado de bacteremia Lesões cutâneas Petéquias Pústulas nas extremidades Artralgia Tenosinovite Artrite séptica Gonorréia Females Males 50% risk of infection after single exposure 20% risk of infection after single exposure Asymptomatic infections frequently not diagnosed Most initially symptomatic (95% acute) Major reservoir is asymptomatic carriage in females Major reservoir is asymptomatic carriage in females Genital infection primary site is cervix (cervicitis), but vagina, urethra, rectum can be colonized Genital infection generally restricted to urethra (urethritis) with purulent discharge and dysuria Ascending infections in 10-20% including Rare complications may include salpingitis, tubo-ovarian abscesses, pelvic epididymitis, prostatitis, and inflammatory disease (PID) , chronic periurethral abscesses infections can lead to sterility Disseminated infections more common, including septicemia, infection of skin and joints (1-3%) Disseminated infections are very rare Can infect infant at delivery (conjunctivitis, More common in homosexual/bisexual opthalmia neonatorum) men than in heterosexual populatiuon Patogênese da Neisseria gonorrhoeae Células com fímbrias aderem ao tecido epitélial intacto das mucosas Capacidade de invadir o epitélio ou a pele com abrasões • Aderência ao epitélio das mucosas • Penetração e multiplicação nas células epiteliais das mucosas • Infecção estabelecida na camada sub-epitelial Sítios mais comuns de inoculação: • Cérvice (cervicite) ou vagina em mulheres • Uretra (uretrite) ou penis no homem Gonococcal Virulence Factors Antiphagocytic capsule-like negative surface charge Only fimbriated (piliated) cells (formerly known as colony types T1 & T2) are virulent Outer membrane proteins (formerly Proteins I, II, & III) •Por (porin protein) prevents phagolysosome fusion following phagocytosis and thereby promotes intracellular survival •Opa (opacity protein) mediates firm attachment to epithelial cells and subsequent invasion into cells •Rmp (reduction-modifiable protein) protects other surface antigens from bactericidal antibodies (Por protein, LOS) Acquisition of iron mediated through Tbp 1 and Tbp 2 (transferrin-binding proteins), Lbp (lactoferrin binding protein) & Hbp (hemoglobin-binding protein) Gonococcal Virulence Factors (cont.) Lipooligosaccharide (LOS) (Lipid A plus core polysaccharide but no O-somatic antigen polysaccharide side chain) has endotoxin activity IgA1 protease Acquisition in last two decades of two types of antibiotic resistance: • Plasmid-encoded beta-lactamase production • Chromosomally-mediated changes in cellular permeability inhibit entry of penicillins, tetracycline, erythromycin, aminoglycosides Laboratory Characterization Small, gram-negative diplococci in presence of polymorphonuclear leukocytes (PMN’s) seen microscopically in purulent urethral discharge Susceptible to drying and cooling, so immediate culture of specimen onto pre-warmed selective (e.g., modified Thayer-Martin, Martin-Lewis agars) and nonselective media (chocolate blood agar) with moist atmosphere containing 5% carbon dioxide Some strains inhibited by vancomycin (in many selective agars) and toxic substances like fatty acids and trace metals in protein hydrolysates and agar found in nonselective media Five morphologically distinct colony types (formerly T1 through T5) that can undergo phase transition are no longer considered to be a useful distinction Prevention & Treatment Penicillin no longer drug of choice due to: • Continuing rise in the MIC • Plasmid-encoded beta-lactamase production • Chromosomally-mediated resistance Uncomplicated infxn: ceftriaxone, cefixime or fluoroquinolone Combined with doxycycline or azithromycin for dual infections with Chlamydia Chemoprophylaxis of newborns against opthalmia neonatorum with 1% silver nitrate, 1% tetracycline, or 0.5% erythromycin eye ointments Treatment of newborns with opthalmia neonatorum with ceftriaxone Measures to limit epidemic include education, aggressive detection, and follow-up screening of sexual partners, use of condoms or spermicides with nonoxynol 9 Analytic Performance of Different Laboratory Detection Methods for Nesseria gonorrhoeae NOTE: Importance of Sensitivity vs. Specificity for any Diagnostic Test Analytic Performance of a Diagnostic Test ACTUAL ACTUAL POSITIVE NEGATIVE TEST POSITIVE 80 True Positives TEST 20 NEGATIVE False Negatives 100 TOTALS Actual Positives 25 False Positives 75 True Negatives 100 Actual Negatives TOTALS 105 Test Positives 95 Test Negatives 200 Analytic Performance of a Diagnostic Test (cont.) Sensitivity = Measure of True Positive Rate (TPR) = No. of True Pos. = No. of True Pos. = 80 = 80% No. of Actual Pos. No. of (True Pos. + False Neg.) 80+20 Sensitivity In conditional probability terms, the probability of a positive test given an actual positive sample/patient. Specificity = Measure of True Negative Rate (TNR) = No. of True Neg. = No. of True Neg. = 75 = 75% No. of Actual Neg. No. of (True Neg. + False Pos.) 75+25 Specificity In conditional probability terms, the probability of a negative test given an actual negative sample/patient. Neisseria meningitidis (meningococos) Visão Geral da Neisseria meningitidis Diplococos Gram-negativos encapsulados e pequenos Segunda causa mais comum (após S. pneumoniae) de meningite adquirida na comunidade; progressão abrupta de estado de saúde para doença gravíssima Pathogenicity: • Colonização de células não-ciliadas do nasofaringe mediada por pili • Cápsula antifagocitária (de polissacarídeos) permite espalhamento sistêmico na ausÊncia de imunidade específica • Efeitos tóxicos mediados pela hiperprodução de lipooligossacarídeos Sorogrupos A, B, C, Y, W135 respondem por 90% de todas as infecções Doenças Associadas a Neisseria meningitidis Seguindo a disseminação de organismos virulentos a partir da nasofaringe Meningite Septicemia (meningococcemia) com ou sem meningite Meningoencefalite Pneumonia Artrite Uretrite Neisseria meningitidis no Líquido Céfalo-Raquidiano Epidemiologia da Doença Meningocóccica Humanos são os únicos hospedeiros naturais Transmissão pessoa-a-pessoa por aerossóis de secreções respiratórias Contato próximo com pessoas infectadas (p.e. membros da família, em creches, acampamentos militares, prisões, etc) Maior incidência em crianças com até 5 anos Comumente coloniza nasofaringe de indivíduos saudáveis; alta taxa de colonização oral e de nasofaringe em crianças com idade escolar, adultos jovens e grupos com condições sócio-econômicas baixas Distribuição Etária da Doença Meningocóccica Lacking maternal antibody Pathogenesis of Meningococcal Disease Specific receptors (GD1 ganglioside) for bacterial fimbriae on nonciliated columnar epithelial cells in nasopharynx of host Organisms are internalized into phagocytic vacuoles, avoid intracellular killing in absence of humoral immunity and complement system (patients with late complement deficiencies are particularly at risk) Replicate intracellularly and migrate to subepithelial space where excess membrane fragments are released Hyperproduction of endotoxin (lipid A of LOS) and blebbing into surrounding environment (e.g., subepithelial spaces, bloodstream) mediates most clinical manifestations including diffuse vascular damage (e.g., endothelial damage, vasculitis (inflammation of vessel walls), thrombosis (clotting), disseminated intravascular coagulation (DIC) Skin Lesions of Meningococcemia NOTE: Petechiae have coalesced into hemorrhagic bullae. Immunogenicity of Neisseria meningitidis Following colonization of the nasopharynx, protective humoral immunity develops against the same or closely related organisms of the same serogroup, but not against other serogroups Bactericidal activity of the complement system is required for clearance of the organisms Cross-reactive protective immunity acquired with colonization by closely related antigenic strains and with normal flora of other genera (e.g., E. coli K1); progressive disease can occur in absence of serogroup-specific immunity Laboratory Characterization of Neisseria meningitidis Large numbers (e.g., >107cells/ml) of encapsulated, small, gram-negative diplococci (flattened along adjoining side) and polymorphonuclear leukocytes (PMN’s) can be seen microscopically in cerebrospinal fluid (CSF) Transparent, non-pigmented nonhemolytic colonies on chocolate blood agar with enhanced growth in moist atmosphere with 5% CO2 Oxidase-positive Acid production from glucose and maltose but not from other sugars Prevention and Treatment of Meningococcal Disease Penicillin is drug of choice for treatment in adjunct with supportive therapy for meningeal symptoms • Increasing MIC mediated by genetic alteration of target penicillin binding proteins is being monitored) • Chloramphenicol or cephalosporins as alternatives Chemoprophylaxis of close contacts with rifampin or sulfadiazine (if susceptible) Polyvalent vaccine containing serogroups A, C, Y, and W135 is effective in people older than 2 years of age for immunoprophylaxis as an adjunct to chemoprophylaxis • Serogroup B is only weakly immunogenic and protection must be acquired naturally from exposure to cross-reacting antigens
Baixar