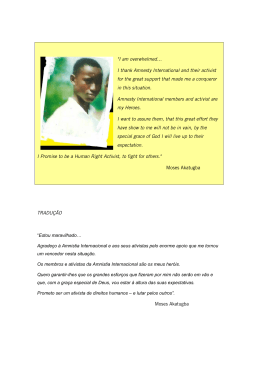
MINISTÉRIO DA EDUCAÇÃO UNIVERSIDADE FEDERAL DO RIO GRANDE DO NORTE CENTRO DE CIÊNCIAS DA SAÚDE PROGRAMA DE PÓS GRADUAÇÃO EM CIÊNCIAS DA SAÚDE CONSEQUÊNCIAS DA COLECTOMIA ASSOCIADA À HEPATECTOMIA NO METABOLISMO HEPÁTICO E NA FORMA E FUNÇÃO DE HEMÁCIAS EM RATOS MARÍLIA DANIELA FERREIRA DE CARVALHO NATAL/RN 2012 MARÍLIA DANIELA FERREIRA DE CARVALHO CONSEQUÊNCIAS DA COLECTOMIA ASSOCIADA À HEPATECTOMIA NO METABOLISMO HEPÁTICO E NA FORMA E FUNÇÃO DE HEMÁCIAS EM RATOS Dissertação apresentada ao Programa de Pós-Graduação em Ciências da Saúde da Universidade Federal do Rio Grande do Norte como requisito para a obtenção do título de Mestre em Ciências da Saúde. ORIENTADOR: Prof. Dr. ALDO DA CUNHA MEDEIROS COORIENTADOR: Prof. Dr. IRAMI ARAÚJO FILHO NATAL/RN 2012 ii MINISTÉRIO DA EDUCAÇÃO UNIVERSIDADE FEDERAL DO RIO GRANDE DO NORTE CENTRO DE CIÊNCIAS DA SAÚDE PROGRAMA DE PÓS GRADUAÇÃO EM CIÊNCIAS DA SAÚDE Coordenadora do Programa de Pós-Graduação em Ciências da Saúde: Prof.a Dra.: Ivonete Batista de Araújo iii MARÍLIA DANIELA FERREIRA DE CARVALHO MOREIRA CONSEQUÊNCIAS DA COLECTOMIA ASSOCIADA À HEPATECTOMIA NO METABOLISMO HEPÁTICO E NA FORMA E FUNÇÃO DE HEMÁCIAS EM RATOS Aprovada em: ____/____/______ Banca Examinadora: Presidente da Banca: Prof. Dr. Aldo da Cunha Medeiros – UFRN ________________________________________ Membros da Banca: Prof.ª Dra. Maria Goretti Freire de Carvalho – UnP ________________________________________ Prof. Dr. Geraldo Barroso Cavalcanti Júnior – UFRN ________________________________________ iv A Daniel, meu irmão, por me fazer entender com a sua ausência o essencial na vida, e por sempre ser uma referência às minhas atividades intelectuais. v AGRADECIMENTOS A Deus, pela minha vida, minha saúde e minha família. Ao meu orientador, Prof. Aldo da Cunha Medeiros, por ter despertado em mim a vocação de ensinar e pesquisar, por ter me dado a oportunidade de estar ao seu lado aprendendo com o seu exemplo de honestidade, determinação, ética, paciência e cordialidade. Ao Prof. Irami Araújo Filho, por ter me ensinado muito além da técnica cirúrgica através de seu exemplo de simplicidade e dedicação aos nossos pacientes. À Amália Cínthia Meneses do Rêgo, pelo exemplo de mulher, mãe, professora e pesquisadora; pela orientação de toda parte laboratorial do nosso estudo. Ao estatístico Ítalo Medeiros Azevedo, pela orientação do nosso trabalho. Aos meus pais, Antônio Martins e Fátima, pelo amor incondicional, principal apoio na realização dos meus sonhos e por sempre estimularem minhas atividades intelectuais. Ao meu marido, Ricardo Moreira, por sua dedicação, compreensão, companheirismo e incentivo constante à realização dos meus sonhos; por tornar minha vida completa e feliz. Às minhas irmãs, Diva e Michele, a quem tenho amor absoluto, por estarem sempre ao meu lado me apoiando, dividindo comigo os momentos mais difíceis e felizes. Às minhas amigas, em especial à Mônica, a quem amo como uma irmã, que sempre esteve próxima, mesmo agora distante, e sempre me motivou. A minha sobrinha Júlia por preencher nossos corações com o seu sorriso. vi “Feliz aquele que transfere o que sabe e aprende o que ensina.” (Cora Coralina) vii RESUMO Este trabalho trata de investigação sobre a influência da colectomia associada à hepatectomia parcial, na biodistribuição do fitato-99mTcO4, na marcação e morfologia de hemácias e parâmetros metabólicos da função hepática. Dezoito ratos Wistar foram distribuídos em três grupos (seis animais cada), denominados: colectomia, colectomia+hepatectomia e sham. No primeiro grupo os animais foram submetidos a uma colectomia direita, no segundo foram submetidos ao mesmo procedimento porém associou-se uma hepatectomia esquerda e no terceiro houve apenas realização de uma laparotomia e leve manipulação de alças intestinais. No trigésimo dia pós-operatório, foi feita injeção de 0,1 mililitro intravenoso de fitato99m TcO4 (radioatividade 0,66 MBq) em todos os animais. Após quinze minutos, uma amostra de fígado foi colhida e pesada. O percentual de radioatividade por grama de tecido (%AIT/g) foi determinado no fígado e hemácias usando-se um contador gama automático. Dosagem sérica de alanina aminotransferase (ALT), aspartato aminotransferase (AST), fosfatase alcalina (FA), morfologia e marcação de hemácias com pertecnetato foram determinadas. O %AIT/g no fígado e nas hemácias foi menor nos animais dos grupos colectomia e colectomia+hepatectomia do que no grupo sham (p<0,05; teste de Tukey). Nenhuma diferença foi detectada comparando os grupos colectomia e colectomia + hepatectomia. A morfologia das hemácias não diferiu entre os 3 grupos. Os níveis séricos de AST, ALT e FA foram significativamente maiores no grupo colectomia+hepatectomia do que no grupo colectomia (p<0,001). Em conclusão, a colectomia associada a hepatectomia contribuiu para reduzir a captação de radiofármaco no fígado e hemácias de ratos, coincidindo com alterações na atividade enzimática do fígado. Descritores: Colectomia. Hepatectomia. Radiofármaco. viii Metabolismo. Biodisponibilidade. ABSTRACT This study investigated the influence of partial colectomy associated with hepatectomy on the biodistribution of the 99m Tc-phytate, on metabolic parameters, as well as labeling and morphology of red blood cells. Wistar rats were distributed into three groups (each with 6), nominated as colectomy, colectomy+hepatectomy and sham. In the 30th postoperative day all rats were injected with 99m Tc-phytate 0.1mL i.v. (radioactivity 0.66 MBq). After 15 minutes, liver sample was harvested and weighed. Percentage radioactivity per gram of tissue (%ATI/g) was determined using an automatic gamma-counter. Serum AST, ALT, alkaline phosphatase and red blood cells labeling were determined. The liver %ATI/g and red blood cells labeling were lower in colectomy and colectomy+hepatectomy rats than in sham rats (p <0.05), and no difference was detected comparing the colectomy and colectomy+hepatectomy groups. Red blood cells morphology did not differ among groups. Serum levels of AST, ALT and alkaline fosfatase were significantly higher in colectomy+hepatectomy than in colectomy rats (p<0.001). Hepatectomy associated with colectomy lowered the uptake of radiopharmaceutical in liver and in red blood cells in rats, coinciding with changes in liver enzymatic activity. Key words: Colectomy. Hepatectomy. Metabolism. Biological availability. Radiopharmaceutical. ix LISTA DE ABREVIATURAS E SIGLAS UFRN- Universidade Federal do Rio Grande do Norte PVPI- Polivinil Pirrolidona Iodo ou iodopovidona CNEM- Comissão Nacional de Energia Nuclear LIGA- Liga Norteriograndense Contra o Câncer %AIT/g- Percentual de radioatividade por grama de tecido ALT- Alanina aminotransferase AST- Aspartato aminotransferase FA- Fosfatase Alcalina ANOVA- Análise de variância Tb- Tempo de meia vida biológica keV- Quiloelétron volt 99 Mo/99mTc- sistema gerador de tecnécio a partir de molibdênio 99m Tc- 99mTecnécio Na99mTcO4- Pertecnetato de Sódio SnCl2 - Cloreto Estanoso CCR- Câncer colorretal UTI- Unidade de Terapia Intensiva CEP- Comitê de Ética em Pesquisa MBq- Megabecquerel HUOL- Hospital Universitário Onofre Lopes x LISTA DE FIGURAS FIGURA 1-Retirada das amostras hepáticas ............................................................14 FIGURA 2-Lavagem das amostras hepáticas ...........................................................14 FIGURA 3-Pesagem dos fragmentos hepáticos em balança de precisão.................15 FIGURA 4-Imagem do Contador Gama.....................................................................15 FIGURA 5-Fotomicrografia das hemácias nos três grupos estudados. (A) Grupo colectomia, (B) Grupo colectomia + hepatectomia e (c) Grupo Sham. 1000x...........23 xi LISTA DE TABELAS Tabela 1- Distribuição do radioisótopo em atividade radiológica por grama de tecido em cada grupo...........................................................................................................23 Tabela 2- Níveis séricos das enzimas hepáticas nos três grupos estudados............22 xii SUMÁRIO 1- INTRODUÇÃO…..……………………………………………………….…...................... 01 1.1-Os Radiofármacos………….……………………………………………………………. 01 1.2-O Tecnécio………………………………………………………..………………………. 03 1.3-A Cintilografia………………..………………………………………………………….... 04 1.4-Colectomia e hepatectomia……………………………………..………………………. 05 1.5-Marcação e Morfologia das hemácias.....………..……………………………………. 08 2-JUSTIFICATIVA………..…………………………………………...…….…..................... 10 3- OBJETIVO…………………………………………………………………….................... 12 3.1-Objetivos gerais…………………………………………………………………………... 12 3.2-Objetivos específicos............................................................................................... 12 4- MÉTODO................................................................................................................... 13 5-ARTIGOS PRODUZIDOS........................................................................................... 17 5.1-Metabolic and hematologic consequences of colectomy associated to hepatectomy in rats…………………………………………………………………………… 17 5.2-Metabolism and gastric remnant changes after Roux-en-Y Gastric Bypass in rats…………………………………………………………………………………………....... 28 5.3-Diabetes and biodistribution of pertechnetate (Na99mTcO4) in rats……………….. 41 5.4-Splenectomy changes the biodistribution of pertechnetate (99mTcO4-) in rats................................................................................................................................. 52 5.5-Bacterial translocation in rats treated with simvastatin undergoing intestinal ischemia and reperfusion…………………………………………………………………….. 62 5.6-Ileal interposition for the treatment of diabetes in rats: repercussion on beta cells mass……………………………………………………………………………………………. 76 5.7-Hepatectomy for benign and malign diseases in University Hospital....................... 89 5.8-Sildenafil as a vasodilatatory mediator in the treatment of abdominal sepsis……………………………………………................................................................ 98 6- COMENTÁRIOS, CRÍTICAS E SUGESTÕES........................................................... 110 7-REFERÊNCIAS........................................................................................................... 116 xiii 1 1. INTRODUÇÃO Ao longo dos anos os avanços na área da saúde modificaram a forma como é diagnosticada e tratada a grande maioria das doenças. Alguns métodos diagnósticos possuem grande precisão porém, não são ao todo isentos de resultados equivocados, principalmente quando se entende o paciente como um ser singular exposto a situações e experiências distintas. Já é bem estabelecido na literatura que algumas doenças, medicações, radioterapias e cirurgias podem falsear resultados de exames cintilográficos1-10, visto que estas circunstâncias podem modificar a capacidade de ligação entre os radiofármacos e as proteínas teciduais9. Uma cirurgia de grande porte (um extenso procedimento cirúrgico relativamente difícil, envolvendo órgãos vitais) pode resultar em importantes alterações anatômicas 4,11,12 imprevisíveis e metabólicas e/ou complicações mutáveis e . Existem poucos trabalhos na literatura que avaliam os efeitos dessas intervenções cirúrgicas na biodistribuição de radiofármacos3. 1.1 Os radiofármacos Radiofármacos são compostos químicos radioativos usados em procedimentos diagnósticos e terapêuticos4,5,7,11,13-15. Na medicina nuclear quase 95% dos radiofármacos são usados para fins de diagnóstico, enquanto os demais são utilizados para tratamento, podendo este último causar danos aos tecidos. Quando possuem função diagnóstica são utilizados para avaliar esvaziamento gástrico, função hepática, função tireoidiana, doenças ósseas, metástases à distância, sangramentos, entre 18 outras aplicações3,4,7,11,16,17, além de distúrbios 19 hemodinâmicos , avaliação da perfusão pulmonar , função e anatomia renal20, e estudos da perfusão miocárdica21. A distribuição de um radiofármaco num órgão é proporcional ao seu grau de disfunção. Por exemplo, no fígado a biodistribuição mantém correlação com o grau da gravidade da doença hepática, a severidade do grau de fibrose na histologia e da disfunção hepática22. Ainda em relação ao fígado, a cintilografia também é uma ferramenta no diagnóstico diferencial da esteatohepatite não alcoólica da simples esteatose. A captação hepática de 99mTc-fitato fornece um índice prático da função hepática e da sua imagem, usando a cintilografia como importante método diagnóstico das alterações da função e 2 morfologia23. Um radiofármaco tem dois componentes: um radionuclídeo e um fármaco; a escolha de qual radiofármaco deverá ser usado é orientada pela sua predileção por determinado órgão ou por determinado componente fisiológico que se pretende ser avaliado14,24. É desejável que o radiofármaco se localize preferencialmente no órgão objeto do estudo, uma vez que a atividade de áreas não alvo podem obscurecer os detalhes estruturais da imagem do órgão alvo. As radiações do radioisótopo devem ser facilmente detectadas através de equipamentos nucleares, e a dose de radiação para o paciente deve ser mínima. Por serem usados em humanos, essas substâncias devem ser estéreis e livres de pirógenos, sendo submetidos a todas as medidas de controle de qualidade exigidas para um medicamento convencional. A diferença entre um traçador radioativo e um radiofármaco reside no fato de que o primeiro não pode ser administrado em humanos, devido à falta de controles adequados como o de esterilidade e apirogenicidade. Geralmente estas substâncias são administrados em pequena quantidade24, em dose única e não devem produzir efeitos farmacológicos. Os radiofármacos considerados ideais deverão apresentar rapidez de obtenção, fácil disponibilidade e produção, baixo custo e meia-vida suficientemente curta para diminuir a taxa de exposição do doente à radiação4,14 mas também longa o suficiente para permitir finalizar o processamento da imagem. Um radiofármaco decai com uma meia-vida definida que é caracterizada pelo radionuclídeo, denominada pela abreviação Tp ou t1/2, independente das condições físico-químicas. Quando um radiofármaco é administrado, o processo de biodistribuição se inicia e este consiste de: absorção, distribuição, metabolismo e excreção; esta última etapa pode acontecer através da eliminação fecal, urinária, transpiração ou outros mecanismos. A biodistribuição de um radiofármacos baseia-se nos mesmos princípios farmacocinéticos descritos para um agente terapêutico e pode ser alterada por procedimentos cirúrgicos25. Há fatores que afetam a marcação de hemácias com 99m Tc, entre eles: o tempo de estanhagem, níveis de hematócrito, método de injeção, período de tempo que o radiofármaco é incubado com hemácias, volume de sangue radiomarcado, a quantidade de íon estanoso usado, entre outros. Particularmente com o advento do método in vivo de marcação das hemácias, problemas relativos à interferência de vários medicamentos começaram a aparecer na literatura7-10 . Desse modo, quando um paciente está usando um determinado medicamento, ou se foi previamente submetido a um procedimento cirúrgico, a biodistribuição do 3 radiofármaco administrado por via intravenosa para a realização de cintilografia poderia7-9,25,26 gerar a possibilidade de diagnósticos equivocados, levando à repetição do exame com um aumento na dose de radiação4,5. Este fato não ocorre somente no tecido traumatizado, mas também em outros órgãos não manipulados pela intervenção cirúrgicas7. O decaimento biológico de um radiofármaco segue uma lei exponencial semelhante ao do decaimento do radionuclídeo. Assim, cada radiofármaco tem uma meia-vida biológica (Tb), sendo este o tempo necessário para que a metade dele desapareça e, por conseguinte, está relacionada com uma constante de decaimento, λb = 0.693/Tb. Portanto, em qualquer sistema biológico, a perda de um radiofármaco é devida tanto à desintegração física do radionuclídeo como pela eliminação biológica do radiofármaco. O decaimento pode ocorrer pela emissão de partículas α e β, porém estas não devem ser usadas para fins diagósticos, visto que causam danos aos tecidos, por este motivo prefere-se os raios γ. Seja qual for o modo de decaimento, para estudos de diagnóstico do radionuclídeo, este deve emitir radiação γ com uma energia entre 30 e 300 keV14. Abaixo de 30 keV os raios γ são absorvidos pelo tecido e não são captados pelo detector24. 1.2 O 99mTecnécio O crescimento e a ampla aplicação da medicina nuclear diagnóstica tem sido impulsionada pela fácil disponibilidade do tecnécio através do sistema gerador 99 Mo/99mTc portátil e das propriedades quase ideais da radiação gama produzida por este radionuclídeo que possibilitou seu uso clínico nos mais diversos tecidos26. O 99m tecnécio (99mTc) é um metal de transição de cor acinzentada pertencente ao grupo VIIB da tabela periódica e tem o número atômico 43. Apresenta emissão de raios gama numa energia de 140KeV11,27-29 com pequena emissão de radiação corpuscular29, sendo obtido em gerador de molibidênio (99Mo/99mTc)14,15 que é o gerador mais importante em medicina nuclear, o que levou à disponibilidade quase ilimitada de 99m Tc29. O tecnécio pode existir em oito estados de oxidação de -1 até +7, que resultam da perda de um determinado número de elétrons. A estabilidade destes estados de oxidação depende do tipo de ligantes e do ambiente químico, sendo os estados +4 e +7 os mais estáveis, sob a forma de óxidos, sulfuretos, halogenetos e pertecnetatos. Os estados de oxidação mais baixos, -1, 1+, +2, e +3, 4 são normalmente estabilizados por complexação com ligantes24. A forma química utilizada para leitura em gama câmera é o pertecnetato de sódio (Na99mTcO4), possui valência +7, e necessita de redução iônica para a marcação de substâncias, células ou órgãos em estudo. Para tal processo, a substância mais utilizada é o cloreto estanoso (SnCl2), sendo os componentes inicialmente dissolvidos em solução, liofilizados e armazenados em atmosfera de azoto ou gás inerte (diminui a oxidação do Sn2+)14. O tecnécio é um dos radionuclídeos mais utilizados em medicina nuclear27,30, corresponde a mais de 80% do total usado4,24,26 devido se ligar a uma grande variedade de moléculas e células5,31. O Na99mTcO4 pode entrar ou sair do meio intracelular livremente, num processo de difusão passiva32. Além disso, essa substância preenche muitos dos critérios de um radionuclídeo ideal: possui radiação, custo, impacto ambiental e energia de emissão muito baixos; é de fácil uso na marcação de hemácias; tem facilidade de obtenção; possui 10% de conversão interna e uma meia vida curta (6h), o que diminui a taxa de exposição dos doentes à radiação2,11,15,24,26,33,34. 1.3 A cintilografia As radiações gama (γ), são emissões de natureza eletromagnética, ou seja, são fótons com massa desprezível e sem carga elétrica; tais características conferem a esta radiação uma menor possibilidade de interação com a matéria quando comparada à capacidade de interação das partículas alfa (α) e beta (β). Assim, a radiação gama tem menor capacidade de ionização e alta energia, o que permite que ela percorra longas trajetórias e atravesse corpos de maior espessura. Esses fatores fizeram com que a medicina nuclear a elegesse como a radiação usada nos exames de imagem, sendo o tecnécio o isótopo radioativo mais frequentemente usado como seu emissor35. Após a administração do radiofármaco, geralmente por via endovenosa, podendo ser também via inalatória ou oral, os radioisótopos, ou os compostos aos quais estão acoplados, têm um comportamento biológico que é idêntico ao de similares não radioativos. Este comportamento biológico é determinado pelas características físico-químicas do composto e também pelo estado funcional dos diferentes tecidos ou células que podem estar envolvidos em sua manipulação5. 5 Essas radiações partem do interior do corpo e são captadas por equipamentos, dotados de um cristal sensível, que capta cada radiação que chega produzindo uma centelha ou cintilação para formar a imagem final, daí o nome cintilografia. O aparelho que registra as radiações é chamado de gama câmara e seu componente principal é a câmara de cintilação, onde se originam informações processadas por um sistema complexo de computação que serão convertidas em imagem. Esta câmara opera no mesmo princípio de um contador de radiação gama, mas é consideravelmente mais complexa na sua construção e funcionamento35,36. A biodistribuição pode ser medida por método invasivo, envolvendo o sacrifício de animais e quantificação da radioatividade nos órgãos e tecidos de interesse, como realizado no nosso estudo, ou por métodos não invasivos37. Esse exame pode ser realizado em diversos órgãos como coração, pulmões, ossos, rins e outros. No caso da cintilografia renal, o exame fornece imagens funcionais dos rins, ou seja, mostra como as células estão desempenhando suas funções. Devido à permanência prolongada do traçador no córtex renal, o exame fornece informações principalmente relativas à concentração do mesmo no parênquima renal, morfologia e dimensões dos rins38. Outros exemplos do uso da cintilografia com o tecnécio (99mTcpertecnetato de sódio) é o diagnostico da mucosa gástrica ectópica (pesquisa de divertículo de Meckel) onde o pertecnetato é captado pela mucosa, além do uso na pesquisa do sangramento intestinal39-41. A sensibilidade avançada dessa técnica permite detectar alteração na função de diversos órgãos, muitas vezes superior à de outros exames36. 1.4 Colectomia e hepatectomia O câncer colorretal corresponde à segunda causa de morte por câncer no Estados Unidos e Reino Unido42-45 além de ser o terceiro mais prevalente no mundo44 depois do câncer de pulmão e estômago46; aproximadamente 150.000 casos de câncer colorectal (CCR) ocorrem todos os anos nos Estados Unidos47 com 63.000 mortes anualmente45. No Brasil o cancer colorretal também é o terceiro mais comum, no ano de 2012, esperam-se 14.180 casos novos de câncer do cólon e reto em homens e 15.960 em mulheres48. Aproximadamente 40% dos pacientes com CCR morrem devido à recorrência e às metástases. Durantes as duas últimas 6 décadas, testemunhamos melhorias substanciais na sobrevida de pacientes com esta neoplasia que foi resultante de um diagnóstico mais precoce, maior eficiência da quimioterapia e radioterapia, e os avanços nas técnicas cirúrgicas, melhorias na área da anestesia e cuidados pós-operatórios, principalmente em UTIs, reduzindo a morbi-mortalidade apesar da abordagem cirúrgica mais agressiva49. No entanto, a melhor promessa de cura continua sendo a excisão cirúrgica adequada do tumor43,44,50-53. O fígado é o sítio mais frequente de metástases do CCR e estas podem ocorrer em até 60% dos pacientes43,47,52-54 porque a drenagem venosa do cólon e reto superior ocorre através da veia porta que drena diretamente para o fígado. Sabe-se que 60-70% do câncer colorretal recorrente envolve o fígado e que este é o órgão unicamente envolvido em 20-35% dos casos46-49. No momento do diagnóstico entre 15-25% dos pacientes têm metástases hepáticas clinicamente detectáveis41-44,52 e em torno de 20%-45% dos pacientes vão desenvolver metástase hepática metacrônica43,46,55, que são aquelas evidenciadas após 6 meses do diagnóstico. Porém apenas 20% dos pacientes possuem doença ressecável44,46. As recidivas após ressecção primária das lesões estão confinadas ao fígado, em aproximadamente, 50% dos casos46. As ressecções das metástases hepáticas caracterizavam um grande desafio para os cirurgiões no passado, devido a sua alta taxa de mortalidade, mas atualmente a taxa de mortalidade é de cerca de 1-5% em importantes centros médicos46,56. Esses procedimentos se tornam cada vez mais seguros, podendo-se ressecar até 80% do parênquima hepático57. Apesar desses avanços, a taxa de ressecabilidade de metástases no momento do diagnóstico ainda é baixa, representando a baixa proporção de pacientes que podem se beneficiar de uma abordagem cirúrgica. Os principais obstáculos para a indicação da ressecção hepatica são: a doença metastática bilobar, tumores volumosos e deixar parênquima hepático residual funcional suficiente após a ressecção57. As hepatectomias são procedimentos relacionados a grande morbi-mortalidade devido a insuficiência hepática que guarda relação com o tamanho da ressecção e se o paciente tem outras doenças hepáticas. Não há evidência de que o número de lesões ou suas localizações no fígado comprometam a sobrevida desde que toda a doença macroscópica seja ressecada. Tem sido argumentado que o fator limitante para o número de lesões que podem ser ressecados é se é tecnicamente possível 7 remover todos os tumores43,49. Porém, os critérios de ressecção vêm sendo contestados por diferentes grupos de pesquisadores ao longo da última década44,52; além disso, o paradigma sobre o tratamento cirúrgico das metástases colorretais sincrônicas também começou a mudar, com autores relatando bons resultados para ressecção simultânea de cólon e metástases do fígado. Os defensores de uma abordagem em dois tempos aprovam esta estratégia devido à preocupações com aumento da morbidade e mortalidade associadas à ressecção simultânea do câncer colorretal com metástases hepáticas58, porém tal fato culmina com uma abordagem mais agressiva no tratamento de metástases hepáticas colorretais45. Embora o câncer colorretal primário tenha um bom prognóstico quando ressecado com margens livres e linfonodos negativos, o diagnóstico de metástases hepáticas é o prenúncio de uma evolução pior. Até recentemente, os pacientes inicialmente considerados como não-ressecáveis foram tratados através de quimioterapia paliativa, com baixas chances de sobrevida em cinco anos51. Estratégias que ampliaram as indicações de ressecção hepática incluindo a quimioterapia locorregional44, embolização da veia porta, quimioterapia neoadjuvante e os procedimentos ablativos; estes últimos apesar da alta taxa de recorrência local podem ser considerados como opção terapêutica nos pacientes sem indicação de quimioterapia loco-regional59. A recente adição de novos regimes de quimioterapia, tais como o irinotecano e oxaliplatina46 e terapia com drogas específicas, tais como bevacizumab e cetuximab demonstraram sobrevida mediana de até 20 meses para pacientes com câncer do cólon, mas eles raramente fornecem uma cura a longo prazo. As taxas de resposta obtidas com 5-fluorouracil e leucovorina foram significativamente aumentadas em combinação com oxaliplatina, irinotecano. Isto permitiu o aumento da sobrevida do paciente em um status paliativo, mas também ofereceu a possibilidade de cura de pacientes previamente irressecáveis sendo estes considerados em reestadiamento melhor que os anteriores. Por reconsiderar a irressecabilidade inicial de pacientes que respondem fortemente à quimioterapia, a sobrevida poderia então ser alcançada através da ressecção hepática em uma significativa proporção de pacientes51. Cerca de 10-20% dos pacientes considerados irresecáveis passam a ser candidatos à metastasectomia. A cirurgia oferece a melhor chance de cura em pacientes com metástases hepáticas colorretais sendo as taxas de sobrevida após a ressecção, em cinco anos, entre 25% e 58%46,49,52-56 com uma sobrevida mediana entre 28 e 40 8 meses em grandes séries. Resultados de dez anos de sobrevida foram documentados em torno de 20% a 26%. Em contraste, a sobrevida mediana para não-ressecados, com metástases hepáticas colorretais, é 5-10 meses54. Porém, nem todos os pacientes possuem indicação cirúrgica e a decisão sobre ressecabilidade depende das condições do paciente, extensão da doença e da função hepática. Desse modo, apenas 10 a 20 % são candidatos à ressecção52,59. Apesar disto, as opções para tratamento não-cirúrgico do câncer colorretal metastático é muito vasta. Se a metástase hepática é diagnosticada juntamente ao tumor primário, e é factível sua remoção, deve ser ressecada no mesmo ato operatório do tumor primário, mas caso seja evidenciada posteriormente, ela é ressecada em outro tempo cirúrgico. No presente trabalho optamos por submeter os animais a uma colectomia direita e hepatectomia esquerda simulando que esses teriam um tumor de cólon direito e metástases hepáticas apenas à esquerda (que caracterizaria uma cirurgia de grande porte) para avaliar as possíveis alterações, em modelo animal, na biodistribuição do radiofármaco e da morfologia das hemácias. Não foi objeto do nosso estudo a carcinogênese , desse modo não foi induzido câncer nestes animais, mas sim o impacto de uma cirurgia de grande porte nos parâmetros estudados. A cirurgia em questão foi escolhida por ser um procedimento cirúrgico cada vez mais indicado para o tratamento, com possibilidade curativa, de paciente com diagnóstico de adenocarcinoma de cólon com metástase hepática, visto que sua incidência é crescente ao longo das últimas décadas. 1.5 Marcação e Morfologia das hemácias Desde o primeiro relato do uso do tecnécio como métodos de marcação de hemácias, foram observadas melhorias que levaram a redução: do dano celular, da eficiência de marcação e de rendimento, e do tempo gasto no procedimento60. Os glóbulos vermelhos marcados com 99m Tc são usados em muitos procedimentos de medicina nuclear2,10,34,61, incluindo os estudos de localização do baço, do sistema cardiovascular, da 9,39 gastrointestinal placenta7,24, além de localizar sítios de sangramento . As hemácias marcadas com radiomarcadores podem ser usadas in vivo, in vitro ou em uma combinação de ambos chamada in vivo/vitro7,34,62. Há uma qualidade maior de imagem no método in vitro em comparação com as outras técnicas31. Os passos sequenciais do processo de marcação intracelular das 9 hemácias incluem: (1) o transporte transmembranar de íons de cloreto estanoso7 e pertecnetato no compartimento interno destas células, (2) redução de (99mTcO4-) pelo SnCl2 e (3) de ligação do 99m 99m Tc Tc reduzido para hemoglobina2. A banda-3 é o sistema de transporte do tecnécio para o interior das hemácias, e os canais de cálcio são responsáveis pelo transporte do estanho33,34,63. A literatura médica sobre o assunto em questão descreve o efeito de drogas artificiais e naturais no processo de radiomarcação de células vermelhas do sangue e proteínas plasmáticas com 99m Tc. Qualquer droga pode modificar a biodisponibilidade de radiofármacos, podendo alterar a marcação de constituintes sanguíneos atuando como agente antioxidante, modificando a estrutura da membrana ou diminuindo a eficiência do sistema de transporte transmembrana de íons estanoso e pertecnetato nas células. Neste estudo avaliamos o impacto da cirurgia de grande porte na morfologia e na marcação das hemácias61 com o tecnécio, a partir de um modelo experimental, pois sabemos que ocorrem alterações nas mesmas em situações de trauma, e quanto mais severo o trauma, mais intensas são as alterações64. 10 2. JUSTIFICATIVA Já é bem estabelecido na área da medicina nuclear que determinadas patologias, medicamentos, produtos naturais e determinados procedimentos cirúrgicos podem alterar a biodistribuição do tecnécio e/ou fixação dos constituintes sanguíneos7,8,9,26. Este fato não ocorre somente no tecido traumatizado, mas também em outros órgãos não submetidos a intervenções cirúrgicas7. Este estudo se propõe a avaliar se a biodistribuição de um determinado radiofármaco também sofreria influência após a realização de uma cirurgia de grande porte, em modelo murino, além de estimar se tais fatores exercem alguma alteração na função hepática, bem como sobre a morfologia e marcação das hemácias. O radiofármaco utilizado foi o tecnécio por ser facilmente disponibilizado e ter propriedades quase ideais26. Devido ao CCR ser uma doença muito prevalente44, e as metástases hepáticas associadas à este muito frequentes41-44; temos na cirurgia o melhor tratamento para esta doença avançada43,44,51-53. Por isso, escolhemos o procedimento cirúrgico colectomia direita com hepatectomia esquerda como representante do grupo de cirurgia de grande porte pois, além de ser cada dia mais realizado, por ser mais factível, este procedimento também revolucionou o tratamento do câncer colorretal nas últimas décadas, elevando os pacientes portadores do CCR com metástase hepática de uma situação de tratamento paliativo a uma de potencial cura. A cintilografia é um procedimento diagnóstico usado pela medicina nuclear para avaliar diversas patologias como sangramentos digestivos, estudos de perfusão, estudos funcionais renais. Esta pode ser utilizada em pacientes com história prévia de câncer no cólon, com implantes metastáticos no fígado, que foram submetidos à ressecção curativa através de colectomia associada à hepatectomia para acompanhar um possível surgimento de metástase ou sangramentos em diversos órgãos digestivos. Qualquer desvio na captação de radiofármacos por órgãos vitais após procedimento cirúrgico pode acarretar interpretações indesejáveis nos resultados de exames cintilográficos, conduzindo a diagnósticos equivocados de doenças, com graves consequências ao acompanhamento dos pacientes. Além disso, existindo a necessidade de repetição do exame teríamos, consequentemente, um aumento na dose de radiação4,5 para o paciente e maior risco para os profissionais envolvidos. Desse modo, o metabolismo hepático, a marcação de 11 hemácias e a biodistribuição do tecnécio podem estar alterados em órgãos importantes, assim os exames cintilográficos poderão estar sujeitos a resultados falso-positivos ou falso-negativos. Pesquisa bibliográfica minuciosa em bases de dados eletrônicas revelou ausência de estudos nessa linha de pesquisa: alteração na biodistribuição de radiofármacos após colectomia com hepatectomia. Foram usados descritores como: metabolismo, biodistribuição, tecnécio, isótopos radioativos versus colectomia associada a hepatectomia. Desse modo, o estudo experimental teve a intenção de dar contribuição importante para o conhecimento de aspectos ainda não esclarecidos. 12 3. OBJETIVOS 3.1 Objetivo geral Este trabalho objetiva avaliar se a realização de uma colectomia com hepatectomia em ratos exerce influência na biodistribuição do radiofármaco 99mTc-fitato e na função hepática. 3.2 Objetivos específicos Avaliar se a biodistribuição do tecnécio, no fígado e hemácias de ratos, sofre alteração após um colectomia direita com hepatectomia esquerda. Avaliar se o procedimento cirúrgico descrito altera os valores das enzimas hepáticas: TGO, TGP e FA. Avaliar se tal intervenção cirúrgica altera a marcação e morfologia das hemácias. 13 4. MÉTODOS O modelo animal escolhido para realização desta pesquisa experimental foi o rato Wistar. Os 18 animais utilizados foram fornecidos pelo biotério do Centro de Ciências da Saúde, com pesos no intervalo de 285±23 g. Foram alojados em gaiolas individuais de polipropileno e mantidos sob condições controladas de temperatura e ambiente com um ciclo claro-escuro de 12 horas. Foi permitido acesso ad libitum ao alimento na forma de ração (Labina, Purina ®) e água. Todos os procedimentos experimentais envolvendo os animais foram realizados de acordo com o Código de Ética para a experimentação animal e as diretrizes brasileiras para o uso científico de animais (Lei n º 11.794). O protocolo foi aprovado pelo Comitê de Ética em Pesquisa (CEP) da Universidade Federal do Rio Grande do Norte (UFRN). No pré-operatório os animais permaneceram em jejum entre 12-18 horas. A anestesia foi realizada com injeção intraperitoneal de 0,2 ml/100 g de uma solução contendo 1 ml de cetamina (50 mg) e 1 ml de xilazina (20 mg) e então os animais foram operados sob condições assépticas após tricotomia e antissepsia com álcool 70%. Além disso, foi mantida analgesia por via subcutânea imediatamente após a cirurgia, e a cada 12 horas durante três dias com cloridrato de tramadol solução contendo 1ml (100 mg) na dose de 20 mg/kg. Os animais foram divididos, aleatoriamente, em três grupos com seis ratos cada; o primeiro grupo chamado colectomia foi submetidos à laparotomia mediana e realizou-se uma colectomia parcial direita. Foram ressecados o ceco, 10 cm de cólon direito e 5 cm de íleo terminal. O trânsito intestinal foi reconstruído através de anastomose término-terminal ileocólica com sutura em pontos separados usando fio de polipropileno 6-0 (Ethicon®, Brasil), com auxílio um microscópio cirúrgico – aumento 10x (DFVasconcelos, São Paulo, Brasil). A laparotomia foi fechada por planos através de sutura contínua com fio mononylon 4-0 (Ethicon®, Brasil). No segundo grupo, denominado colectomia+hepatectomia, os ratos foram submetidos à colectomia parcial, com a mesma técnica descrita acima para o grupo colectomia, associada à ressecção do lobo esquerdo do fígado (hepatectomia esquerda), sendo a reconstrução do trânsito e o fechamento da cavidade realizado da mesma forma citada para o grupo colectomia. No terceiro grupo, chamado sham, que caracteriza o grupo controle, foi realizada laparotomia mediana e manipulação suave das alças do 14 intestino, sendo a parede abdominal fechada nas mesmas condições dos outros grupos. Os animais dos três grupos permaneceram em observação por 30 dias, em gaiolas individuais nas condições ambientais previamente descritas, e nesse período foram pesados semanalmente em balança digital (Filizola® São Paulo, Brasil) com sensibilidade para variação a partir de 1 grama. Após esse periodo os animais foram anestesiados e submetidos à administração de radiofármaco através da cateterização da veia femoral numa alíquota de 0,1 ml de 99mTc-fitato, correspondendo a uma atividade radioativa de 0,66 MBq. Decorridos quinze minutos da administração do radiofármaco, foi colhida amostra de 5 ml de sangue por punção cardíaca, os animais foram sacrificados com superdose de anestésico (tiopental sódico 100mg/Kg intraperitoneal) e procedeu-se a retirada de amostra do fígado para determinar a biodistribuição do fitato (Figura 1), a seguir estas foram lavadas com solução salina 0,9% (Figura 2) e pesadas em balança de precisão (Figura 3). Um contador gama automático Wizard 1470 (Perkin-Elmer®, Finlândia) detectou a captação radioativa hepática e das hemácias, medidas em percentual de radioatividade por grama de tecido (% ATI/g) (Figura 4). Figura 1- Retirada das amostras hepáticas. Figura 2- Lavagem das amostras. 15 Figura 3-Pesagem em balança de precisão. Figura 4-O Contador Gama. Toda essa fase do experimento, que utiliza radiação, seguiu as normas de radioproteção preconizados pela Comissão Nacional de Energia Nuclear (CNEM). O radiofármaco utilizado foi fornecido pelo Serviço de Medicina Nuclear da Liga Norteriograndense Contra o Câncer (LIGA) e os rejeitos radioativos foram prontamente devolvidos para a LIGA em recipiente de chumbo, para tratamento adequado. Avaliação bioquímica As amostras de sangue, em volumes de 3 ml, foram inseridas em tubos de ensaio sem anticoagulante, centrifugadas a 3000 rpm por 10 min e as alíquotas de plasma estocadas a -40°C até análise. Os provas de função hepática como: Aspartato aminotransferase (AST), alanina aminotransferase (ALT) e fosfatase alcalina (FA) foram medidas usando um kit comercial e dosadas em auto-analisador (Konelab, versão do software, 60i, Finlândia). Morfologia das hemácias A partir de amostras de sangue total foram preparadas distensões sanguíneas em lâminas, que foram coradas pelo método Leishman. As imagens das hemácias foram capturadas por câmera digital (Samsung®) usando-se microscopia óptica (Microscópio Olympus, modelo BX50, Japan, aumento 1000x,) para análise digital, após a transferência da imagem do microscópio para a tela do computador. Para 16 obtenção da forma das hemácias e das medidas morfométricas (relação perímetro/área) foi utilizado programa específico (Image ProPlus Software, versão 6.0). Estatística Os dados obtidos foram expressos em média ± desvio padrão. A comparação entre os grupos foi realizada pela análise de variância (ANOVA) e pelo teste de comparações múltiplas de Tukey, usando-se significância de 0,05. 17 5. ARTIGOS PRODUZIDOS 5.1. O Artigo foi publicado no periódico Acta Cirúrgica Brasileira 2011;26(6):503-07. ISSN 1678-2674. Que possui fator de impacto 0.2486, Qualis B1 da Capes para Área Medicina III. Metabolic and hematologic consequences of colectomy associated to hepatectomy in rats1 Consequências metabólicas e hematológicas da colectomia associada à hepatectomia em ratos Marília Daniela Ferreira CarvalhoI, Irami Araújo-FilhoII, Ítalo Medeiros AzevedoIII, Amália Cínthia Meneses RêgoIV, Aldo Cunha MedeirosV 1 Research performed at Center of Experimental Surgery, Department of Surgery, UFRN, Natal-RN, Brazil. I Fellow Master Degree, Postgraduate Program of Health Sciences, UFRN, Natal, Brazil. Acquisition, interpretation of data and collection of study informations. II PhD, Associate Professor, Department of Surgery, Federal University of Rio Grande do Norte (UFRN), Natal, Brazil. Involved with technical procedures. III Fellow Master Degree, Department of Statistics, UFRN, Natal, Brazil. Responsible for interpretation of data, statistical analysis. IV PhD, Associate Professor, Potiguar University, Natal, Brazil. Helped with technical procedures, collection and processing of study informations V Chairman, Full Professor, Department of Surgery and Postgraduate Program of Health Sciences, UFRN, Natal, Brazil. Responsible for conception, design, intellectual and scientific content of the study. ABSTRACT Purpose: This study investigated the influence of partial colectomy associated with hepatectomy on the biodistribution of the 99m Tc-phytate, on metabolic parameters, as well as labeling and morphology of red blood cells. Methods: Wistar rats were distributed into three groups (each with 6), nominated as colectomy, 18 colectomy+hepatectomy and sham. In the 30th postoperative day all rats were injected with 99m Tc-phytate 0.1mL i.v. (radioactivity 0.66 MBq). After 15 minutes, liver sample was harvested and weighed. Percentage radioactivity per gram of tissue (%ATI/g) was determined using an automatic gamma-counter. Serum AST, ALT, alkaline phosphatase and red blood cells labeling were determined. Results: The liver %ATI/g and red blood cells labeling were lower in colectomy and colectomy+hepatectomy rats than in sham rats (p <0.05), and no difference was detected comparing the colectomy and colectomy+hepatectomy groups. Red blood cells morphology did not differ among groups. Serum levels of AST, ALT and alkaline fosfatase were significantly higher in colectomy+hepatectomy than in colectomy rats (p<0.001). Conclusion: Hepatectomy associated with colectomy lowered the uptake of radiopharmaceutical in liver and in red blood cells in rats, coinciding with changes in liver enzymatic activity. Key words: Colectomy. Hepatectomy. Metabolism. Biological availability. Radiopharmaceutical. RESUMO Objetivo: Investigar a influência da colectomia associada à hepatectomia parcial, na biodistribuição do fitato-99mTcO4, na marcação e morfologia de hemácias e em parâmetros metabólicos. Métodos: Ratos Wistar foram distribuídos em três grupos (6 animais cada), denominados: colectomia, colectomia+hepatectomia e sham. No 30º dia pós-operatório, em todos eles foi feita injeção de 0,1 mL i.v. de fitato-99mTcO4 (radioatividade 0,66 MBq). Após 15 minutos, uma amostra de fígado foi colhida e pesada. O percentual de radioatividade por grama de tecido (%ATI/g) foi determinado no fígado e hemácias usando-se um contador gama automático. Dosagem sérica de AST, ALT, fosfatase alcalina, morfologia e marcação de hemácias com pertecnetato foram determinadas. Resultados: O %ATI/g no fígado e nas hemácias foi menor nos animais dos grupos colectomia e colectomia+hepatectomia do que no grupo sham (p<0,05; teste de Tukey). Nenhuma diferença foi detectada comparando os grupos colectomia e colectomia+hepatectomia. A morfologia das hemácias não diferiu entre os 3 grupos. Os níveis séricos de AST, ALT e fosfatase alcalina foram significativamente maiores no grupo colectomia+hepatectomia do que no grupo colectomia (p<0,001). Conclusão: A colectomia associada a hepatectomia contribuiu para reduzir a 19 captação de radiofármaco no fígado e hemácias de ratos, coincidindo com alterações na atividade enzimática do fígado. Descritores: Colectomia. Hepatectomia. Metabolismo. Biodisponibilidade. Radiofármaco. INTRODUCTION The liver is affected by metastases in 50% of patients with colorectal cancer and metastatic disease remains the leading cause of cancer-related death. The metastases may be single or multiple, affecting one or both hepatic lobes and are synchronous with the primary tumor in 16 to 25% of cases, several months or years after diagnosis1. The surgical resection of liver metastases is possible in 10 to 15% of patients and it is considered the treatment of choice with potential for cure and five-year survival in 22 to 65% of cases2. One of the most widely used diagnostic tools in identifying diseases and metabolic changes, uses radiopharmaceuticals. On nuclear medicine, pertechnetate (99mTcO4-) is used in the diagnosis of gastric, kidney, liver, lung, intestinal, skeletal, endocrine, heart, blood flow and postoperative disorders3. Used intravenously, this radiopharmaceutical remains in the circulation long enough to analyse various organic and functional parameters for the diagnosis of diseases. Gradually it comes into equilibrium with the extracellular space, is taken up by tissues, and a small percentage is eliminated by urinary excretion. The 99m TcO4- is used in approximately 85% of diagnosis procedures, has low cost and small environmental impact3. Some recent studies have demonstrated significant changes in biodistribution of 99m TcO4- on the postoperative of major surgery4-8. In nuclear medicine, red blood cells can be labeled by 99m TcO4-, and used to detect certain clinical disorders, digestive bleeding, blood flow, heart perfusion, etc9. The labeling of blood constituents with 99m TcO4- has been used as a tool in experimental studies in vitro and in vivo, in order to demonstrate the interaction between drugs and radiopharmaceuticals18. The labeling of red blood cells involves intracellular reaction between 99m TcO4- and hemoglobin. It is often used to evaluate pulmonar perfusion10, digestive bleeding, liver tumors and hemodynamic disorders11. It has been shown that changes on the morphology of red blood cells may arise in the first hours after trauma, persists for several days and may interfere with the their 20 labeling. These changes are more severe in patients with postoperative septic complications12. Any deviation in the uptake of radiopharmaceuticals, on vital organs and red blood cells after surgery, can result undesirable interpretations in the results of scintigraphic examinations, leading to mistaken diagnoses, with serious consequences to the patients. Repetition of the exams can determine an increase of radiation dose for patients and risk for the involved professionals. This work is part of a research field that has been studying the consequences of major surgery performed in organs of the digestive system. We have demonstrated relevant postoperative metabolic disorders after massive intestinal resection4, total gastrectomy5,6, total colectomy7 and Roux-en-Y gastric bypass8, by using this experimental model. Based on the above concepts, this study aimed to examine in an animal model if colectomy associated with hepatectomy modifies liver biodistribution of 99m Tc- phytate, metabolic parameters and labeling of red blood cells. METHODS Eighteen Wistar rats weighing 285±23g, were housed in polypropylene cages and kept under controlled conditions of temperature in a clear-dark cycle of 12 hours and allowed ad libitum access to food (Labina, Purina ®) and water. All experimental procedures in animals were conducted according to the code of ethics for animal experimentation of the Council for International Organization of Medical Sciences and the Brazilian Law on the Scientific use of Animals (Law No. 11794). The protocol was approved by the Institutional Research Ethics Committee. The anesthesia was accomplished with intraperitonial injection of 0,2ml/100g of a solution containing 1ml of ketamine (50mg) and 1 ml of xilazine (20 mg) and operated under aseptic conditions. In addition, analgesia (tramadol 20 mg/kg body weight) was applied subcutaneously immediately after surgery and every 12 hours for three days. The animals from group colectomy underwent laparotomy and a subtotal colectomy was performed, proceeding ileocolic anastomosis with 6-0 polypropilene suture. Cecum, 5 cm of colon and 10 cm of ileum were resected. The laparotomy was closed in layers with 4-0 mononylon. In the group colectomy+hepatectomy the rats were submitted to partial colectomy associated to resection of the left lobe of the 21 liver. In the group sham, we performed medium laparotomy and soft manipulation of the intestine. The animals were weighed weekly and remained under observation. After 30 days they were anesthetized, the femoral vein was dissected and 0.1 mL of 99m Tc- phytate was injected i.v. (radioactivity 0.66 MBq). After 15 minutes, 5 mL of blood were harvested by cardiac puncture and the rats were killed with an overdose of anesthetic (sodium thiopental 100mg/Kg). A sample of liver was harvested to examine the biodistribution of 99mTc-phytate. After centrifugation of 2 mL of blood, red blood cells were separated for examination of in vivo labeling with pertechnetate and morphology. The liver samples were isolated, washed with 0.9% saline solution and weighed with a precision scale (Bel-Mark 160-II-Italy). The detection of liver radioactive uptake was determined using an automatic gamma counter, Wizard 1470 (PerkinElmer, Finland). The percentage of radioactivity per gram of tissue (%ATI/g) was calculated dividing the activity of the liver sample by the total activity administered to each animal. The experiment with radiopharmaceutical was carried out in compliance with radiation protection standards recommended by the Comissão Nacional de Energia Nuclear. The radiopharmaceutical was provided by Department of Nuclear Medicine of Liga Norte-Riograndense Contra o Câncer (LIGA) and the radioactive waste returned to the LIGA for proper treatment. Assay for biochemical levels Samples of blood (3 mL) were inserted into test tubes without anticoagulant, centrifuged to 3000 rpm by 10 min and the serum was stocked to -40°C until analysis. Serum levels of aspartate aminotransferase (AST), alanine aminotransferase (ALT), and alkaline phosphatase were measured using a commercial kit on the autoanalyzer (Konelab, Software Version, 60i, Finland). Red blood cells morphology Blood strains were prepared on slides, them stained with Leishman. The images of red blood cells were captured by digital camera using optical microscopy (Olympus microscope, model BX50, Japan, 1000x,) for analysis. To take the shape of red blood cells and the morphometric measurements we used the ImagePro Plus Software, version 6.0. 22 Estatistics Data were expressed as mean±sd. The comparison between groups was performed by analysis of variance (ANOVA) and by the multiple comparison test of Tukey, using a 0.05 significance. RESULTS The animals were randomly divided into three groups of six each. We observed 8% weight loss in group colectomy+hepatectomy at the end of first week. A progressive recovery of weight occured until day 30. In the other groups there was no weight loss after surgery. At the end of the experiment there was no significant difference in mean weights among groups. Table 1 shows the results of the percentage of radioactivity per gram of tissue (%ATI/g), found in red blood cells and liver, as well as the tests to investigate the statistical differences among the groups colectomy, colectomy+hepatectomy and sham. Table 1 - 99mTc-phytate biodistribution studies for each group. Groups Organ (%ATI/g)1 Red blood cells2 Liver2 Colectomy 0.21 ± 0.04 4.35 ±0.71b Colectomy + hepatectomy 0.16 ± 0.02a 4.41 ±0.56a Sham 0.22 ± 0.05a 5.70 ± 0.87ab 0.042 0.024 p-value Mean±Standard deviation 1. Percent of radioactivity per gram of tissue 2. Dosages in each column, followed by the same letter differ significantly (Tukey test). Rats from colectomy and colectomy+hepatectomy groups had significantly lower 99m 99m Tc-phytate uptake in the liver than in the sham group rats (p=0.024). The Tc-phytate uptake in the liver of colectomy rats was higher than in the colectomy+hepatectomy group rats, but the difference was not significant (p>0.05). Concerning the erythrocytes labeling, we observed a significant difference in %ATI/g 23 when the colectomy+hepatectomy group rats were compared with sham rats (p=0.042). These data are summarized in table 1. Table 2–Serum levels of liver enzymes and alkaline phosphatase in colectomy, colectomy+hepatectomy and sham rats. Groups Colectomy Colectomy + hepatectomy Sham AST (u/L)1 ALT (u/L)1 Alkaline phosphatase (u/L)1 37,67 ± 1,37a 47,33 ± 2,50a 170,6± 22,91b 155,00 ± 13,67ab 76,33 ± 6,89a 232,3 ± 28,93ab 44,33 ± 4,72b 51,17 ± 3,19 180,7 ± 20,35a <0,001 <0,001 <0,001 p-value Mean ± Standard deviation 1. Dosages in each column, followed by the same letter, differ significantly (Tukey test). AST, aspartate animotransferase; ALT, alanine aminotraferase Serum levels of AST, ALT and alkaline phosphatase were significantly higher in colectomy+hepatectomy rats than in colectomy group rats (p<0.001), signaling that hepactectomy contributed to these results. Comparing the serum levels of AST, ALT and alkaline phosphatase from colectomy group with sham rats, the results were similar (p>0.05) (Table 2). The qualitative and quantitative evaluation of the shape of red blood cells under optical microscopy was performed and alterations on the shape and morphometric measures were not found, when compared the three groups (Figure 1). A B C Figure 1 – Photomicrography of red blood cells from (A) colectomy, (B) colectomy +hepatectomy and (C) sham rats. 1000x. 24 DISCUSSION It is well established in the area of digestive surgery that surgical resection is the most effective treatment for isolated liver metastasis in patients with colorectal cancer13. Perioperative morbidity and mortality does not differ between simultaneous resections and staged procedures for selected patients with liver metastases. Meanwhile, patients undergoing simultaneous resections could expect a short duration of surgery and postoperative hospitalization as well as less blood loss during surgery13. Although the treatment for patients with synchronous colorectal cancer liver metastases remains controversial, surgical resection of both the primary tumor and liver metastases is the only option offering a potential cure13. In the experimental model used in this work we did not include induction of colon cancer, because our objective was to examine the repercussion of colectomy associated partial hepatectomy without carcinogenesis. After the standardization of the technique in the pilot study, the morbidity was low and there was not mortality during the 30 days of observation of all rats. Despite the great surgical trauma, the animals progressed well until the end of the experiments. Weight loss in the first week was observed in the animals from colectomy+hepatectomy group, but they had a satisfactory recovery in the three subsequent weeks. These findings corroborate the statement that hepatectomy increased morbidity, but over time the animals had satisfactory evolution. However, at the end of the observation and collection of biological samples, we detected significant changes in some parameters, when the groups were compared. There was a significant reduction in 99m Tc-phytate biodistribution in the liver of colectomy+hepatectomy animals, compared with the sham group, but no difference was observed comparing with colectomy group. This finding may be interpreted based on the hypotesis that after 30 days liver regeneration was sufficient to compensate any disfunction, normalizing the 99mTc-phytate uptake. The distribution of radiocolloids in the liver has been shown to correlate well with the severity of chronic liver diseases, the severity of histologic fibrosis, prognosis, and hepatic function14. Thus, liver uptake of 99m Tc-phytate colloid provides a practical index of hepatic function and image, by using planar scintigraphy techniques15. In a study from our laboratory it was demonstrated that in splenectomized rats the biodistribution of 99mTc-phytate to the liver was higher than in 25 controls, suggesting that the operation favored the hepatic uptake of the radiopharmaceutical. This result coincided with the improvement in liver function, confirmed by the better alanine aminotransferase, aspartate aminotransferase and lactic dehydrogenase activities in splenectomized rats, compared with controls16. Otherwise, in the present study the lower liver lower alanine aminotransferase, 99m aspartate Tc-phytate uptake coincided with a aminotransferase and alkaline phosphatase activities in colectomy+hepatectomy rats, than in sham rats. Nuclear medicine procedures have proven increasingly effective imaging modalities in the study of several disorders17. Besides the disease, these procedures could be altered by medications, surgery and natural products that could change the biodistribution of radiopharmaceuticals in a specific target or the fixation of 99m Tc to blood constituents16,18. In general, the labeling of blood constituents could decrease by the action of drugs and trauma:(a) changing of the cellular membrane structure or modifying the transport systems of pertechnetate ions into cells, (b) by direct oxidation or generation of free radicals, (c) by direct inhibition (chelating action) of pertechnetate ions, or (d) binding at the same sites on the blood constituents3. In this study we observed that pertechnetate labeling of red blood cells of the colectomy+hepatectomy rats was lower than in sham rats. This data is relevant, because red blood cells labeling is an important method for diagnosis of digestive and renal bleeding19. Interactions of some factors resulting from hepatic resection may be involved with the ion transport systems of pertechnetate ions, decreasing the labeling of red blood cells with pertechnetate. This could in part, explain the data obtained. CONCLUSION In conclusion, hepatectomy associated with colectomy lowered the liver and erytrocytes uptake of pertechnetate in rats, coinciding with changes in hepatic enzymatic activity. 26 REFERENCES 1. Lochan R, White SA, Manas DM. Liver resection for colorectal liver metastasis. Surg Oncol. 2007;16:33–45. 2. Lee WS, Yun SH, Chun HK, Lee WY, Kim SJ, Choi SH, Heo JS, Joh JW, Choi D, Kim SH, Rhim H, Lim HK. Clinical outcomes of hepatic resection and radiofrequency ablation in patients with solitary colorectal liver metastasis. J Clin Gastroenterol. 2008;42:945–9. 3. Arano, Y. Recent advances in 99mTc radiopharmaceuticals. Ann Nucl Med 2002, 16:79-93. 4. Chacon DA, Araujo Filho I, Villarim Neto A, Medeiros AC. Biodistribuição do radiofármaco pertecnetato de sódio (Na99mTcO4) em ratos submetidos a ressecção extensa de intestino delgado. Acta Cir Bras. 2007;22: 430-5. 5. Medeiros AC, Filho IA, Medeiros VB, Pinheiro LA, Freire FH, Azevedo IM, Brandão-Neto J. Comparing reconstruction with ileocecal graft to jejunal interposition pouch after total gastrectomy in rats. J Invest Surg. 2007;20:41-8. 6. Rêgo AC, Villarim Neto A, Azevedo IM, Araújo-Filho I, Egito ES, Medeiros AC. Biodistribution of Technetium-99m pertechnetate after total gastrectomy and Roux-en-Y jejunal pouch. J Invest Surg. 2010;23:94-100. 7. Rêgo AC, Ramalho RA, Egito ES, Araújo-Filho I, Azevedo IM, Palestro CJ, Medeiros AC. Biodistribution of technetium-99m pertechnetate after total colectomy in rats. Appl Radiat Isot. 2010;68:2169-73. 8. Rêgo AC, Araújo-Filho I, Azevedo IM, Jácome DT, Ramalho R A, Medeiros AC. Biodistribution of technetium-99m pertechnetate after Roux-en-Y gastric bypass (Capella technique) in rats. Acta Cir Bras. 2010;25:9-12. 9. Zink SI, Ohki SK, Stein B, Zambuto DA, Rosenberg RJ, Choi JJ, Tubbs DS. Noninvasive evaluation of active lower gastrointestinal bleeding: comparison between contrast-enhanced MDCT and 99mTc-labeled RBC scintigraphy. Am J Roentgenol. 2008;191:1107-14. 10. Hunt A, Frier M, Johnson R, Berezenko S, Perkins A C. Preparation of Tc99m-macroaggregated albumin from recombinant human albumin for lung perfusion imaging. Euro J Pharm Biopharm. 2006; 62: 26-31. 11. Schneider A, Attaran M, Gratz K F, Bleck J S, Winkler M, Manns M P, Ott M. Intraportal infusion of 99m technetium-macro-aggregrated albumin particles and 27 hepatocytes in rabbits: assessment of shunting and portal hemodyn changes. Exp Transplant. 2003; 75: 296-302. 12. Berezina T L, Zaets S B, Machiedo G W. Alterations of red blood cell shape in patients with severe trauma. J Trauma-Injury Infect Crit Care. 2004; 57: 82-7. 13. Jong M, van Vledder M, Ribero D, Hubert C, Gigot J, Choti MA, Schulick RD, Capussotti L, Dejong CH, Pawlik TM. Therapeutic efficacy of combined intraoperative ablation and resection for colorectal liver metastases: an international, multi-institutional analysis. J Gastrointest Surg. 2011;15:336–44. 14. Hoefs JC, Wang F,Kanel G. Functional measurement of nonfibrotic hepatic mass in cirrhotic patients. Am J Gastroenterol. 1997; 92:2054–8. 15. Kikuchi M, Tomita K, Nakahara T, Kitamura N, Teratani T, Irie R, Yokoyama H, Suzuki T, Yokoyama T, Taguchi T, Tanaka S, Noguchi M, Ohkura T, Hibi T. Utility of quantitative 99mTc-phytate scintigraphy to diagnose early-stage nonalcoholic steatohepatitis. Scand J Gastroenterol. 2009;44:229-36. 16. Pereira KRSG, Açucena MKMT, Villarim-Neto A, Rêgo ACM, Bernardo-Filho M, Azevedo IM, Medeiros AC. Biodistribution of the radiopharmaceutical technetium-99m-sodium phytate in rats after splenectomy. Braz Arch Biol Technol. 2008;51:203-7. 17. Lodge MA, Braess H, Mahmoud F, Suh J, Englar N, Geyser-Stoops S, Jenkins J, Bacharach SL, Dilsizian V. Developments in nuclear cardiology: transition from single photon emission computed tomography to positron emission tomography-computed tomography. J Invasive Cardiol. 2005;17:4916. 18. Fonseca AS, Frydman JN, Rocha VC, Bernardo-Filho M. Acetylsalicylic acid decreases the labeling of blood constituents with technetium-99M. Acta Biol Hung. 2007; 2:187-98. 19. Howarth DM. The role of nuclear medicine in the detection of acute gastrointestinal bleeding. Semin Nucl Med. 2006;36:133-46. Correspondence: Aldo Cunha Medeiros ([email protected]) Av. Nilo Peçanha 620, Natal-RN, Brazil 59012-300 Conflict of interest: none. Financial source: CNPQ 28 5.2. Artigo publicado no periódico Journal of Investigative Surgery. 2011;24:109-14. (Qualis B1). ISSN 0894-1939 Metabolism and gastric remnant changes after Roux-en-Y Gastric Bypass in rats. Aldo Cunha Medeiros, Amália Cínthia Meneses Rêgo, Ítalo Medeiros Azevedo, Marília D. Ferreira Carvalho, Vítor Brasil Medeiros, Irami Araújo-Filho. Department of Surgery, Postgraduate Program in Health Sciences, Federal University of Rio Grande do Norte, Natal, Brazil. ABSTRACT Background: The Roux-en-Y gastric bypass (RYGB) may affect gastric microbiology as well as the histology of the excluded stomach. Therefore, this study aimed to investigate these issues in rats. Methods: Twelve rats were randomly allocated to a RYGB group (n=6) and nonoperated control group (n=6). After 30 postoperative days, all rats were killed. Samples of the remnant stomach mucosa were harvested for bacterial and fungal count such as colony-forming units/g and histology. Results: The excluded stomach mucosa of RYGB rats showed higher bacterial and fungal count, atrophy, intestinal metaplasia and neutrophilic polymorphonuclear inflammation than in controls. Conclusions: This work showed that a model of murine RYGB significantly modified the microbiota/histology of the excluded stomach. Keywords: Bariatric surgery, Gastric microbiology, Histology, Roux-en-Y gastric bypass, Rats INTRODUCTION Morbidity and mortality are strongly correlated to the level of obesity [1], and the list of diseases with a causal factor for obesity continues to expand. The failure of most current approaches to control morbid obesity has led to the development of surgical techniques for the upper gastrointestinal tract designed to induce weight loss 29 (bariatric surgery). Patients have achieved effective weight loss after bariatric surgery and most have had complete resolution or improvement of their diabetes, hypertension, hyperlipidemia, and obstructive sleep apnea [2], in addition to reduced long-term mortality [3]. The Roux-en-Y gastric bypass (RYGB) is the predominant approach used in the United States [4] and Brazil [5]. After the adoption of RYGB, occasional concern has arisen regarding bacterial overgrowth in the upper digestive tract, especially in the excluded stomach. Gastric juice is an important barrier against bacterial colonization and an essential component of the gut barrier, which protects the organs from infection when vagal innervation is lost [6]. Although the procedure can be successful, it is associated with a number of metabolic and structural complications. These complications are sometimes subtle and difficult to diagnose early. Since these patients have limited physiologic reserve, it is imperative that complications are identified early by image procedures and appropriately managed [7]. One of the most widely used diagnostic methods in identifying a great number of diseases and metabolic disorders is the use of radiopharmaceuticals, radioactive compounds used in diagnostic procedures as sources of radiation and tracers. Examination of gastric emptying, liver function, thyroid function, bone disorders, etc, are often used in patients undergoing bariatric surgery. Radiopharmaceutical biodistribution may provide important information about their uptake to target organs and their function, but post-surgery data are scarce [8]. It is important to investigate the biodistribution of technetium-99m pertechnetate after RYGB, since it is highly secreted by gastric mucosa. After this operation the stomach is mostly bypassed, the metabolism is affected, and changes in biodistribution are expected. Drugs and surgery may interfere in the biological behavior of radiopharmaceuticals used in scintigraphy and single photon emission computed tomography (SPECT). Technetium-99m pertechnetate is used in more than 80% of scintigraphic examinations [9-11]. Thus, the biological effects of technetium-99m pertechnetate and its uptake to various organs may be altered. RYGB is a major surgery and may therefore result in important anatomical and metabolic changes as well as unpredictable complications [7]. Accordingly, scintigraphic studies may be needed in the postoperative period. Given that the biodistribution of technetium-99m pertechnetate is expected to cause changes in important organs and tissues due to bariatric surgery, scintigraphic examinations 30 may produce false-positive or false negative images, leading to repetition of nuclear medicine procedures with unnecessary radiation exposure for patients. The aim of this study was to analyze the effects of RYGB on gastric microbiology, metabolism, histology and technetium-99m pertechnetate biodistribution in rats. METHODS The use of laboratory animals followed the Council for International Organization of Medical Sciences Ethical Code for animal experimentation and the Brazilian guidelines for the scientific use of animals (Law no. 11.794). The protocol was approved by the Institutional Research Ethics Committee. Rats were observed in individual polypropylene cages at room temperature of 24ºC, relative humidity of 45%, 12-hour light/dark cycles, with food and water ad libitum. For preoperative procedures, rats were deprived of food for 16 to 18 hours and anesthetized with a mixture of ketamine and xylazine (200 mg: 5 mg, 0. 8 ml/kg, intraperitoneally). For postoperative pain control, 1.5 mg/kg of tenoxicam (Roche, Brazil) was administered subcutaneously, once a day for 3 days. Operative and laboratory procedures Twelve Wistar rats (349.3 ±10.7 g) were equally divided into RYGB and control groups. The rat abdomens were shaved and prepared with 70% alcohol. All the surgical procedures were carried out by the same well-trained investigator, experienced in animal surgery. Three previous series of experiments were conducted in sequence to develop the RYGB model. A midline incision was made, exposing the stomach and distal esophagus. The stomach was divided 2 cm below the esophagus and both gastric ends were oversewn using a running 6-0 polypropylene suture. The suture lines were then embrocated. The jejunum was divided 16 cm below the ligament of Treitz, creating a 16 cm biliary-pancreatic limb. A 4 to 5 mm end-to-side gastrojejunostomy was sewn using interrupted 6-0 polypropylene sutures on the anterior surface of the gastric fundus. The stump of the proximal jejunum was closed with a running suture. A 7 to 8 mm side-to-side jejunojejunostomy was sewn 10 cm below the gastrojejunostomy. The procedure lasted approximately 30 minutes, after 31 which the abdomen was closed in layers, using a running 4-0 nylon suture. Rats drank water and a 10% glucose plus 2% saline solution starting 24 hours after the operation and for the first 3 days. This was followed by a solid diet (Labina-Purina®). For the first three postoperative days, rats were hydrated with normal saline solution (20ml) injected subcutaneously to prevent dehydration. A surgical microscope with 10x magnification (DF Vasconcelos, São Paulo, Brazil) was used for anastomosis. The control group rats (n=6) were not operated. The animals remained under observation for 30 days after surgery and under anesthesia, injected with 0.1 ml of technetium-99m pertecnetate via the orbital plexus, corresponding to radioactive activity of 0.66 MBq. Thirty minutes after radiopharmaceutical administration, blood samples were obtained by cardiac puncture to determine serum dosages. Furthermore, a midline laparotomy was performed under sterile conditions. The defunctionalized stomach was opened and intragastric material (including mucosa) was harvested for culture. Samples were collected from the nonoperated stomach of control rats. Samples were then removed from the liver, kidney, heart, lung, thyroid, stomach and femur. The tissue samples were washed in 0.9% saline and weighed on a precision scale (Mark 160®, Bel equipment, Italy). Radioactivity was determined in an automatic gamma counter (Wizard 1470®, Perkin-Elmer, Finland). The results were shown in counts per minute (CPM), corrected by disintegrations per minute (DPM). The efficiency of the gamma counter was 86%, as specified by the manufacturer. The specific activity of each sample was calculated by dividing absolute count in DPM by weight (DPM/g). The percentage radioactivity of each sample (% ATI/g) was calculated by dividing its specific activity (DPM/g) by the total radioactivity of each animal. Laboratory tests Blood samples were centrifuged immediately at 3000 rpm for 10 min. and serum samples stored at -80°C until analysis. Serum albumin, calcium, alanine (ALT) and aspartate aminotransferase (AST) levels were assayed using a Konelab 60i analyzer (assay kit from Weiner, São Paulo, Brazil). The levels of free triiodothyronine (T3), free thyroxin (T4) and parathyroid hormone (PTH) were determined by radioimmunoassay using an [I125] and PTH assay kit (Diagnostic Products, Los Angeles, USA). Sensitivity was determined to be 0.4 ng/dL. 32 Microbiological analysis The excluded stomach was opened and antral specimens (5 mm punchbiopsy) for bacterial quantification were obtained on day 30. In control rats, samples were harvested from the antrum of the non operated stomach. They were then individually weighed and homogenized in 1 ml of sterile 0.9% saline solution using a sterile technique. Serial dilution was performed, and samples were plated onto trypticase soy agar containing 5% sheep blood agar for colony counts of viable aerobic bacteria. Aliquots were spread on blood/agar plates for Gram positives and agar McConkey for Gram negative bacteria. Incubation proceeded at 37˚C for 48 h. The number of colony-forming units (CFU)/g was counted in 100-µl aliquots of fluid. Fungi were inoculated in acidified agar/dextrose/potato plates, and incubation proceeded at 25˚C for 7 days. The number of colonies was computed by colony counter, and all colony counts were expressed as the number of colony-forming units per gram of tissue (CFU/g). Statistical analysis The data were expressed as mean ± standard deviation. Statistical analysis for group comparison was performed using the Student t test, at a significance level of 0.05. RESULTS All animals survived the study. Table 1 summarizes the descriptive results of percentage radioactivity (% ATI) in the organs of rats from groups RYGB and control. 33 Table 1. Percentage radioactivity (% ATI/g) of each organ sample in animals submitted to Roux-en-Y gastric bypass and controls. Organs %ATI/g P RYGB Control Liver 0.32 ± 0.04 0.57 ± 0.06 0.023 Kidney 0.57 ± 0.21 0.43 ± 0.06 0.120 Heart 0.22 ± 0.05 0.26 ± 0.08 0.131 Lung 0.52 ± 0.17 0.39 ± 0.16 0.099 Tyroid 2.97 ± 0.98 3.42 ± 1.68 0.530 Stomach 0.53 ± 0.31 2.95 ± 1.64 0.005 Femur 0.13 ± 0.03 0.25 ± 0.07 0.026 The values appear as mean±standard deviation. RYGB, Roux-en-Y gastric bypass. In the kidney and lung we observed an increase in radioactivity uptake in rats submitted to RYGB, compared with controls, but the difference was not statistically significant (p>0.05). However, in the RYGB rats a significant decrease in the radioactivity uptake (%ATI/g) occurred in the stomach, liver and femur, compared with controls (p<0.05). A comparison between radioactivity uptake in the heart and thyroid of RYGB and control rats showed a tendency for a further decrease in % ATI/g in RYGB animals, although it was not statistically significant (p>0.05). Table 2 shows a significant reduction mean serum albumin and calcium levels in animals undergoing RYGB surgery, compared with those of the control group (p <0.05). Liver function tests (ALT and AST) revealed a significant difference between the two groups. T3 and T4 levels were significantly lower in RYGB rats than in control rats (p=0.002 and 0.016 respectively). However, PTH levels were significantly higher in RYGB rats than in controls (p=0.009) (Table 2). 34 Table 2. Comparison of control and RYGB postoperative laboratory values. Control RYGB p-valor Albunin (g/dL) 3.2±0.7 2.3±0.2 0.048 Calcium (mg/dL) 8.2±1.4 5.3±1.1 0.031 ALT (U/L) 97.3±18.5 57.6±14.2 0.045 AST (U/L) 47.3±12.7 33.7±10.5 0.048 T3 (ng/dL) 28.7±4.10 16.3±3.06 0.002 T4(ng/dL) 31.4±2.01 20.1±2.13 0.016 PTH (pg/mL) 59.3±1.96 65.7±2.5 0.009 Results are shown in means ± SD. ALT, alanine aminotransferase; AST, aspartate aminotransferase; T3, free triiodothyronine; T4, free thyroxin; PTH, parathyroid hormone; RYGB, Roux-en-Y gastric bypass. Quantification of microorganisms The homogenate fluid of the excluded stomach of RYGB rats showed a high bacterial count on postoperative day 30, with 46033.33 ± 18369.29 CFU/g of tissue. Control rats showed significantly lower counts (11100 ± 1678.09 CFU/g; p = 0.005), compared to RYGB rats. On day 30 we detected 190.00 ± 19.75 CFU/g of fungi in the homogenate fluid of the excluded stomach of RYGB rats. A lower fungi count of 38.23 ± 9.93 CFU/g was found in the control rats (p < 0.001). Microorganisms were identified as Escherichia coli, Staphylococcus sp. and Klebsiela sp. Fungi were predominantly Candida spp. These data are summarized in table 3. Table 3. Comparison of control and RYGB postoperative gastric bacteria and fungal counts. Bacteria and fungi Bacteria (CFU/g) Fungi (CFU/g) Group RYGB 46033.33 18369.29 190.00 ± 19.75 Control ± p-valor(1) 11100.00 ± 1678.09 0.005 38.23 ± 9.93 <0.001 1 - P-valor, Student t test for independent data; Numbers indicate colony forming units per g (CFU/g) of tissue. 35 Histology We determined the effects of RYGB on the mucosa of the excluded stomach. Histological examination revealed mucosal atrophy with reduced tissue and cell size. Atrophy affected the glands, which were sparse and small (Figure 1). The difference between the two groups was significant (p=0.01). Intestinal metaplasia occurred in one RYGB rat. We found the simultaneous presence of intraepithelial mononuclear cell infiltrate and neutrophilic polymorphonuclear inflammation in all the excluded stomachs. Prominent numbers of eosinophils were observed in the antral mucosa of two RYGB rats. Mean inflammatory cell density and mucosal thickness related to these findings are summarized in table 4. Table 4 – Histologic findings expressed as mean cell density and mucosal thickness. Group Parameters Inflammation Mucosal length (mµ) p-valor(1) RYGB Control 20045± 97 4130 ±104 0.005 95 ± 11 173 ± 14 0.01 1 - P-valor, Student t test for independent samples; Numbers indicate mean inflammatory cell density and mucosal thickness (mµ). DISCUSSION Significant efforts have been made to obtain good results with surgical techniques, and patients subjected to bariatric operations have achieved significant 36 weight loss [12]. Despite these promising results, bariatric surgery may lead to anatomical and metabolic complications [13]. A literature survey shows that severe disease can affect the bypassed stomach after RYGB. Following this surgery conventional gastroscopy cannot assess the excluded stomach, which may result in delayed diagnosis of gastric disease. Perforated peptic ulcer [14] and gastric cancer have been reported [15]. The diagnosis of these disorders may require imaging examinations such as radiography, endoscopy and scintigraphy. Technetium-99m is the most widely used radionuclide in nuclear medicine and research studies. It has a short half-life (6h), emits low radiation and requires small doses for diagnostic procedures [18]. Changes in the biodistribution of technetium-99m pertecnetate in organs and tissues are well identified in a number of clinical studies. It has been used in vivo and in vitro, in the study of diseases, drugs and chemotherapy that interfere with its distribution [16,17]. However, few studies have focused on radiopharmaceutical biodistribution in the postoperative period of major surgery. To understand and explore the relationship between the RYGB and radiopharmaceutical biodistribution in organs and tissues, we used a reproducible and well characterized animal model. Scintigraphic examinations in the postoperative period are used to diagnose gastrointestinal tract bleeding, gastroesophageal reflux and patency of anastomosis. Diagnosis of postoperative changes in the kidneys, liver, lung, heart and other organs are performed using scintigraphy and SPECT with radiotracers and technetium-99m pertecnetato [18]. In this study, the RYGB did not affect the biodistribution of technetium-99m pertecnetate in the heart, lungs, kidneys and thyroid. The stomach is often examined in the postoperative period of bariatric surgery, primarily for diagnosing the presence of fistulas, since escape from the anastomosis may be an early or late complication of this operation. A case series of 63 patients with leaks after RYGBP reports that most were not detected by CT imaging and that most required surgery (63%), with morbidity of 53% and mortality of 10% [19]. In the case of small fistulas, since the rate of escape of contrast medium is low, leaks may be overlooked by radiography. It has been suggested that scintigraphy is highly accurate in diagnosing gastroparesis and other postoperative complications of postoperative bariatric surgery [20]. In this study the pertechnetate uptake was significantly lower in the remnant functional stomach after RYGB. Therefore, 37 scintigraphic examination of this organ in the postoperative period of bariatric surgery must be interpreted considering this finding. Several different mechanisms may explain the changes in bone metabolism observed after bariatric surgery. Poor mineral and vitamin absorption, including calcium and vitamin D, has been documented [21]. In this study we detected low levels of serum calcium in the RYGB rats. Consistent data have been reported suggesting that secondary hyperparathyroidism occurs after gastric bypass. Elevated and these levels persisted after 6 months of calcium and vitamin D supplementation [22]. In our RYGB rats we demonstrated higher levels of PTH compared with controls, and there is evidence that the increase in PTH may be progressive [23]. Higher turnover and reduced bone mineral density may occur as a physiological adaptation to weight loss and changes in skeletal mechanics or as a result of pathophysiological responses to surgery [24]. The metabolic changes in calcium and PTH may, at least in part, explain the decreased biodistribution of technetium-99m pertecnetate in the femur of animals submitted to RYGB compared to the control group. In our study the uptake of technetium-99m pertecnetate by the liver of RYGB rats was significantly lower than in controls, indicating that liver function may have been affected, as suggested by our data. caution. Indeed, some authors These results should be viewed with demonstrated significant improvement in aminotransferase and gamma glutamyl transferase levels in the postoperative period of patients submitted to RYGB [25], and others found transiently higher postoperative aminotransferase values (five to eightfold) [26]. The rat model for RYBG, which seems to be reasonably reliable, will enable continued research into metabolic changes, aimed at validating postoperative metabolic findings. Bacterial concentrations were consistently higher in the gastric biopsy homogenate of the bypassed stomach than in the control organ. This finding is in disagreement with the results described by Ishida et al. [27], who studied the bacterial count of intragastric fluid endoscopically harvested in patients. However, our data indicate that the assessment and quantification of bacteria in intragastric fluid may reflect different results, when compared with the bacterial count of mucosal biopsy homogenates. These data support the hypothesis that the use of intragastric fluid for diagnosis of infection may be insufficient and if possible, should be replaced by tissue biopsies. It has been demonstrated that Candida albicans is able to colonize the murine alimentary tract, as well as adhere to and penetrate gastric 38 tissues [28]. In this study, we observed Candida spp colonization in the bypassed stomach. This evoked a prominent, granulocyte-dominated, inflammatory response in the gastric mucosal tissues. In the present study, antral mucosal atrophy affected primarily the glands, which became sparse and small. In some specimens, mucosal thinning was non-apparent, likely due to accompanying inflammation characterized by the simultaneous presence of mononuclear and neutrophilic polymorphonuclear infiltrate. The occurrence of chronic gastritis and intestinal metaplasia has been confirmed in the excluded stomach [29,30], but the clinical significance of these histological changes remains obscure. In conclusion, the current investigation demonstrated that a murine model of RYGB modified the biodistribution pattern of technetium-99m pertechnetate, the microbiota/histology of the excluded stomach and the metabolism. REFERENCES 1. Calle EE, Thun MJ, Petrelli JM, et al. Body-mass index and mortality in a prospective cohort of U.S. adults. N Engl J Med. 1999;341:1097–1105. 2. Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292:1724-1737. 3. Adams TD, Gress RE, Smith SC, et al. Long-term mortality after gastric bypass surgery. N Engl J Med. 2007;357:753-761. 4. Livingston EH. Procedure incidence and in-hospital complication rates of bariatric surgery in the United States. Am J Surg. 2004;188:105-110. 5. Campos CD, Dalcanale L, Pajecki D, et al. Calcium intake and metabolic bone disease after eight years of Roux-en-Y gastric bypass. Obes Surg. 2008; 18:386– 390. 6. Martinsen TC, Bergh K, Waldum HL. Gastric juice: a barrier against infectious diseases. Basic Clin Pharmacol Toxicol. 2005; 96: 94-102. 7. Livingston EH. Complications of bariatric surgery. Surg Clin North Am. 2005; 85:853–868. 8. Chacon DA, Araújo-Filho I, Villarim-Neto A, et al. Biodistribution of the radiophamarceutical sodium pertechnetate (Na99mTcO4) after massive small bowel resection in rats. Acta Cir Bras. 2007;22:430-435. 39 9. Moreno S R F, Carvalho J J, Nascimento A L, et al. Bioavailability of the sodium pertechnetate and morphometry of organs isolated from rats: study of possible pharmacokinetic interactions of a Ginkgo biloba extract. Braz Arch Biol Technol. 2005;48:73-78. 10. Xavier-Holanda C M C, Jales R L C, Catanho M T J A, et al. Effects of the glucantime on the kinetic of biodistribution of radiopharmaceuticals in Wistar rats. Cell Mol Biol. 2002;48:761-765. 11. Rêgo AC, Villarim Neto A, Azevedo IM, et al. Biodistribution of Technetium-99m pertechnetate after total gastrectomy and Roux-en-Y jejunal pouch. J Invest Surg. 2010;23:94-100. 12. Hutter MM, Randall S, Khuri SF, et al. Laparoscopic versus open gastric bypass for morbid obesity: a multicenter, prospective, risk-adjusted analysis from the National Surgical Quality Improvement Program. Ann Surg. 2006;243:657–662. 13. Leea CW, Kellyb JJ, Wassef WY. Complications of bariatric surgery. Curr Opin Gastroenterol. 2007;23:636–643. 14. Macgregor AM, Pickens NE, Thoburn EK. Perforated peptic ulcer following gastric bypass for obesity. Am Surg. 1999; 65: 222-225. 15. Lord RV, Edwards PD, Coleman MJ. Gastric cancer in the bypassed segment after operation for morbid obesity. Aust N Z J Surg. 1997; 67: 580-582. 16. Bernardo-Filho M, Silva JRM, Reis RJN, et al. Conditions for labeling of Schistosoma mansoni cercaria with technetium-99m. J Nucl Biol Med. 1992;36:56-59. 17. Braga ACS, Oliveira MBN, Feliciano GD, et al. The Effect of Drugs on the Labeling of Blood Elements with Technetium-99m. Curr Pharm Design. 2000;6:1179-1191. 18. Nickel, RA. Radiopharmaceuticals. In: Early, P.J., Sodee, D.B. Principles and practice of nuclear medicine. 2nd ed. London, Mosby Year Book Inc., 1995, p.94114. 19. Gonzalez R, Sarr MG, Smith CD, et al. Diagnosis and contemporary management of anastomotic leaks after gastric bypass for obesity. J Am Coll Surg. 2007;204:47–55. 40 20. Tarakji AM, Morales F, Rovito P. Hepatobiliary scintigraphy as a diagnostic modality for gastroparesis of the bypassed stomach after gastric bypass for morbid obesity. Obes Surg. 2007;17:414-415. 21. Madan AK, Orth WS, Tichansky DS, Ternovits CA. Vitamin and trace mineral levels after laparoscopic gastric bypass. Obes Surg. 2006;16:603-606. 22. Goode LR, Brolin RE, Chowdhury HA, et al. Bone and gastric bypass surgery: effects of dietary calcium and vitamin D. Obes Res. 2004;12:40–47. 23. Johnson JM, Maher JW, DeMaria EJ, et al. The long-term effects of gastric bypass on vitamin D metabolism. Ann Surg. 2006;243:701–704. 24. Johnson JM, Maher JW, Samuel I, et al. Effects of gastric bypass procedures on bone mineral density, calcium, parathyroid hormone, and vitamin D. J Gastrointest Surg. 2005;9:1106-1110. 25. Dixon JB, Bhathal PS, O'Brien PE. Weight loss and non-alcoholic fatty liver disease: falls in gamma-glutamyl transferase concentrations are associated with histologic improvement. Obes Surg. 2006;16:1278-1286. 26. Nguyen NT, Bradley S, Fleming NW, et al. Comparison of postoperative hepatic function after laparoscopic versus open gastric bypass. Am J Surg. 2003;186:4044. 27. Ishida RK, Faintuch J, Paula AM, et al. Microbial flora of the stomach after gastric bypass for morbid obesity. Obes Surg. 2007;17:752-758. 28. Westwater C, Schofield DA, Nicholas PJ, et al. Candida glabrata and Candida albicans; dissimilar tissue tropism and infectivity in a gnotobiotic model of mucosal candidiasis. FEMS Immunol Med Microbiol. 2007;51:134-139. 29. Sundbom M, Nyman R, Hedenström H, Gustavsson S. Investigation of the excluded stomach after Roux-en-Y gastric bypass. Obes Surg. 2001;11:25-27. 30. Safatle-Ribeiro AV, Kuga R, Iriya K, et al. What to Expect in the Excluded Stomach Mucosa after Vertical Banded Roux-en-Y Gastric Bypass for Morbid Obesity. J Gastrointest Surg. 2007; 11:133–137. The authors declare that they have no conflict of interest. 41 5.3. O artigo foi publicado no periódico Journal of Surgical and Clinical Research 2010;1:13-21 (ISSN: 2179-7889) Diabetes and biodistribution of pertechnetate (Na99mTcO4) in rats1 Diabetes e biodistribuição de pertecnetato de sódio (Na99mTcO4) em ratos Ítalo Medeiros Azevedo, Daniele Pimentel Fernandes, Ticiana Cabral da Costa, Irami Araújo-Filho, MD, PhD, Amália Cinthia Meneses Rêgo, PhD, Vítor Brasil Medeiros, Marília Daniela Ferreira Carvalho, Aldo Cunha Medeiros, MD, PhD. 1-Research performed at Nucleus for Experimental Surgery, Department of Surgery, Federal University of Rio Grande do Norte (UFRN), Brazil. Financial support: CNPq, Brazil. Conflict of interest: None. Correspondence address: Ítalo Medeiros Azevedo, Department of Surgery, Federal University of Rio Grande do Norte, at Ave Nilo Peçanha 620, Natal, RN, Brazil, Email: [email protected] Submitted: 25 November 2010. Accepted, after review: 27 December 2010. ABSTRACT Purpose: This study aimed to clarify if diabetes induced in rats changes the biodistribution of the radiopharmaceutical sodium pertechnetate (Na99mTcO4) and, consequently, the accuracy of the scintigraphic exams. Methods: We used 14 male Wistar rats, randomly allocated in 2 group: the diabetic group (D) rats (n=7) were submitted to the induction of diabetes with streptozotocin, and 7 non diabetic rats were used as controls (C). After 7 days, in the 14 animals it was administered 0,1 mL of Na99mTcO4 (0.66 MBq) through orbital plexus and, after 30 minutes, the radiopharmaceutical sodium pertechnetate was evaluated, being compared the uptske of this in the several studied organs of diabetic animals and controls. Results: The biodistribution of Na99mTcO4 was significantly higher in the liver and smaller in the bladder, thyroid and stomach of diabetic mice when compared to the control group rats. Conclusion: Diabetes induced in rats alters the biodistribution of Na99mTcO4, and this finding could have clinical implications on scintigraphic exams. 42 Key words: Bioavailability. Tc 99m Pertechnetate. Diabetes. Streptozotocin. Rats. RESUMO Objetivo: Contribuir para esclarecer se o diabetes induzido em ratos altera a biodistribuição do radiofármaco pertecnetato de sódio (Na99mTcO4). Métodos: Estudo do tipo experimental com utilização de 14 ratos machos Wistar, divididos aleatoriamente em 2 grupos, um grupo submetido à indução do diabetes com estreptozotocina, e o outro somente observado. Após 7 dias, nos 14 animais foi administrado 0,1 mL de Na99mTcO4 (0.66 MBq) via plexo venoso orbital e, após 30 minutos, foi avaliada a biodistribuição do radiofármaco, comparando-se a captação deste nos diversos órgãos estudados de animais diabéticos e controles. Resultados: A biodistribuição do Na99mTcO4 foi significativamente maior no fígado e menor na bexiga, tireóide e estômago de ratos diabéticos quando comparados aos ratos do grupo controle. Conclusão: O diabetes induzido em ratos altera a biodistribuição do radiofármaco Na99mTcO4, podendo esses achados ter implicações clínicas na interpretação de exames cintilográficos. Descritores: Biodisponibilidade. Pertecnetato. Diabetes. Estreptozotocina. Ratos. INTRODUCTION The radionuclides are employed in many fields of knowledge. In health sciences they contribute to the improvement of diagnosis and treatment, enabling advances in clinical and experimental research. Most diagnostic tests like scintigraphy, reveals the uptake of radioisotopes in several organs and tissues1-4. The most used radioisotopes are gamma radiation emitting, as a source of radiation or tracers1. Since the 60s, the 99mTechnetium (99mTc) is used in the biomedical area because it is easily obtained from molybdenum/technetium (99Mo/99mTc) generators, it has short half-life (6h), low emission energy, it is easy to label red blood cells, cellular structures or molecular, it has low cost and low environmental impact5-8. These features make 99mTc the most widely used radioisotope, administered in the form of sodium pertechnetate (Na99mTcO4) or attached to other molecules. Their biodistribution is evaluated by scintigraphy or other systems to detect radioativity6. 43 The scintigraphic image reflects morphology and organ function. Thus, different radioactive compounds can be used to study the physiology of organs and tissues. Therefore, a diseased tissue may contain higher or lower uptake of radioactivity, depending on its disfunction8. Scintigraphic examinations are used in the diagnosis of tumors, metastasis, gastric emptying, esophageal motility, thyroid nodules, bleeding, and in the monitoring of systemic diseases and their consequences, among them, diabetes9-15. The metabolic imbalance associated with diabetes causes secondary disorders in multiple organ systems, which can cause alterations in biodistribution of radioisotopes. Changes in scintigraphic examination results can generate false positive images, repetition of exams and increased patient exposure to radiation. Some studies advocate the use of streptozotocin to induce experimental diabetes, because it is a cytotoxic chemical agent, specific for pancreatic beta cells, causing severe primary insulin insuficiency and high glucose levels, followed by the establishment of diabetes in the subsequent 24 hours. This model, although with a high mortality rate is relatively easy, destroying the endocrine cells with preservation of exocrine function of pancreas16-18. Considering such principles, the objective of this study was to evaluate the biodistribution of sodium pertechnetate (Na99mTcO4) in different organs of rats with diabetes. METHODS We used 14 three months old Wistar rats, weighing 265g ± 31g, provided by the vivarium of the Health Sciences Center, Federal University of Rio Grande do Norte, Brazil. All animals were weighed, placed in individual cages with water and food (Purina ® Labina) ad libitum and acclimated in the laboratory for 7 days. They were kept under controlled temperature (21 degrees), humidity (60-70%), lighting (12/12 h) light / dark cycle and handled in accordance with the Ethical Code for Animal Experimentation (Council for International Organization of Medical Sciences) and the rules of the Brazilian College of Animal Experimentation. They were distributed randomly into two groups: diabetes (D, n = 7) and control group (C, n = 7). The animals in group D were subjected to induction of diabetes by injecting streptozotocin at the dose 80mg/kg, intraperitoneally (IP). Seven days after the injection of streptozotocin, glucose was measured by collecting blood from the dorsal vein of the 44 tail, using the equipment Accu-Chek Advantage, Roche Diagnostics, Mannheim, Germany (2003). We considered diabetic the animals with fasting glucose above 200 mg/dL. The C animals were not subjected to any procedure, only observed. On day 7, all animals were anesthetized with thiopental (20mg/kg-IP) and Ketamine (20mg/Kg-IM), administered 0, l ml Na99mTcO4 intravenously into the orbital plexus, and radioactivity dose was 0.68 MBq. After 30 minutes, the animals were killed with a lethal dose of anesthetic thiopental (100mg/kg), intracardiac, and samples were harvested from pancreas, brain, thyroid, lung, heart, stomach, liver, kidney, bladder and right femur. The samples were washed in 0.9% NaCl, weighed on a digital precision balance (Bel-Mark 160-II-Italy) and taken for detection of radioactivity through the 1470 Auto Gamma counter, WizardTM-Perkin-Elmer (Finland) with automatic correction of decay. The percentage of radioactivity per gram (% ATI/g) of each organ was calculated by dividing the activity per gram of tissue by the total radioactivity administered to each animal. The experiment was completely randomized with statistical analysis by Student t test. The level of significance for the test was 5% (95% CI), ie, p<0.05 was considered statistically significant. RESULTS Table 1 shows the results of %ATI/g in group D and C. In group D rats we observed a significant increase of the biodistribution of Na99mTcO4 in the liver and reduction in the uptake of thyroid, bladder and stomach when compared with group C rats. (p <0.05). The other organs did not show difference in %ATI/g, comparing with controls. Table 1 shows the results of %ATI/g in group D and C. In group D rats we observed a significant increase of the biodistribution of Na99mTcO4 in the liver and reduction in the uptake of thyroid, bladder and stomach when compared with group45 C rats. (p <0.05). The other organs did not show difference in %ATI/g, comparing with controls. Table 1. Biodistribution of Na99mTcO4 in organs and respective groups % ATI/g Organs Diabetes 0.02 ± 0.008 0.46 ± 0.154 0.41 ± 0.157 0.23 ± 0.067 0.43 ± 0.373 2.97 ± 1.745 0.27 ± 0.161 0.19 ± 0.055 0.15 ± 0.058 0.15 ± 0.047 Brain Thyroid Lung Heart Stomach Liver Kidney Bladder Femur Pancreas p-valor1 Control 0.01 ± 0.003 3.89 ± 1.447 0.39 ± 0.141 0.29 ± 0.061 3.33 ± 1.593 0.34 ± 0.050 0.42 ± 0.074 0.34 ± 0.094 0.14 ± 0.032 0.13 ± 0.046 0.093109 0.00075* 0.803036 0.223256 0.004118* 0.009782* 0.106062 0.015865* 0.709645 0.518932 Mean±SD. *Significant diference p<0.05. 1- p-valor of Student t test. DISCUSSION Research shows the interference of anesthetic drugs, chemotherapy and J Surg Cl on Res the ± Vol.biodistribution 1 (1) 2010:13-21 of sodium pertechnetate (Na99mTcO4). Recently, 15 herbals studies from our laboratory demonstrated changes in the uptake of radiopharmaceuticals in the postoperative of major surgeries involving experimental models of short bowel syndrome and bariatric surgery19-23. Diabetes mellitus and associated metabolic disturbances interfere with homeostasis, which may have caused changes in the biodistribution of pertechnetate on this study. We detected an increase in radioisotope uptake in the liver and a reduction in the stomach, bladder and thyroid gland of diabetic rats compared to controls. Bertin et al24 argued that the control of gastric emptying involves neurological, hormonal and metabolic factors and that the role of diabetes on gastric motility is little known. However El-Shaldy et al25 attributed the delay in gastric emptying to the inhibition of the hormone motilin by hiperglicemia. Theoretically, it was expected to obtain a higher uptake of gastric pertechnetate in rats of the experimental group, given the prior knowledge of several other trials on diabetic gastroparesis associated with autonomic neuropathy. However, we observed the opposite. This may affect the results of scintigraphy for the study of gastric emptying in diabetic patients commonly performed during the search of dispepticsymptoms14,26-31. 46 Another autonomic dysfunction in diabetes is the neurogenic bladder. Many researchers adopt as diagnostic of this pathology an increased tracer retention in the bladder during the performance of radionuclide cystography. The bladder dysfunction would result from neurological, muscular and urothelial injuries, uriginated on hiperglicemia32,33. We suppose that the low bladder uptake of sodium pertechnetate observed in this study was due to a marked polyuria in the experimental group rats, which may have contributed to greater intravesical radioactive energy dissipation. In relation to thyroid disorders associated with diabetes, it is a phenomenon widely reported in the current literature. It is estimated that diabetes is associated with hypothyroidism, Hashimoto's thyroiditis and nontoxic goiter in about 20-56% of cases involving mainly patients with type II diabetes34-36. It is therefore of great importance for thyroid evaluations. In this sense, thyroid scintigraphy is used in complementing clinical data and ultrasound. The use 99mTc displays advantages over iodine 131, because it labels the gland, allows its morpho-functional evaluation, with less patient exposure to radiation without interfering with the glandular function36. There was a lower thyroid uptake of sodium pertechnetate (Na99mTcO4) in our diabetic animals due to a probable subclinical hypothyroidism, as evidenced by Akbar et al, studying thyroid dysfunction in patients with type II diabetes37. Passos et al38 stated that a reduction in the synthesis of thyroglobulin precursor results in a lower uptake of sodium pertechnetate by the gland, since there is not enough protein to be marked. Thus, we alert to possible changes in thyroid scintigraphy in diabetic patients. A final analysis concerns the greater hepatic uptake of pertechnetate in the rats of the experimental group. Clinical trials point to the diabetes in the pathogenesis of liver diseases, with emphasis on non-alcoholic steatohepatitis, cirrhosis and hepatocellular carcinoma, including transplanted patient39-45. The liver participates directly in the glucose metabolism, raising or lowering the glucose uptake as vary their organic levels. It is postulated that a normalization of blood glucose, would result in regression of these pathological processes in inicial stage46. In this study, a likely steatohepatitis could have caused an increased uptake of sodium pertechnetate in the liver of diabetic rats, because once present in the circulation, the radiopharmaceuticals label not only erythrocytes but also leukocytes, showing a higher bioavailability in inflammed sites47,48. This phenomenon could alter the results 47 of liver scintigraphy when searching for primary tumors, liver cirrhosis and functional assessments in detecting metastases. CONCLUSION Diabetes altered the biodistribution of sodium pertechnetate (Na99mTcO4) in the liver, stomach, thyroid and urinary bladder of rats, emphasizing the need for a careful analysis of the results, if scintigraphic examinations are to be performed in patients with this disease. REFERENCES 1. Sampsom CB. Adverse reactions and drug interactions with radiopharmaceutical. Drug Safety. 1993;8:280-94. 2. Gutfilen B, Pellini MP, Roure-Neder J, Amarante Júnior JL, Evangelista MG, Fernandes SR, et al. 99mTc labeling white blood cells with a simple technique: clinical application. Ann Nucl Med. 1994;8:85-9. 3. Moreno SRF, Mattos MF, Rocha EK, Khan MM, San Gil Rãs, Conceição RC et al. Thalidomide: Labelling and suggestion of the chemical binding with techenetion-99m. Chem Nucl Med. 1999;65:641-6. 4. Gutfilen B, Ribeiro BLAR, Mattos MF, Ribeiro CR, Bernardo-Filho M. Labeling of thymidine technetion-99: suggestion of a chemical model. Braz Arch Biol T ecnol.1996;39:69-74. 5. Saha GB. Fundamentals of nuclear Pharmacy. 4ed. New York:Springer- Verlag; 1997. 6. Hladik WB, Saha GB. Study T. Essentials of Nuclear Medine Science. Baltimore: Williams; 1987: p3-50. 7. Braga AC, Oliveira MB, Feliciano GD, Reiniger IW, Oliveira JF, Silva CR et al. The effect of drugs on the labeling of blood elements with technetium-99m. Curr Pharm Des. 2000;6:1179-91. 8. Saha GB. Fundamentals of nuclear pharmacy. New York:Springer-Verlag; 2004. 9.Buchmann I, Riedmüller K, Hoffner S, Mack U, Aulmann S, Haberkorn U. Comparison of 99mtechnetium-pertechnetate and 123iodide SPECT with FDG-PET 48 in patients suspicious for breast cancer. Cancer Biother Radiopharm. 2007;22:77989. 10. Hansen AA, Rosenberg RJ. Gastrointestinal stromal tumor detected on Tc- 99m red blood cell scintigraphy. Clin Nucl Med. 2007;32:221-3. 11. Shie P, Cardarelli R, Brandon D, Erdman W, Abdulrahim N. Meta-analysis: comparison of F-18 Fluorodeoxyglucose-positron emission tomography and bone scintigraphy in the detection of bone metastases in patients with breast cancer. Clin Nucl Med. 2008;33:97-101. 12. Mariani G, Boni G, Barreca M, Bellini M, Fattori B, AlSharif A et al. Radionuclide gastroesophageal motor studies. J Nucl Med. 2004;45:1004-28. 13. Stathaki MI, Karkavitsas NS. Nuclear Medicine in the diagnosis of lower gastrointestinal bleeding. Hell J Nucl Med. 2007;10:197-204. 14. Faraj J, Melander O, Sundkvist G, Olsson R, Thorsson O, Ekberg O et al. O esophageal dysmotility, delayed gastric emptying and gastrointestinal symptoms in patients with diabetes mellitus. Diabet Med. 2007;24:1235-9. 15. Ohlsson B, Melander O, Thorsson O, Olsson R, Ekberg O, Sundkvist G. O esophageal dysmotility, delayed gastric emptying and autonomic neuropathy correlate to disturbed glucose homeostasis. Diabetologia. 2006;49:2010-4. 16. Delfino VDA, Figueiredo JF, Matsuo T, Fávero ME, Matni AM, Mocelin AJ. Diabetes mellitus induzido por estreptozotocina: comparação em longo prazo entre duas vias de administração. J Bras Nefrol. 2002;24:31-6. 17. Taniguchi H, Muroi R, Kobayashi-Hattori K, Uda Y, Oishi Y, Takita T. Differing effects of water-soluble and fat-soluble extracts from Japanese radish (Raphanus sativus) sprouts on carbohydrate and lipid metabolism in normal and streptozotocininduced diabetic rats. J Nutr Sci Vitaminol. 2007;53:261-6. 18. Ozkaia Y, Agar A, Hacioglu G, Yargiçglu P. Exercise improves visual deficits tested by visual evoked potentials in streptozotocin-induced diabetic rats. Tohoku J Exp Med. 2007;213:313-21. 19. Simões SB, Machado-Silva JR, Gutfilen B, Presgrave OA, Oliveira MB, Bernardo Filho M. Biodistribution study of the anaesthetic sodium phenobarbital labelled with technetium-99m in Swiss mice infected with Schistosoma mansoni Sambon, 1907. Mem Inst Oswaldo Cruz. 1997;92:677-81. 49 20. Santos JS, de-Paula EF, Correa TG, de-Freitas LC, da-Fonseca LM, Gutfilen B et al. Effect of cyclophosphamide on the binding of 99mTcO-4 and 99mTc-MDP to blood cells and plasma proteins. Braz J Med Biol Res. 1995;28:131-5. 21. Oliveira JF, Avila AS, Braga AC, de Oliveira MB, Boasquevisque EM, Jales RL et al. Effect of extract of medicinal plants on the labeling of blood elements with Technetium-99m and on the morphology of red blood cells: I--a study with Paullinia cupana. Fitoterapia. 2002;73:305-12. 22. Chacon DA, Araújo-Filho I, Villarim-Neto A, Rêgo AC, Azevedo IM, BernardoFilho M et al. Biodistribution of the radiophamarceutical sodium pertechnetate (Na99mTcO4) after massive small bowel resection in rats. Acta Cir Bras. 2007;22:430-5. 23. Araújo-Filho I, Rêgo ACM, Brandão-Neto J, Villarim-Neto A, Egito EST, Azevedo IM et al . Biodistribution of the radiopharmaceutical sodium pertechnetate after biliopancreatic bypass with a duodenal switch. Braz Arch Biol Technol. 2007;50:18997. 24. Bertin E, Schneider N, Abdelli N, Wampach H, Cadiot G, Lobo Guerrero A, et al. Gastric emptying is accelerated in obese type 2 diabetic patients without autonomic neuropathy. Diabetes Metab. 2001;27:357-64. 25. El-Salhy M, Spångéus A. Gastric emptying in animal models of human diabetes: correlation to blood glucoselevel and gut neuroendocrine peptide content. Ups J Med Sci. 2002;107:89-99. 26. Malmud LS, Fisher RS, Knight LC, Rock E. Scintigraphic evaluation of gastric emptying. Semin Nucl Med.1982;12:116-25. 27. Cesarini PR, Ferreira SRG, Dib SA. Gastroparesia diabética. Rev Assoc Med Bras. 1997;43:163-8. 28. Jones KL, Horowitz M, Wishart MJ, Maddox AF, Harding PE, Chatterton BE. Relationships between gastric emptying, intragastric meal distribution and blood glucose concentrations in diabetes mellitus. J Nucl Med. 1995;36:2220-8. 29. Nowak TV, Johnson CP, Kalbfleisch JH, Roza AM, Wood CM, Weisbruch JP et al. Highly variable gastric emptying in patients with insulin dependent diabetes mellitus. Gut. 1995;37:23-9. 30. Qi HB, Luo JY, Zhu YL, Wang XQ. Gastric myoelectrical activity and gastric emptying in diabetic patients with dyspeptic symptoms. World J Gastroenterol. 2002;8:180-2. 50 31. Yoshimura N, Chancellor MB, Andersson KE, Christ GJ. Recent advances in understanding the biology of diabetes-associated bladder complications and novel therapy. BJU Int. 2005;95:733-8. 32. Nagabhushan N, Syed R, Hoh IM, Syed I, Ell PJ, Shah PJ et al. 99mTechnetiummercaptoacetyltriglycine scintigraphy with full bladder in patients with severe bladder dysfunction. J Urol. 2006;176:1481-6. 33. Pimenta WP, Mazeto GMFS, Callegaro CF, Shibata SA, Marins LV, Yamashita S et al. Associação de tireopatias em uma população de pacientes com diabetes. Arq Bras Endocrinol Metab. 2005;49:234-40. 34. Umpierrez GE, Latif KA, Murphy MB, Lambeth HC, Stentz F, Bush Al. Thyroid dysfunction in patients with type 1 diabetes: a longitudinal study. Diabetes Care. 2003;26:1181-5. 35. Chubb SA, Davis WA, Davis TM. Interactions among thyroid function, insulin sensitivity, and serum lipid concentrations: the Fremantle diabetes study. J Clin Endocrinol Metab. 2005;90:5317-20. 36. Ramos CD, Zantut Wittmann DE, Etchebehere EC, Tambascia MA, Silva CA, Camargo EE. Thyroid uptake and scintigraphy using 99mTc pertechnetate: standardization in normal individuals. Sao Paulo Med J. 2002;120:45-8. 37. Akbar DH, Ahmed MM, Al-Mughales J. Thyroid dysfunction and thyroid autoimmunity in Saudi type 2 diabetics. Acta Diabetol. 2006;43:14-8. 38. Passos MC, Ramos CF, Bernardo-Filho M, de Mattos DM, Moura EG. The effect of protein or energy restriction on the biodistribution of Na99TcmO4 in Wistar rats. Nucl Med Commun. 2000;21:1059-62. 39. Hickman IJ, Macdonald GA. Impact of diabetes on the severity of liver disease. Am J Med. 2007;120:829-34. 40. Bell DS, Allbright E. The multifaceted associations of hepatobiliary disease and diabetes. Endocr Pract. 2007;13:300-12. 41. Komura T, Mizukoshi E, Kita Y, Sakurai M, Takata Y, Arai K. Impact of diabetes on recurrence of hepatocellular carcinoma after surgical treatment in patients with viral hepatitis. Am J Gastroenterol. 2007;102:1939-46. 42. Moscatiello S, Manini R, Marchesini G. Diabetes and liver disease: an ominous association. Nutr Metab Cardiovasc Dis. 2007;17:63-70. 51 43. Targher G, Bertolini L, Padovani R, Rodella S, Tessari R, Zenari L. Prevalence of nonalcoholic fatty liver disease and its association with cardiovascular disease among type 2 diabetic patients. Diabetes Care. 2007;30:1212-8. 44. Toledo FG, Sniderman AD, Kelley DE. Influence of hepatic steatosis (fatty liver) on severity and composition of dyslipidemia in type 2 diabetes. Diabetes Care. 2006;29:1845-50. 45. Iozzo P, Hallsten K, Oikonen V, Virtanen KA, Kemppainen J, Solin O. Insulinmediated hepatic glucose uptake is impaired in type 2 diabetes: evidence for a relationship with glycemic control. J Clin Endocrinol Metab. 2003;88:2055-60. 46. Papathanasiou ND, Rondogianni PE, Pianou NK, Karampina PA, Vlontzou EA, Datseris IE. 99mTc-depreotide in the evaluation of bone infection and inflammation. Nucl Med Commun. 2008;29:239-46. 47. Joseph B, Bhargava KK, Tronco GG, Palestro CJ, Gupta S. Systemic and local release of inflammatory cytokines regulates hepatobiliary excretion of 99mTcmebrofenin. Nucl Med Commun. 2008;29:336-44. 48. Carmo VA, Ferrari CS, Reis EC, Ramaldes GA, Pereira MA, De Oliveira MC. Biodistribution study and identification of inflammation sites using 99mTc-labelled stealth pH-sensitive liposomes. Nucl Med Commun. 2008;29:33-8. 52 5.4. O Artigo foi publicado no periódico Journal of Surgical and Clinical Research. 2010:1(1):46-53. (ISSN 2179-7889) Splenectomy changes the biodistribution of pertechnetate (99mTcO4-) in rats A esplenectomia altera a biodistribuição do pertecnetato (Tc99mo4-) em ratos Ítalo Medeiros Azevedo, Ana Paula Fernandes Neves, Danilo Veras Lobo de Paiva, Jurema Samara Fonsêca Véras, Larissa de Castro Tomasi, Amália Cínthia Meneses Rêgo, PhD, Marília Daniela Ferreira Carvalho, Vítor Brasil Medeiros, Irami Araújo- Filho, MD, PhD, Aldo Cunha Medeiros, MD, PhD. From the Department of Surgery and Postgraduate Program in Health Sciences, Federal University of Rio Grande do Norte, Brazil Financial support: CNPq, Brazil. Conflict of interest: None. Correspondence address: Ítalo Medeiros Azevedo, Department of Surgery, Federal University of Rio Grande do Norte, at Ave Nilo Peçanha 620, Natal, RN, Brazil. Email: [email protected] Submitted: 06 December 2010. Accepted, after review: 27 December 2010. ABSTRACT Purpose: To assess if splenectomy alters the biodistribution of sodium pertechnetate in organs and tissues of rats. Methods: Twelve Wistar rats were randomly allocated into two groups, A (splenectomized) and B (control), anesthetized with ketamine (50 mg / kg, IM, and sodium thiopental (20 mg / kg-IP) and operated under aseptic conditions. Group A (n = 6) rats underwent laparotomy for splenectomy and group B rats (n = 6) were only anesthetized. Both remained under postoperative observation and after 10 days they were injected with 0.1 mL of sodium pertechnetate (0.66MBq) via orbital plexus. After 30 min, the rats were killed by an overdose of anesthetic and samples of stomach, liver, heart, lung, thyroid, bladder, kidney, brain and femur were harvested. Detection of radioactivity was determined by an automated gamma counter, Wizard Gamma Counter Perkin-Elmer. Data were expressed as mean±standard deviation and Student t test was used for independent samples, considering p<0.05 as significant. Results: There was a lower uptake of pertechnetate in group A than group B in kidney, heart, lung, bladder and femur 53 (p<0.05), when compared with controls. The liver of the splenectomized animals showed radioactive uptake significantly higher than in controls. Conclusion: According to the experimental model, we conclude that totalsplenectomy in rats resulted in alteration in the biodistribution of pertechnetate in vital organs. Key words: Bioavailability. Tc 99m Pertechnetate. Splenectomy. Rats. RESUMO Objetivo: Avaliar se a esplenectomia altera a biodistribuição do radiofármaco pertecnetato de sódio nos órgãos e tecidos de ratos. Métodos: Doze ratos Wistar foram distribuídos aleatoriamente em 2 grupos, A (esplenectomizados) e B (controle), anestesiados com ketamina (50 mg/Kg-IM, e tiopental sódico (20 mg/KgIP), operados sob condições assépticas. Os animais do grupo A (n=6) foram submetidos a laparotomia mediana e esplenectomia total e grupo B (n=6) apenas foram anestesiados. Ambos permaneceram sob observação pós- operatória e após 10 dias foram submetidos à administração de 0,1 ml de pertecnetato de sódio (0,66MBq) via plexo orbital. Após 30 min, foram mortos com superdose de anestésico e submetidos à retirada de segmentos do estômago, fígado, coração, pulmão, tireóide, bexiga, rim, fêmur e cérebro. A detecção da radioatividade foi determinada através de contador gama automático, Wizard Gama Counter PerkinElmer®. Dados foram expressos em média±desvio padrão e o teste t de Student para amostras independentes foi usado, considerando as diferenças significantes com p<0,05. Resultados: Observou-se menor captação do pertecnetato nos animais do grupo A em relação ao grupo B, no rim, coração, pulmão, bexiga e fêmur com p<0,05. O fígado dos animais esplenectomizados apresentou captação radioativa significativamente maior do que nos controles. Conclusão: De acordo com o modelo experimental utilizado, pode-se concluir que a esplenectomia total em ratos resultou em alteração na biodistribuição do pertecnetato de sódio em órgãos vitais. Descritores: Biodisponibilidade. Pertecnetato. Esplenectomia. Ratos. INTRODUCTION 54 The use of radionuclides has contributed to important advances in health sciences. Diagnostic evaluations are possible by using radiopharmaceuticals labeled with 99m technetium (99mTc)1-6. The widespread use of 99mTc is due to a number of chemical, physical, economic and ambiental characteristics7. 99mTc is an artificial radionuclide originating from the disintegration of 99molibdenium, an isotope from the nuclear fission of uranium. Its main features are: half-life of six hours, emission of gamma (g) rays and radiation energy of 140 Kev. By its high availability, easy for connecting to the red blood cells, biological species, cellular structures, molecular, low cost and negligible environmental impact, it has become the most used radionuclide in nuclear medicine under sodium pertechnetate (Na99mTc04)8. It is known that some drugs can interfere with the biodistribution of radiofarmaceuticals912 . However, little is known about the impact of organ resection on the biodistribution of Na99mTc04 and publications are unavailable in the literature regarding the effects of splenectomy on biodistribution13. If splenectomy interferes with the biodistribution of radiopharmaceuticals, scintigraphic exams may result in images of dubious accuracy, culminating in repeated examinations and unnecessary exposure of patients to radiation. In recent decades, traditional indications for splenectomy have been discarded due to high incidence of deaths due to postoperative sepsis14. The emergence of alternative management replaced splenectomy. However, serious cases such as pancytopenia, hematological diseases with high risk of systemic or intracranial bleeding, hypersplenism, gastric carcinoma, portal hypertension and trauma are still indications for esplenectomy14. The aim of this study was to evaluate if the excision of the spleen alters the biodistribution of Na99mTc04 in organs and tissues of operated rats. METHODS In this experimental study we used 12 Wistar rats weighing 295±23g. The rats were from Vivarium of Center of Health Sciences, Federal University of Rio Grande do Norte, Brazil. They were randomly allocated into 2 groups: A (Esplenectomized) and B (Control), of 6 rats each. The investigational protocol was approved by the Institutional Animal Care Committee, and the research was performed in accordance with the guidelines of the Brazilian College of Animal Experimentation. 55 The rats were observed in individual cages with food and water ad libitum; They were anesthetized with ketamine (50 mg/Kg) i.m. and sodium thiopental (20 mg/Kg) i.p, operated under aseptic conditions. Splenectomy group animals underwent midline laparotomy and subsequent splenectomy. The laparotomy was closed in layers with mononylon 4-0 suture. Hydration was done with normal saline (10 mL/100g weight) injected subcutaneously in the rats for the first 2 postoperative days. Postoperative pain was treated with tenoxicam (Roche Pharm., Brazil); 0.5 mg/kg was injected i.m. once a day for 3 days. In the control group the rats were only anesthetized. Both groups remained under observation for 10 postoperative days, during which the rats were weighed dayly. The animals were again anesthetized with the above-mentioned anesthetic association and injected with 0.1 ml of Na99mTc04 via the orbital plexus, producing a radioactivity of 0.66 MBq. After 30 minutes, the rats were killed by an overdose of anesthetic (thiopental 100mg/Kg) and samples of stomach, liver, heart, lung, thyroid, bladder, right kidney, right femur and brain were harvested. The samples were washed with 0.9% saline solution, and weighed on a precision scale. The detection of radioactivity in each sample was determined using an automatic gamma counter, Wizard Gamma Counter® Perkin-Elmer, Finland. The percentage of radioactivity of each organ (%ATI/g) was calculated by dividing the radioactivity of each organ by the total activity administered to each animal. Data were expressed as mean±SD. The comparison between groups was performed by Student t test for independent samples, using a 0.05 significance. RESULTS After analysis of the percentages of radioactive uptake (%ATI/g) from the organs samples, comparing the control and splenectomized groups, it was observed that there was lower uptake of pertechnetate in group A rats than group B in the kidney, heart, lung, bladder and femur. These differences were statistically significant (p<0.05). The liver of the splenectomized animals showed significantly higher radioactive uptake than in controls (p=0.0239). The other organs showed no significant change in the uptake of compared splenectomy and control groups (Table 1). 56 Table 1 - Values of % radioactivity per gram of tissue (%ATI/g) from rats organs. Mean±SD * p≤0.05, comparing splenectomy group and control. 1. P-valor after analysis by t test for independent samples. DISCUSSION 99m Technetium (99mTc) is of great diagnostic utility. The labeling of tissues is based on the reduction capacity of stannous chloride (SnCl2), which acts on the 99m Tc in the form of Na99mTc04. Several factors influence the biodistribution of different radiopharmaceuticals, among them are surgical procedures13,32-34. Changing in biodistribution can lead to repeat examinations for patients undergoing surgery, resulting in unnecessary irradiation. The human spleen is located in the left hypochondrium and has the dimensions 12 cm long by 8 cm wide and 3 cm thick. His weight without blood varies from 75 to 90g; in vivo, the spleen weight varies between 150 and 250g15. Despite its size, it is irrigated with 350 liters of blood per day, at a speed of 200 ml/min, accounting for 40% of portal vein flow16. Through its great amount of macrophages, spleen has one quarter of the lymphoid tissue of the body, and is able to remove foreign particles from the blood and abnormal cells17. This function is very important because these macrophages can phagocyte even without the presence of opsonins. This peculiarity gives great power to the spleen as a defense organ in cases of acute infection. However, this paper only begins to develop over the years, since in childhood the spleen is an organ histologically and 57 physiologically imature18. Splenectomy is indicated in several situations, among them, traumatic causes14. It is also held in non-traumatic cases, such as the surgical treatment of gastric carcinoma, portal hypertension, idiopathic thrombocytopenic purpura and splenic cysts19-21. As there are no published reports of research involving the study of the biodistribution of Na99mTc04 after splenectomy, this study has sought to fill this gap and contribute to clarify this issue. The distribution, fixation and disposal of radiopharmaceuticals in the organs and tissues depend on the flow circulation, metabolism and binding to tissue and blood elements22. However, it is known that red blood cells are remodeled in the spleen, passing from spherical to biconcave discs; it clears substances deposited on their surface, such as proteins, Howell- Jolly bodies (nuclear remnants), Heinz bodies (denatured hemoglobin) and Pappenheimer corpuscles (siderotic granules). The spleen is also active on the destruction of aging red blood cell, poorly formed or coated with antibodies14. Therefore, the spleen is of fundamental importance in the formation of functional red blood cells and destruction of aged red blood cells. Splenectomy can interfere with labeling with radiopharmaceuticals, thereby altering the biodistribution of Na99mTc04. Some studies have related splenectomy as a source of repercussions on the monocytic fagocitosis23 lipidic profile24 limph nodes25, showing that the asplenic state carries systemic consequences. In our study there was a change in the Na99mTc04 biodistribution in various organs. There was lower uptake in kidney, heart, lung, bladder, femur and brain of splenectomized animals than in controls. This finding confirms the hypothesis that removal of the spleen significantly alters the biodistribution of Na99mTc04 in rats, which may be related to the effects of asplenia in the formation of red blood cells or other systems. It has been reported that spleen interferes with hepatic function26. In fact, in our study certainly the most relevant finding was the observation that the radioactive uptake in the liver was found to be higher than in controls, indicating that the absence of the spleen increased the uptake of Na99mTc04 in liver. If this is true, we can infer that there are clinical implications after splenectomy, i.e., the liver can undergo changes in their physiology, affecting the uptake of radiopharmaceuticals for diagnostic or therapeutic use. Splenectomy might somewhat promote hepatic regeneration26,27, prevent liver fibrosis to a certain degree28, reduce serum bilirubin concentration and improve liver 58 function29,30. In a clinical study, serum total bilirubin concentration was promptly decreased to normal range or pre-operative level on the 7th day in splenectomy group, though it was raised for a transient time. Serum total bilirubin concentration increased on 10 to 14 days in non-splenetomy group. The total bilirubin concentration was significantly lower in the former than in the latter on the 7th day after operation, obviously reflecting the effect of splenectomy on reducing the burden of hepatocyte bilirubin31. CONCLUSION According to the experimental model used in this study, we can conclude that total splenectomy in rats resulted in alteration in the biodistribution of Na99mTc04 in vital organs. REFERENCES 1. Tiktinsky E, Horne T, Agranovich S, Landsberg S. Unilateral Tc-99m pertechnetate breast uptake: is it always benign? Clin Nucl Med. 2007;32:735-6. 2. Zhang L, Zhu ZH, Dai HJ, Cai ZG, Mao C, Peng X et al. Application of 99mTcpertechnetate scintigraphy to microvascular autologous transplantation of the submandibular gland in patients with severe keratoconjunctivitis sicca. J Nucl Med. 2007;48:1431-5. 3. Tuncel M, Ozgen Kiratli P. Vascular retention of Tc-99m pertechnetate and Tc99m sestamibi, mimicking thyroid carcinoma metastases. Rev Esp Med Nucl. 2007;26:226-9. 4. Sadeghi R, Kakhki VR, Zakavi R. Dramatic movement of a Meckel's diverticulum on Tc-99m pertechnetate imaging. Clin Nucl Med. 2007;32:460-1. 5. Zanglis A, Andreopoulos D, Baziotis N. Trapping of technetium-99m albumin macroaggregate and other four radiopharmaceuticals by blood clots in vitro. Hell J Nucl Med. 2007;10:24-5. 6. Kim H, Chaudhuri TR, Buchsbaum DJ, Wang D, Zinn KR. High-resolution singlephoton emission computed tomography and X-ray computed tomography imaging of Tc-99m-labeled anti-DR5 antibody in breast tumor xenografts. Mol Cancer Ther. 2007;6:866-75. 59 7. Early PJ, Sodee DB. Principles and practice of nuclear medicine. 2 ed. Saint Louis: Mosby Year Book; 1995. 8. Saha GB. Fundamentals of nuclear pharmacy. 5th ed. New York: Springer- Verlag; 2004. 9. Gomes ML, de Mattos DM, Freitas RS, Diré GF, Lima EA, Souza SM et al. Evaluation of the effect of mitomycin-C on the bioavailability of technetium-99mlabelled sodium pyrophosphate in mice. Cell Mol Biol. 2002;48:757-9. 10. Braga AC, Oliveira MB, Feliciano GD, Reiniger IW, Oliveira JF, Silva CR et al. The effect of drugs on the labeling of blood elements with technetium-99m. Curr Pharm Des. 2000;6:1179-91. 11. Oliveira JF, Avila AS, Braga AC, de Oliveira MB, Boasquevisque EM, Jales RL et al. Effect of extract of medicinal plants on the labeling of blood elements with Technetium-99m and on the morphology of red blood cells: A study with Paullinia cupana. Fitoterapia. 2002;73:305-12. 12. Feliciano GD, Lima EA, Pereira MJ, de Oliveira MB, Moreno SR, de Mattos DM et al. Effect of a chayotte (Sechium edule) extract on the labeling of red blood cells and plasma proteins with technetium-99m: in vitro and in vivo studies. Cell Mol Biol. 2002;48:751-5. 13. Chacon DA, Araújo-Filho I, Villarim-Neto A, Rego ACM, Azevedo IM, BernardoFilho M, Medeiros AC. Biodistribution of sodium pertechnetate (Na99mTcO4) after massive small bowel resection in rats. Acta Cir Bras. 2007;22:430-5 14. Petroianu A. Esplenectomia. In: Petroianu A. Terapêutica Cirúrgica. 1a ed. Rio de Janeiro:Guanabara Koogan; 2001. p.596-9. 15. Jakobsen SS, Jakobsen US. The weith of normal spleen. Forensic Sci Int. 1997;88:215-23. 16. Coetzee T. Clinical anatomy and psysiology of the spleen. South Afr Med. 1982;61:737-46. 17. Petroianu A, Barbosa AJA. Quantitative study on the macrophage phagocytosis in whole spleen and in remnant of subtotal splenectomy. Med Sci Res. 1991;19:3735. 18. Llende M, Deplin AS, Lavergne J. Immunobiological consequences of splenectomy. J Surg Res. 1986;40:85-94. 19. Ferzli G, Fiorillo M, Kiel T. Early experience with laparoscopic splenectomy. J Laparoendosc Surg. 1996;6:83-6. 60 20. Nogueira MVF, Winkler A, Hidd BE et al. Esplenectomia leparoscópica. Rev Col Bras Cir. 1994;21:278-81. 21. Sard A. Laparoscopic splenectomy for patients with idiopathic thrombocytopenic purpura. Surg Laparosc Endosc. 1994;4:316-9. 22. Sampson CB. Complications and difficulties in radiolabelling blood cells: a review. Nucl Med Commun. 1996;17:648-58. 23. Petroianu A. Evaluation of possible failure of the mononuclear phagocyte system after total splenectomy in rats. Braz Arch Biol Technol. 2004;47:199-204. 24. Petroianu A et al. Effects of splenic surgeries on lipidogram of rats. Rev Assoc Med Bras. 2006;52:56-9. 25. Slusarczyk K et al. Effect of splenectomy on the morphology of haemolymph splenic nodes in Wistar rats. Med Sci Monit. 2000;6:675-9. 26. Murata K, Shiraki K, Sugimoto K, Takase K, Nakano T, Furusaka A et al. Splenectomy enhances liver regeneration through tumor necrosis factor (TNF)- alpha following dimethylnitrosamine-induced cirrhotic rat model. Hepatogastroenterology. 2001;48:1022-7. 27. Akahoshi T, Hashizume M, Tanoue K, Shimabukuro R, Gotoh N, Tomikawa M et al. Role of the spleen in liver fibrosis in rats may be mediated by transforming growth factor beta-1. J Gastroenterol Hepatol. 2002;17:59-65. 28. Chen D, Liu W, Leng E, Wu B. Effect of splenectomy on CCl4-induced liver fibrosis in rats. Chin Med J. 1998;111:779-83. 29. Shimada M, Hashizume M, Shirabe K, Takenaka K, Sugimachi K. A new surgical strategy for cirrhotic patients with hepatocellular carcinoma and hypersplenism. Performing a hepatectomy after a laparoscopic splenectomy. Surg Endosc. 2000;14:127-30. 30. Lin MC, Wu CC, Ho WL, Yeh DC, Liu TJ, Peng FK. Concomitant splenectomy for hypersplenic thrombocytopenia in hepatic resection for hepatocellular carcinoma. Hepatogastroenterology. 1999;46:630-4. 31. Cao ZX, Chen XP, Wu ZD. Effects of splenectomy in patients with cirrhosis undergoing hepatic resection for hepatocellular carcinoma. World J Gastroenterol. 2003;9:2460-3. 32. Rêgo AC, Ramalho RA, Egito ES, Araújo-Filho I, Azevedo IM, Palestro CJ, Medeiros AC. Biodistribution of technetium-99m pertechnetate after total colectomy in rats. Appl Radiat Isot. 2010;68:2169-73. 61 33. Rêgo AC, Villarim Neto A, Azevedo IM, Araújo-Filho I, Egito ES, Medeiros AC. Biodistribution of Technetium-99m pertechnetate after total gastrectomy and Rouxen-Y jejunal pouch. J Invest Surg. 2010;23:94-100. 34. Rêgo AC, Araújo-Filho I, Azevedo IM, Jácome DT, Ramalho Rde A, Medeiros AC. Biodistribution of technetium-99m pertechnetate after Roux-en-Y gastric bypass (Capella technique) in rats. Acta Cir Bras. 2010;25:9-12. 62 5.5. O Artigo foi publicado no periódico Journal of Surgical and Clinical Research. 2010;1:54-65. (ISSN 2179-7889). Bacterial translocation in rats treated with simvastatin undergoing intestinal ischemia and reperfusion. Translocação bacteriana em Ratos tratados com sinvastatina submetidos a isquemia intestinal e reperfusão. Ítalo Medeiros Azevedo, Irami Araújo Filho, MD, PhD, Amália Cinthia Meneses Rêgo, PhD, Vítor Brasil Medeiros, Marília Daniela Ferreira Carvalho, MD, Eryvaldo Sócrates Tabosa Egito, PhD, Aldo Cunha Medeiros, MD, PhD. Research performed at Nucleus for Experimental Surgery and Postgraduate Program in Health Sciences, Federal University of Rio Grande do Norte (UFRN), Brazil. Financial support: CNPq, Brazil. Conflict of interest: None. Correspondence address: Ítalo Medeiros Azevedo, Department of Surgery, Federal University of Rio Grande do Norte, at Ave. Nilo Peçanha 620, Natal, RN, Brazil, Email: [email protected] Submitted: 10 December 2010. Accepted, after review: 27 December 2010. ABSTRACT Purpose: To evaluate the anti-inflammatory effect of simvastatin in an experimental model of intestinal ischemia/reperfusion, as well as in the prevention of bacterial translocation. Methods: We used Wistar rats, randomly allocated in 5 groups: C (n=10) controls; S (N=10) Shan-operated; I/R (n=10) intestinal ischemia and reperfusion; S+Sim (n=7) sham treated with simvastatin and I/R+Sim (n=7) ischemia/reperfusion treated with simvastatin. In the group S, a laparotomy and manipulation of intestinal loops were performed. In the groups I/R and I/R+Sim, the superior mesenteric artery was occluded with a vascular microclamp, the laparotomy was closed and reopened 60 minutes after for pull back the clamp. The reperfusion was confirmed by the return of the pulsation of the mesenteric arcade. The animals were sacrificed after 120 minutes of reperfusion. Simvastatin microemulsion (10mg/kg) was administered (gavage) 18 hs and 2 hours before the surgical procedure. Blood was collected by cardiac puncture for measurement of TNF-α, IL- 63 1β, IL-6 and IL-10. One gram of spleen, liver and mesenteric lymph nodes was harvested for culture in selective means for Gram (-) and Gram (+) bacteria. A sample of terminal ileum of each animal was harvested, fixed in formalin 10% and included in paraffin. Slices were stained with hematoxilin-eosin for morphometric measurement. The damages of the intestinal samples were examined in a blind way by an experienced pathologist, in agreement with microscopic criteria for levels of aggressions based previously on a grade system. ANOVA and the post-hoc Tukey test were used, considering p<0,05 as significant. Results: We observed bacterial translocation to mesenteric lymph nodes, spleen, liver and blood in all animals submitted to I/R, being smaller in the group I/R treated with simvastatin than in controls. In the I/R group rats the values of pro-inflammatory cytokines were significantly higher, when compared to the I/R+Sim group rats. The I/R+Sim group rats showed higher levels of IL-10, when compared with the other groups (p<0.05). The ileal segments presented macroscopic dilation and intramural hemorrhage. The microscopy revealed intense mucosa lesion in the group I/R compared to the other groups. The histopathologic findings of the I/R+Sim group rats were similar to that found in the groups C and S. Conclusion: The simvastatin contributed to reduce the bacterial translocation, the values of pro-inflammatory cytokine and to increase the levels of anti-inflammatory cytokine, preserving the integrity of the intestinal epithelium in an experimental model of ischemia/reperfusion. Key words: Simvastatin. Ischemia/Reperfusion. Bacterial Translocation. Sepsis. Rat. RESUMO Objetivo: Avaliar o efeito anti-inflamatório da sinvastatina em modelo experimental de isquemia/reperfusão intestinal, assim como na prevenção da translocação bacteriana. Métodos: Ratos Wistar foram distribuídos aleatoriamente em 5 grupos: C (n=10) controle; S (n=10) simulação (sham); I/R (n=10) isquemia intestinal e reperfusão; S+Sin (n=7) sham tratado com sinvastatina e I/R+Sin (n=7) isquemia/reperfusão tratado com sinvastatina. No grupo S, procedeu-se laparotomia e manipulação atraumática de alças intestinais. Nos grupos I/R e I/R+Sin, a artéria mesentérica superior foi ocluída com microclamp vascular por 60 minutos. A laparotomia foi fechada e reaberta após 60 minutos para retirada do clamp e a reperfusão foi confirmada pelo retorno da pulsação da arcada mesentérica. Os 64 animais foram sacrificados após 120 minutos de reperfusão. Microemulsão de sinvastatina (10mg/kg) foi administrada por gavagem 18 horas e 2 horas antes do procedimento cirúrgico. Sangue total foi coletado por punção cardíaca, para dosagem de TNFa, IL-1b, IL-6 e IL-10. Um grama de baço, fígado e linfonodos mesentéricos foram removidos para cultura bacteriana em meios seletivos para Gram (-) e Gram (+). Segmento de íleo terminal de cada animal foi fixado em formalina a 10% e embebido em parafina. Secções coradas com hematoxilinaeosina para usadas para medidas morfométricas. Os danos intestinais foram avaliados de acordo com critérios microscópicos para níveis de lesões baseados em um sistema de graduação previamente descrito. Foram utilizados os testes ANOVA e Tukey, considerando p<0,05 estatisticamente significante. Resultados: Observouse translocação bacteriana para linfonodos mesentéricos, baço, fígado e sangue em todos os animais submetidos a I/R, sendo menor no grupo I/R+ Sin, tratado com sinvastatina. No grupo I/R, os valores de citocinas pró-inflamatórias foram significativamente maiores, quando comparados ao grupo I/R+Sin. Os animais do grupo I/R+Sin apresentaram os maiores níveis de IL-10, em relação aos demais grupos (p<0,05). Os segmentos de íleo apresentaram dilatação e hemorragia intramural macroscópicas. A microscopia revelou lesão intensa de mucosa nos ratos do grupo I/R comparado aos demais grupos. Os achados histopatológicos do grupo I/R+Sin foram semelhantes aos encontrados nos grupos C e S. Conclusão: A sinvastatina contribuiu para a redução da translocação bacteriana, dos valores de citocinas pró-inflamatórias e elevou os níveis de citocina anti-inflamatória, preservando a integridade do epitélio intestinal em modelo experimental de isquemia e reperfusão. Descritores: Sinvastatina; Isquemia/Reperfusão; Translocação Bacteriana; Sepse; Rato. INTRODUCTION Intestinal ischemia-reperfusion (I-R) injury is a severe condition resulting from acute mesenteric ischemia, small bowel transplantation, abdominal aortic aneurysm, hemorrhage, trauma, septic shock, or severe burns1,2. Various chemical and cellular mediators have been implicated in the pathogenesis of intestinal 65 ischemia/reperfusion, such as reactive oxygen, cytokines, endotoxins, and neutrophils. Following adhesive interactions among neutrophils and endothelial cells, neutrophil accumulation in the intestinal mucosa contributes to intestinal ischemia/reperfusion injury via production of reactive oxygen metabolites and proteases3. Leukocyte accumulation is a complex phenomenon that also involves endothelium-based adhesion molecules as well as leukocyte chemotaxis factors such as interleukin-8 (IL-8). Intercellular adhesion molecules are normally expressed at a low basal level, but their expression can be enhanced by several inflammatory cytokines such as IL-1β and tumor necrosis factor-α (TNF-α). A variety of cytokines, including TNF-α, interferon-γ and IL-1β, are released from post-ischemic tissues4. On 1976, in independent publications, Endo et al. e Brown et al, described the first statin able to inhibit the HMG-CoA redutase. These drugs attracted the attention of researchers because of their capacity to reduce serum cholesterol. Then, many other statins were isolated5-7. Increasing number of evidence suggests that 3hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase inhibitors, or statins, exert pleiotropic effects which are independent from their cholesterol-lowering action8. One of these effects appears to be protection against ischemia/reperfusion injury. Several studies dealing with ischemia/reperfusion have shown that statins significantly reduce infarct size not only in heart but also in brain9,10. Statins have been shown to elevate the expression of endothelial nitric oxide synthase (eNOS); hence enhancing the basal and stimulated production of NO and improving endothelium dependent vasorelaxation besides promoting antiinflammatory processes11. They are involved in diverse cellular functions, including actin cytoskeleton organization, cell adhesion and motility, gene expression, and inflammation. Thus, inhibition of Rho kinases may contribute to some of the cholesterol-independent beneficial effects of statin therapy. It has been postulated that their antiinflammatory effects may be associated with modulation of both adhesion molecule and cytokine production12,13. Maintenance of bacteria and their products in the intestinal lumen are made by mucin and epithelial cells, essential for survival. The enterocytes in constant division, form an impermeable barrier to the intestinal contents. Because they are metabolically active, they are susceptible to hypoxia, reducing the absorptive function with loss of basement membrane integrity, leading to the bacterial translocation 14,15. Berg and Garlington (1979) described the translocation as the passage of viable 66 bacteria through the intestinal mucosa to mesenteric lymph nodes, tissues and órgãos16. It is postulated that ischemia and reperfusion promote translocation, bacteremia and toxemia, initiating an inflammatory response and activating inflammatory mediators, including cytokines17. In sepsis, the mortality ratio is directly proportional to the intensity of the inflammatory response18-20. Based on these principles, the objective of this study was to evaluate the anti- inflammatory effect of simvastatin in an experimental ischemia/reperfusion model, as well as bacterial translocation. METHODS Animals Fifty male Wistar rats weighing 265±32g (from Nucleus of Experimental Surgery, Federal University of Rio Grande do Norte-UFRN, Brazil) were used. Rats were housed in polypropilene cages and maintained under controlled temperature conditions on a 12h light-dark cycle and allowed ad libitum access to commercially available rat chow and water. The experimental protocol was approved by the Research Ethics Committee of the Federal University of Rio Grande do Norte, Brazil, and adhered to the Guide for the Care and Use of Laboratory Animals, US National Research Council, 1996. Experimental design The rats were randomly assigned to 5 groups (n=7 in each group) as described below. The control group (C) received only chow and water; Group sham (S) served as a normal control, and a laparotomy was performed and the rats received only chow and water. The ischemia/reperfusion rats (I/R) were submitted to mesenteric ischemia/reperfusion; the sham/simvastatin (S+Sim) and the Ischemia/reperfusion (I/R+Sim) group rats were treated with simvastatin. Treatment with simvastatin or normal saline (0.9%) was done according to the protocol. Simvastatin rats received 20 mg/Kg of simvastatin microemulsion via gavage for 5 days before surgery. Animals were fasted 12 hr before the experiment and anesthetized with an intramuscular injection of 50mg of ketamine/Kg of body weight and thiopental 20mg/Kg IP. In groups I/R and I/R+Sim, under sterile conditions, a laparotomy was performed and the superior mesenteric artery (SMA) was occluded with a 67 microvascular clamp for 60 minutes. In order to block any collateral blood supply, the right colic and proximal jejunal arteries were also clamped. The laparotomy incision was then closed, to be opened later for removal of the clamps after 60 minutes of ischemia. Reperfusion was confirmed by the return of the mesenteric arcade pulsation. The incision was closed again and the animals were killed by anesthetic overdose (thiopental 100mg/Kg) after 120 minutes of reperfusion. The shamoperated rats received the same surgical procedure as the other groups without being subjected to the ischemia- reperfusion protocol. Measurement of bacterial translocation At the end of the procedures (time = 180 minutes), a midline laparotomy was performed under aseptic conditions and biopsies were aseptically obtained for bacterial colony counts. One gram of MLN complex, liver and lung was removed for culture. Tissues were homogenized and aseptically solubilized after addition of 0.5 mL of 0.9% saline. Aliquots of 0.2mL were processed and cultured on selective MacConkey's agar and blood agar for detection of gram- negative and gram-positive bacteria, respectively. The agar plates were incubated at 37 oC and examined for growth after 24 and 48 hours. Any growth in the plates of bacteria of the same biotype as cultured was considered positive and expressed as colony-forming units per gram of tissue (CFU/g). Histological study Ileum specimens were fixed in 10% buffered formalin and embedded in paraffin. Sections cut at a thickness of 4mm were stained with hematoxylin and eosin for morphometric measurements using an image analyzer (Image-Pro Plus, Media Cyber®). The damage of the intestinal specimens was assessed in a blinded manner by an experienced pathologist according to microscopic criteria for degree of damage based on a grading system previously described [17]: normal mucosa, 0; subepithelial space at the viluus tip, 1; more extended subepithelial space, 2; epithelial lifting along villus, 3; denuded villi, 4; loss of villus tissue, 5; crypt layer infarction, 6; transmucosal infarction, 7; transmural infarction, 8. Cytokine assays Portal blood samples were collected and used for measurement of tumor 68 necrosis factor-alfa (TNFa), interleukin-1b (IL-1b), interleukin-6 (IL-6) and interleukin10 (IL-10), determined using enzyme-linked immunoassay kits (all from PeproTech, Rocky Hill, NJ, USA), according to the manufacturer’s recommended protocols. The fluorescence was measured by a Bio-Tec Instruments EL 808 ultra microplate reader, using KC4-V3.0 analysis software. Sensitivity of detection was 30 pg/ml for cytokines. Statistics Data analysis was performed using the BioEstat 2.0 program. Differences between the microbiological samples as measured by positive cultures were evaluated by a test for differences between proportions. The results were tabulated and compared by ANOVA using post hoc analysis with Tukey test. P<0.05 was considered significant. RESULTS We observed bacterial translocation to mesenteric lymph nodes, spleen, liver and blood in all animals subjected to I / R. However, in I/R group rats treated with simvastatin, translocation to these organs was significantly lower than in I/R untreated (Table 1). In the control group, there was no bacterial translocation as well as in the sham group rats, except in the mesenteric lymph nodes. In group S+Sin, paradoxically, there was bacteremia at the expense of Gram-positive (Staphylococcus aureus). Table 1- Bacterial Translocation in groups treated and not treated with simvastatin (colony-forming units per gram of tissue - CFU/g). *p < 0.01 compared with groups C, S, IR/Sim. Cytokines were not detected in group C rats. In group S+Sin, we observed 69 lower levels of proinflammatory cytokines (TNF-a, IL-1 b, IL-6) and a higher level of antiinflammatory-cytokine (IL-10), when compared with group S (Table 2). In I/R group rats, the levels of pro-inflammatory cytokines were significantly higher when compared to I/R+Sim. This group had the highest values of IL-10 when compared with all other groups (p<0.05). Table 2- Serum levels of cytokines in groups with and without simvastatin treatment. *p<0.01 compared with I/R, S, S+Sim Macroscopically, the ileum segments studied showed dilation and intramural hemorrhage, with higher intensity in I/R group rats, compared with the other groups. The microscopic findings revealed marked mucosal injury after ischemia and reperfusion injury; we observed most intense injury in I/R group rats compared with the other groups. The lesions most often found were: thinning of the mucosa, transmural infarction, infiltration of leukocytes in the lamina propria and mucosa. (Figures 1,2,3). Histopathological findings of I/R+Sim were comparable to those found in groups C and S. 70 DISCUSSION The HMG-CoA reductase inhibitors, including simvastatin, are used in the treatment of hypercholesterolemia, because of their effects on cholesterol biosynthesis, mevalonate pathway. Some studies have reported that statins preserve endothelial function in the absence of hypercholesterolemia, raising eNOS22,23. The activity of eNOS (nitric oxide synthase) inhibits leukocyte- endothelial interactions in microcirculation24, reducing injury during ischemia and reperfusion of myocardium25 indeed "stroke protection"26. Nitric oxide suppresses the expression of several endothelial adhesion molecules, including P-selectin, VCAM-1 and ICAM-12728. In consequence, the present study used an experimental model of ischemia and reperfusion, to verify the effect of simvastatin on intestinal injury and bacterial translocation. Some authors consider the bacterial factor, crucial in the pathogenesis of sepsis and multiple organ failure. In surgery and intensive care, intestinal obstruction and intestinal ischemia are the most associated pathological conditions2931 . This study showed that pretreatment with simvastatin attenuated the translocation 71 of bacteria to the liver, spleen and lymph nodes of rats. We used a simvastatin dose of 10 mg/kg via gavage 18 hours and 2 hours before ischemia and reperfusion, based on findings of Pruefer et al, who concluded that these are the periods with the best results of the antiinfective effects of simvastatin32. Naito et al found that pretreatment with rosuvastatin inhibited bacterial translocation, reducing the levels of cytokines in maintaining the integrity of epithelial mucosa33. A similar phenomenon occurred in the trial of Ozacmak et al. They demonstrated that atorvastatin not only preserved the ileal mucosa but also the muscle contractility after ischemia and reperfusion34. OuvirLer In the sham group without simvastatin treatment it was observed bacterial translocation only in mesenteric lymph nodes, but in Group S + Sin, some animals showed Staphylococcus aureus in the blood. As we observed growing exclusively of Gram positive bacteria, we interpreted it as a probable contamination in the isolate. The I/R+Sim group rats showed levels of bacterial translocation significantly lower in lymph nodes and liver, compared with group I/R. In the study of Pirat et al, simvastatin reduced the neutrophil infiltration and severity of injury in lung tissue in similar experimental model35. Other research found that treatment with simvastatin reversed inflammatory alterations in mice subjected to sepsis by cecal ligation and puncture, attributing these effects to the reduction of monocyte adhesion to endotelium36,37. It is known that the balance between anti-and pro-inflammatory cytokines is important in the development of bacterial translocation and septic shock. Activated leukocytes produce TNF-a and IL-6, which activate additional neutrophils to propagate inflammation32. In our study the levels of proinflammatory cytokines (TNFa, IL-1 b, IL-6) were significantly lower in I/R+Sin rats than in other groups; however, the levels of the anti-inflammatory IL-10 were higher in I/R+Sim rats than in other groups. It is attributed to IL-10 the inhibition of tissue factors released by activated monocytes via endotoxins, and reduction of expression of TNF-a by monocytes38,39. Ando et al argued that cerivastatin was able to reduce serum levels of TNF-a, IL-1 b in rats with sepsis induced by endotoxin, improving survival41. Finally, Waehre et al researching the effect of statins in patients with coronary artery disease, demonstrated significantly reduced serum levels of IL-1 in treated patients compared to controls42. In this regard, we observed that simvastatin exerted marked antiinflammatory effects, a phenomenon found in other studies38,40. 72 CONCLUSION The use of simvastatin in rats subjected to intestinal ischemia and reperfusion reduced bacterial translocation and the levels of pro-inflammatory cytokines and increased levels of anti-inflammatory cytokine, influencing the integrity of the intestinal epithelium. REFERENCES 1. Bulhak A, Sjoquist PO, Pernow J. Rosuvastatin protects the myocardium against ischaemia-reperfusion injury via inhibition of GGPP synthesis. Cardiovasc J S Afr 2004; 15: S11. 2. Weinberg EO, Scherrer-Crosbie M, Picard MH, Nasseri BA, MacGillivray C, Gannon J, Lian Q, Bloch KD, Lee RT. Rosuvastatin reduces experimental left ventricular infarct size after ischemia-reperfusion injury but not total coronary occlusion. Am J Physiol Heart Circ Physiol. 2005; 288: 1802-9. 3. Takagi T, Yoshida N, Isozaki Y, Shimozawa M, Katada K, Manabe H, Hanada O, Kokura S, Ichikawa H, Naito Y, Okanoue T, Yoshikawa T. CV- 11974, angiotensin II type I receptor antagonist, protects against ischemia- reperfusion injury of the small intestine in rats. Eur J Pharmacol. 2006;535:283- 90. 4. Naito Y, Katada K, Takagi T, Tsuboi H, Kuroda M, Handa O, Kokura S, Yoshida N, Ichikawa H, Yoshikawa T. Rosuvastatin reduces rat intestinal ischemia-reperfusion injury associated with the preservation of endothelial nitric oxide synthase protein. World J Gastroenterol. 2006;12:2024-30. 5. Endo, A., and M. Kuroda. Citrinin, an inhibitor of cholesterol synthesis. J Antibiot. 1976;29: 841-3. 6. Brown AGTC, Smale TJ, King R, Thompson RH. Crystal and molecular structure of compactin, a new antifungal metabolite from Penicillium brevicompactum. J Chem Soc. 1976; 1:1165-70. 7. Endo A.The discovery and development of HMG-CoA reductase inhibitors. J Lipid Res. 1992; 33:1569-82. 8. Sanada S, Asanuma H, Minamino T, Node K, Takashima S, Okuda H, Shinozaki Y, Ogai A, Fujita M, Hirata A, Kim J, Asano Y, Mori H, Tomoike H, Kitamura S, Hori M, Kitakaze M. Optimal windows of statin use for immediate infarct limitation: 5'- 73 nucleotidase as another downstream molecule of phosphatidylinositol 3-kinase. Circulation. 2004;110:2143-9. 9. Di Napoli P, Taccardi AA, Grilli A, De Lutiis MA, Barsotti A, Felaco M, De Caterina R. Chronic treatment with rosuvastatin modulates nitric oxide synthase expression and reduces ischemia-reperfusion injury in rat hearts. Cardiovasc Res. 2005;66:46271. 10. Hayashi T, Hamakawa K, Nagotani S, Jin G, Li F, Deguchi K, Sehara Y, Zhang H, Nagano I, Shoji M, Abe K. HMG CoA reductase inhibitors reduce ischemic brain injury of Wistar rats through decreasing oxidative stress on neurons. Brain Res. 2005;1037:52-8. 11. Laufs U, Gertz K, Dirnagl U, Böhm M, Nickenig G, Endres M. Rosuvastatin, a new HMG-CoA reductase inhibitor, upregulates endothelial nitric oxide synthase and protects from ischemic stroke in mice. Brain Res. 2002;942:23- 30. 12. Büyükafşar K, Akça T, Nalan Tiftik R, Sahan-Firat S, Aydin S. Contribution of Rho-kinase in human gallbladder contractions. Eur J Pharmacol. 2006;540:162-7. 13. Pannu R, Barbosa E, Singh AK, Singh I. Attenuation of acute inflammatory response by atorvastatin after spinal cord injury in rats. J Neurosci Res. 2005;79:34050. 14. Grots MR, Ding J, Guo W, Huang Q, Deitch EA. Comparison of plasma cytokine levels in rats subjected to superior mesenteric artery occlusion or hemorrhagic shock. Shock. 1995;3:362-8. 15. Alexander JW, Gianotti L, Pyles T, Carey MA, Babcock GF. Distribution and survival of Escherichia coli translocation from the intestine after thermal injury. Ann Surg. 1991;213:558-66. 16. Berg R, Garlington A W. Translocation of certain indigenous bacteria from the gastrointestinal tract to the mesenteric lymph-nodes and the other organs in a gnotobiotic mouse model. Infect Immun. 1979;23:403-11. 17. Caty MG, Guice KS, Oldham KT, Remick DG, Kunkel SI. Evidence for tumor necrosis factor-induced pulmonary injury after intestinal ischemia- reperfusion injury. Ann Surg. 1990; 212:694-700. 18. Galley H. F, Webster N. R. the immuno-inflammatory cascade. Br J Anaesth. 1996; 77:11-6. 19. Cunneen J, Cartwright M. The puzzle of sepsis: fitting the pieces of the inflammatory response with treatment. AACN Clin Issues. 2004;15:18-44. 74 20. Caille V, Bossi P, Grimaldi D, Vieillard-Baro A. Physiopathology of severe sepsis. Presse Med. 2004;33:256-61. 21. Park P O, Haglund U, Bulkley G B, Falt K. The Sequence of Development of Intestinal Tissue-Injury after Strangulation Ischemia and Reperfusion. Surgery. 1990; 107: 574-80. 22. O’Driscoll G, Green D, Taylor RR. Simvastatin, na HMG-Coenzyme A reductase inhibitor, improves endothelial function within 1 month. Circulation. 1997:1126-31. 23. Stalker TJ, Lefer AM, Scalia R. A new HMG-CoA reductase inhibitor, rosuvastatin, exerts anti-inflammatory effects on the microvascular endothelium: the role of mevalonic acid. Br J Pharmacol. 2001;133:406-12. 24. Pruefer D, Scalia R, Lefer AM. Simvastatin inhibits leukocyte-endothelial cell interactions and protects against inflammatory processes in normocholesterolemic rats. Arterioscler Thromb Vasc Biol. 1999;19:2894-900. 25. Lefer AM, Campbell B, Shin YK, et al. Simvastatin preserves the ischemicreperfused myocardium in normocholesterolemic rat hearts. Circulation. 1999; 100:178–84. 26. Endres M, Laufs U, Huang Z, et al. Stroke protection by 3-hydorxy-3methylglutaryl (HMG)- CoA reductase inhibitors mediated by endothelial nitric oxide synthase. Proc Natl Acad Sci USA. 1998;95:8880-5. 27. Davenpeck KL, Gauthier TW, Lefer AM. Inhibition of endothelial-derived nitric oxide promotes P-selectin expression and actions in the rat microcirculation. Gastroenterology. 1994;107:1050–8. 28. De Caterina R, Libby P, Peng HB, Thannickal VJ, Rajavashisth TB, Gimbrone MA Jr, Shin WS, Liao JK. Nitric oxide decreases cytokine-induced endothelial activation. J Clin Invest. 1995;96:60–8. 29. Stechmiller JK, Treloar D, Allen N: Gut dysfunction in critically ill patients: a review of the literature. Am J Crit Care. 199; 6:204-9. 30. Van Leeuwen PA, Boermeester MA, Houdijk AP, Ferwerda CC,Cuesta MA, Meyer S, Wesdorp RI: Clinical significance of translocation. Gut. 1994; 35:28- 34. 31. Sagar PM, MacFie J, Sedman P, May J, Mancey-Jones B, Johnstone D: Intestinal obstruction promotes gut translocation of bacteria. Dis Colon Rectum. 1995, 38:640-4. 32. Pruefer D, Makowski J, Schnell M, et al. Simvastatin inhibits inflammatory properties of Staphylococcus aureus -toxin. Circulation. 2002; 106:2104–10. 75 33. Naito Y, Katada K, Takagi T, Tsuboi H, Kuroda M, Handa O, Kokura S, Yoshida N, Ichikawa H, Yoshikawa T. Rosuvastatin reduces rat intestinal ischemiareperfusion injury associated with the preservation of endothelial nitric oxide synthase protein. World J Gastroenterol. 2006;12:2024-30. 34. Ozacmak VH, Sayan H, Igdem AA, Cetin A, Ozacmak ID. Attenuation of contractile dysfunction by atorvastatin after intestinal ischemia reperfusion injury in rats. Eur J Pharmacol. 2007;562:138-47. 35. Pirat A, Zeyneloglu P, Aldemir D, Yücel M, Ozen O, Candan S, Arslan G. Pretreatment with simvastatin reduces lung injury related to intestinal ischemiareperfusion in rats. Anesth Analg. 2006;102:225-32. 36. Merx MW, Liehn EA, Janssens U, Lütticken R, et al. HMG-Coa Reductase Inhibitor Simvastatin profoundly improve survival in a murine model of sepsis. Circulation. 2004; 109: 2560-5. 37. Merx MW, Liehn EA, Graf J, et al. Statin treatment after onset of sepsis in a murine model improves survival. Circulation. 2005;112:117-24. 38. Lindmark E, Tenno T, Chen J, Siegbahn A. IL-10 inhibits LPS-induced human monocyte tissue factor expression in human blood. Br J Haematol. 1998;102:597604. 39. Shin DI, Banning U, Kim YM, Veheyen J, Hannen M, Veheyen J, Hannan M, Bonig H. Interleukine 10 inhibits TNF-alfa production in human monocytes independently of interleukin 12 and interleukin 1 beta. Immunol Invest. 1999;28:16575. 40. Musial J, Undas A, Gajewski P, et al. Anti-inflammatory effects of simvastatin in subjects with hypercholesterolemia. Int J Cardiol. 2001; 77:247- 53. 41. Ando H, Takamura T, Ota T, Nagai Y, Kobayashi K. Cerivasatatin improves survival of mice with lipopolysaccharide-induced sepsis. J Pharmacol Exp Ther. 2000; 294: 1043-6. 42. Waehre T, Yndestad A, Smith C, Haug T, Tunheim SH, Gullestad L, Frøland SS, Semb AG, Aukrust P, Damås JK. Increased expression of interleukin-1 in coronary artery disease with downregulatory effects of HMG- CoA reductase inhibitors. Circulation. 2004;109:1966-72. 76 5.6. O Artigo foi publicado no periódico Journal of Surgical and Clinical Research. 2011:2:03-14. (ISSN: 2179-7889). Ileal interposition for the treatment of diabetes in rats: repercussion on beta cells mass Tratamento do diabetes pela interposição ileal em ratos: Repercussão na massa de células beta Layra Ribeiro de Sousa Leão, Irami Araújo Filho, MD, PhD, Amália Cínthia Meneses Rêgo, PhD, Ítalo Medeiros Azevedo, Marília Daniela Ferreira Carvalho, MD, Aldo Cunha Medeiros, MD, PhD. Research performed at University Hospital Onofre Lopes, Department of Surgery, Federal University of Rio Grande do Norte (UFRN), Brazil. Financial support: CNPq, Brazil. Conflict of interest: None. Correspondence address: Aldo Cunha Medeiros, Department of Surgery, Federal University of Rio Grande do Norte, at Ave. Nilo Peçanha 620, Natal, RN, Brazil, Email: [email protected] Submitted: 08 July 2011. Accepted, after review: 11 August 2011. ABSTRACT Purpose: Research with the aim of studying the effect of ileum interposition in hyperglycemia and pancreatic beta cell mass in nonobese diabetic rats. Methods: We used 18 Wistar rats randomly divided into 3 groups of 6 each. A non-diabetic control group, a diabetic control group, and diabetic with ileal interposition group. Induction of diabetes was underwent with streptozotocin. The beta cell mass was quantified by an indirect method by dividing the serum C-peptide (ng/mL) for blood glucose (mg / dL). We used variance (ANOVA) and Tukey's test for analysis of specific differences, considering the significance p <0.05. Results: The blood glucose of diabetic animals with ileal interposition was significantly lower (94.5 ± 5.6mg/dL) than in diabetic control rats (245 ± 4.8 mg / dL) (p <0.05). The C-peptide levels showed significantly higher in diabetes interposition group (0.58 ± 0.06 ng / mL) than in control diabetes group (0.42 ± 0.03 ng /mL), suggesting a greater response to pancreatic stimulation in that group (p <0.05). The ratio of C-peptide and glucose levels showed a higher beta cells mass in diabetic interposition animals (0.61) than in control diabetes (0.004), and the difference was significant (p<0.05). Conclusion: The results showed that the ileal interposition contributed to the reduction of blood glucose and to increase the mass of functioning beta cells in diabetic rats. 77 Key words: Diabetes. Ileum interposition. Streptozotocin. Beta cells. Rats RESUMO Objetivo: Pesquisa com o objetivo de estudar a ação da interposição do íleo terminal na hiperglicemia e na massa de células beta pancreáticas em ratos diabéticos não obesos. Métodos: Foram utilizados de 18 ratos Wistar, divididos aleatoriamente em 3 grupos de 6 cada. Um grupo controle não diabético, um grupo (controle diabético) submetido à indução do diabetes com estreptozotocina, e outro grupo diabetes submetido à interposição ileal. A massa de células beta foi quantificada por método indireto através da divisão dos níveis séricos de peptídeo-C (ng/mL) pela glicemia (mg/dL). Usados os testes de variância (ANOVA) e Tukey, para análise de diferenças específicas, considerando-se significância de p<0.05. Resultados: A glicemia dos animais diabéticos com interposição ileal foi significativamente reduzida (94,5±5.6mg/dL), quando comparada com o grupo controle diabético significativamente (245±4,8mg/dL) maiores nos (p<0,05). animais do O peptídeo-C grupo revelou diabetes níveis interposição (0,58±0,06ng/mL) do que no grupo controle diabetes (0,42±0,03ng/mL), sugerindo maior resposta à estimulação pancreática neste grupo (p<0,05). A razão entre peptídeo-C e glicemia revelou diferença significante (p<0,05), observando-se maior massa e função de células beta nos animais diabetes interposição (0,61) do que nos controle diabetes (0,004). Conclusão: Os resultados obtidos permitem concluir que a interposição ileal contribuiu para a redução da glicemia e para o aumento da massa de células beta funcionantes em ratos diabéticos. Descritores: Diabetes. Interposição. Íleo. Estreptozotocina. Células beta. Ratos. INTRODUCTION Diabetes mellitus (DM) has great importance in Brazil, because it affects 7.6% of individuals between 30 and 69 years1,2, with increasing prevalence particularly in urbanized population. The increasing prevalence is a worldwide phenomenon in the United States and a study of 18,825 adults aged >20 years showed a prevalence of 5.1% of diagnosed DM, and 2.7% of non diagnosed DM3. The DM causes cardiovascular, neurological, renal and eye complications and is among the 10 78 leading causes of morbidity and mortality in Brazil4, resulting in high costs to the health system5. The correct treatment decreases morbidity and mortality, improves quality of life, and reduce costs6,7. Type 2 diabetes is the most common form of diabetes in humans and is a combination of genetic and acquired factors that impair the function of pancreatic beta cells and tissue sensitivity to insuline8. There is evidence that beta-cell dysfunction is crucial for the development and progression of this form of diabetes9,10. Studies in patients and in isolated pancreatic islets have demonstrated quantitative and qualitative defects in insulin secretion, stimulated by glucose. Thus, there has been growing interest in the possibility of preservation of beta cells to prevent diabetes, or to prevent the progressive deterioration of glycemic control observed after diagnosis of the disease over the years10. Assuming that the beta-cell dysfunction is the key to the development and progression of type 2 diabetes, there is evidence that the beginning and triggering of disease can be slowed and the blood glucose control can be affected by certain therapeutic measures. Ideally, these beneficial effects are associated, at least in part, to the maintenance of beta cell function. For this to occur, strategies must be developed through drugs, cells and islets transplantation, or other appropriate measures. In addition, efforts should be undertaken to better understand what changes in the beta cells are present11. Obesity and diabetes mellitus (DM) have reached epidemic proportions, and the scientific world has studied new methods of treating these metabolic disorders12. Remission of diabetes has been observed after surgical procedures that affect the entero-insular axis, as is the case of bariatric surgery13,14, with improvement in glucose homeostasis independent of weight loss15,16. Bariatric surgery offers the control of diabetes and co-morbidities, leading to a change in lifestyle, having a role of surgery metabólica17. With the increasing number of bariatric surgeries, technical modifications have been explored to minimize the morbidity and associated malabsorption. However, the improvement of diabetes after bariatric surgery may be related to other factors that do not occur in non obese diabetic individuals. This applies to the large reduction in calorie intake and very fast reduction of fat tissue mass. The possibility of surgical intervention interfere with the beta cells mass has been studied18. The ileal interposition involves alteration of the intestinal tract through the 79 transposition of a segment of distal ileum for the zone of proximal jejunum. This surgery, together with the sleeve gastrectomy, has resulted in post-operative glucose control. As it does not involve bypass of small bowel and nutrients, changing in food absorption is small18,19. The hypothesis inherent in the model, initially proposed by Mason, is that the early stimulation of the ileum is an important component in the mediation and release of hormones that can improve type 2 diabetes19. Some studies have demonstrated improved glucose homeostasis in diabetic patients and in postoperative of animal models of ileal interposition18,20. Possible factors involved include the increase of hormones produced by the ileum, such as glucagon-like peptide-1 (GLP-1), which is significantly elevated after ileal interposition20. Since GLP-1 and its receptor antagonists promote the proliferation of pancreatic beta cells and reduce apoptosis, is likely that ileal interposition results in proliferation of beta cells mass21,22,23. Treatment with streptozotocin results in the destruction of beta cells and causes severe hyperglycemia in rats24. In the present study we used a streptozotocin dose enough to partial destruction of beta cells25. Assuming that the ileal interposition results in increased secretion of GLP-1, the protocol for this project worked with the hypothesis that the interposition will extend the beta cell mass and glucose tolerance in rats. The incretins, including GLP-1, are hormones secreted in the digestive tract and make the production of insulin more efficient20. The gastrointestinal bypass prevents and cures diabetes type II, stimulating the release of GLP-1 from the terminal ileum when glucose and fat come to this intestinal region25. There is no consensus about which test is best to monitor beta cell mass and function in patients with diabetes and after islet transplantation26. Many tests give variable results, are time consuming and difficult to perform. The low variability, high reproducibility and close relationship between the serum C-peptide with insulin secreted into the portal system, makes it an important tool to monitor beta cell function27. The measurement of C-peptide has been routinely performed before and after transplantation of pancreatic islets to document the survival of transplanted islets28. Plasma levels of C-peptide values depend on glucose, so that they may indicate good allograft function if the glucose is normal, but may be too low if glucose is high. Calculations involving C-peptide values in relation to blood glucose in type 2 diabetes, as well as in transplants of the pancreas and islets have been made with measurements in urine and serum29-31. In this study we used the ratio between C- 80 peptide and glucose (CP/G), which corrects the calculations according to their glycemic control32. Based on the above concepts and the fact that this is an important issue, and that this is an issue poorly understood, in this study we induced diabetes in rodents and examened the action of the ileum transposition in the mass of pancreatic beta cells and treatment of hyperglycemia in non-obese rats. OBJETIVE To examine the effect of ileal interposition in the evolution of glycemia in diabetic rats. Through an indirect method, to quantify the beta cells mass before and after ileal interposition. METHODS Animals and diet Non-diabetic Wistar rats 3 months old, were housed in individual polypropylene cages and maintained with free access to water and food (Labina - Purina ®). The protocol followed all the precepts of the Brazilian Law No. 11.794/08, which addresses the use of animals in research. Experimental protocol After acclimatization in the laboratory for 7 days, the animals were weighed. An initial dosage of glicemia was performed and the animals were randomly distributed according to the protocol in three groups: non-diabetic control group (n = 6), diabetic control (n = 6); diabetic interposition (n = 6). Diabetes induction The groups of diabetic rats were treated with a single dose of streptozotocin (STZ) (Sigma-Aldrich ®) (35 mg / kg dissolved in citrate buffer pH 4.5) to induce hyperglycemia. With this dose, not all beta cells were destroyed and theoretically this model did not create insulin-dependent diabetes. 48 hours after the use of STZ, blood glucose was measured by manual Glucometer (Accu-chek, Roche ®, Germany). 81 Surgery After defined hyperglycemia between 200 and 300 mg/dL, the rats fasted for 12 hours and they were anesthetized with thiopental (20 mg/kg) and ketamine (30 mg/kg) IM. Using aseptic technique, 3 cm midline laparotomy was performed in all of them, the cecum was exposed and the terminal was ileum identified. In the diabetes interposition group, the ileum was cut to 2 cm and 12 cm from the ileocecal valve, and an ileal loop 10 cm in length was prepared, keeping the blood supply intact. Ileoileal anastomosis was performed to reconstruct intestinal transit. The jejunum was transected 10 cm from the Treitz angle, the previously isolated ileal loop was interposed between the two ends of the jejunum by an isoperistaltic anastomosis, using 6-0 Prolene ® (Ethicon), with the aid of surgical microscope 10x (DFV, São Paulo, Brazil). Rats body weight was determined and recorded once a week after surgery and all animals were observed for 30 days. Quantification of indirect functional beta cells mass Completed 30 days of evolution, glucose concentrations were determined by the Accu-Chek (Roche, Germany). Measurement of C-peptide was performed by radioimunoassay. The ration between C-peptide and glucose levels was performed using the following formula: C-peptide/glucose ratio= C-Peptide (ng/ml) x 100 Glucose (mg/ml) All calculations were performed using measurements of C-peptide and serum glucose obtained from the same blood sample. Morbidity and Mortality All rats were examined daily from the clinical point of view during the experiment. Diarrhea, pain signals, water and food intake and weight control were measured. Statistical Analysis The data were submitted to analysis of variance (ANOVA). The Tukey test was 82 applied to analyze specific differences. Data were expressed as mean±standard deviation, considering the significant differences at p<0.05. RESULTS There was a significant difference in body weight among the 3 groups. All 18 rats survived for 30 days. Group control diabetes animals had a mean weight loss of 85±15.1 g and the diabetes interposition group had a mean weight loss of 73±13.4 g over the 30 days (p<0.05). Non diabetes control group gained a mean of 65±6.2 g. Table 1 shows the results of serum glucose and C-peptide, as well as tests to investigate the statistically significant differences between diabetic and diabetic control ileal transposition, as well as between the control non-diabetic and diabetic control rats. Table 1 – Effect of ileal interposition in serum biochemical parameters in non-diabetic control rats, diabetic control and diabetic rats undergoing ileal interposition. Data expressed as mean±standard deviation * Values significantly different compared with the diabetic control group * P <0.05, ** Values with significant difference compared with control nondiabetic and diabetic control group ** P <0.05. The analysis of Table 1 to means that the blood glucose, in diabetic animals which ileal interposition was performed, was significantly reduced, when compared with non-operated diabetic animals (p<0.05). The same profile was observed in relation to determination. Significantly higher levels of C-peptide were observed in the diabetic interposition group than in diabetic control rats, suggesting increased pancreatic stimulation response (p<0.05). Evaluation of beta cells mass Table 2 – Effect of ileal interposition on functional beta cell mass, calculated by the C- peptide/glucose ratio in non diabetic control, diabetic control and diabetic ileal 83 interposition rats. *P<0.05. Values significantly different comparing with diabetic control group. The C-peptide and glucose ratio was higher in diabetic ileal interposition group (0.61), when compared with diabetic control rats (0.004), and the difference was significant (p<0.05). Thus, we can infer that the ileal interposition contributed to increase the beta cell mass (Table 2). DISCUSSION The bariatric and metabolic surgery emerged to control morbid obesity and to treat comorbidities such as type 2 diabetes mellitus. It is known that these surgical techniques imply on restriction of food intake, malabsorption and increased release of intestinal glucagon20. On early times the improvement of metabolic alterations after bariatric surgery was exclusively attributed to weight loss. However, studies have shown that most obese and diabetic patients undergoing surgical treatment had an improvement in type 2 diabetes long before a significant weight loss33,34. The origin of this observation is related to increased release of incretins by intestine L cells, especially GLP-1. L cells are found mainly in the ileum and proximal colon and they are part of the enteroendocrine system, which is involved in the mechanism of hunger/satiety control, gastrointestinal motility, peripheral insulin sensitivity, glucose and lipid metabolism35. Anatomical abnormalities resulting from the ileal interposition stimulate the release of some hormones, mainly GLP-1, because of the early perfusion of nutrients in the distal ileum36. Thus, the ileal interposition promotes the release of incretins, without causing disabsorptive syndrome. The present study found significant improvement in blood glucose in the diabetic group after ileal interposition, compared with diabetic control group. This fact corroborates the findings of Culnan et al37, in which the early stimulation of the ileum after ileal interposition improved glucose tolerance, insulin sensitivity and muscle glucose uptake in Zucker obese rats, without changing the absorption of nutrients. Similarly, clinical study interposing a segment of 50 cm ileum 84 distal to the Treitz angle, showed the same endocrine stimulation, with reduction in serum glucose38. Strader et al39 demonstrated weight reduction associated with increased levels of GLP-1 in rats. This effect is possibly related to the anorectic effect of this hormone and peptide YY, an incretin hormone also produced by L cells. Regarding the measurement of indirect effects of incretins on the mass of functioning beta cells of animals, dosage of C-peptide in the systemic circulation has been used. C-peptide is produced by beta cells and secreted into the bloodstream. For along time, the C-peptide was considered important in the biosynthesis of insulin, but it has minimal biological activity40. However, it remains an excellent parameter to evaluate the function of pancreatic beta cells. It is equimolecular with insulin secretion, has longer half life than insulin and a negligible hepatic clearance. Many researchers prefer C-peptide concentrations instead of insulin, to detect changes in insulin secretion by beta cells27,32,40. The ileal interposition used in our study to treat diabetes in the animal model used in this study revealed a positive effect on the measurement of C-peptide. The animals of the diabetes interposition group showed levels of this peptide significantly higher than the diabetic control rats. Likewise, the analysis of the C-peptide/glicemia ratio showed a significant difference between groups ileal interposition diabetes and diabetes control. This finding validates the finding that ileal interposition results in increased beta cell mass in rats21-23. The results of this study, which is part of a research line, corroborated with the literature, demonstrate the great importance of the issue, in view of the effective potential of this surgical technique in treating diabetes and preventing its complications. Other parameters of immunogenetics, cell proliferation and hormone examination are part of further research to validate the preliminary results of this work. CONCLUSION The results showed that the ileal interposition was beneficial for the evolution of blood glucose and contributed to increased beta cell mass in diabetic rats. 85 REFERENCES 1. Malerbi DA, Franco LJ. Multicenter study of the prevalence of diabetes mellitus and impaired glucose tolerance in the urban Brazilian population aged 30-69 yr. The Brazilian Cooperative Group on the Study of Diabetes Prevalence. Diabetes Care. 1992; 15:1509-16. 2. Oliveira JE, Milech A, Franco LJ. The prevalence of diabetes in Rio de Janeiro, Brazil. The Cooperative Group for the Study of Diabetes Prevalence in Rio de Janeiro. Diabetes Care. 1996; 19:663-9. 3. Harris Ml, Flegal KM, Cowie CC, Eberhardt MS, Goldstein, et al. Prevalence of diabetes, impaired fasting glucose, and impaired glucose tolerance in US adults (The Third National Health and Nutrition Examination Survey, 1988-1994). Diabetes Care. 1998;21:518-24. 4. Laurenti R, Fonseca LA, da Costa Júnior ML. Diabetes mellitus mortality in the municipality of São Paulo (Brazil). Evolution over a period of 79 years (1900-1978) and analysis of some aspects of the association of causes. Rev Saude Publ. 1982;16:77-91. 5. Hart WM, Espinosa C, Rovira J. Costs of known diabetes mellitus in Spain. Med Clin. 1997;109:289-93. 6. Santiago JV. Intensive management of insulin dependent diabetes: risks, benefits and unanswered questions. J Clin Endocrinol Metab. 1992;75:977-80. 7. Harris Ml. Diabetes in America: Epidemiology and scope of the problem. Diabetes Care. 1998;21(supl 3):11-4. 8. American Diabetes Association: Diagnosis and classification of diabetes mellitus. Diabetes Care. 2008; 31 ( Suppl. 1): S55– S60. 9. Stumvoll M, Goldstein BJ, van Haeften TW. Type 2 diabetes: principles of pathogenesis and therapy. Lancet. 2005; 365: 1333– 46. 10. Marchetti P, Dotta F, Lauro D, Purrello F. An overview of pancreatic beta-cell defects in human type 2 diabetes: implications for treatment. Regul Pept. 2008; 146: 4– 11. 11. Astrup A, Finer N. Redefining type 2 diabetes: “diabesity” or “obesity dependent diabetes mellitus”? Obes Rev. 2000;1:57–9. 12. Sjostrom L, Lindroos AK, Peltonen M, Torgerson J, Bouchard C, Carlsson B, Dahlgren S, Larsson B, Narbro K, Sjostrom CD, Sullivan M, Wedel H. Lifestyle, 86 diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med. 2004;351:2683–93. 13. Greenway SE, Greenway FL, Klein S. Effects of obesity surgery on non-insulindependent diabetes mellitus. Arch Surg. 2002;137:1109–17. 14. Flatt PR. Effective surgical treatment of obesity may be mediated by ablation of the lipogenic gut hormone gastric inhibitory polypeptide (GIP): evidence and clinical opportunity for development of new obesity-diabetes drugs? Diabetes Vasc Dis Res. 2007;4:151–3. 15. Cohen RV, Schiavon CA, Pinheiro JS, Correa JL, Rubino F. Duodenal-jejunal bypass for the treatment of type 2 diabetes in patients with body mass index of 22– 34 kg=m2: a report of 2 cases. Surg Obes Relat Dis. 2007;3:195–7. 16. Kawamura I, Ochiai T. Current status of obesity surgery as metabolic surgery. Nippon Geka Gakkai Zasshi. 2006;107:305–11. 17. Patriti A, Facchiano E, Annetti C, et al. Early improvement of glucose tolerance after ileal transposition in a non-obese type 2 diabetes rat model. Obes Surg. 2005;15:1258–64. 18. Atkinson RL,Whipple JH,Atkinson SH, et al. Role of the small bowel in regulating food intake in rats. Am J Physiol. 1982;242:429–33. 19. Mason EE. Ileal correction of ilial transposition and enteroglucagon/GLP-1 in obesity (and diabetic?) surgery. Obes Surg. 1999;9:223–8. 20. Strader AD, Vahl TP, Jandacek RJ, et al. Weight loss through ileal transposition is accompanied by increased ileal hormone secretion and synthesis in rats. Am J Physiol Endocrinol Metab. 2005;288:447–53. 21. Perfetti R, Zhou J, Doyle ME, et al. Glucagon-like peptide-1induces cell proliferation and pancreatic-duodenum homeobox-1 expression and increases endocrine cell mass in the pancreas of old, glucose-intolerant rats. Endocrinology. 2000;141:4600–5. 22. U G, Stoffers DA, Habener JF, et al. Exendin-4 stimulates both beta-cell replication and neogenesis, resulting in increased beta-cell mass and improved glucose tolerance in diabetic rats. Diabetes. 1999;48:2270–6. 23. Araújo-Filho I, Jácome DT, Rego AC, Azevedo IM, Egito EST, Medeiros AC. Efeito da sinvastatina na sepse abdominal de ratos diabéticos. Rev Col Bras Cir. 2010;37:31-8. 24. Li Y, Hansotia T, Yusta B, et al. Glucagon-like peptide-1 receptor signaling 87 modulates beta cell apoptosis. J Biol Chem. 2003;278:471–8. 25. Ferrannini E, Mari A. Beta cell function and its relation to insulin action in humans: a critical appraisal. Diabetologia. 2004; 47: 943–56. 26. Palmer JP, Fleming GA, Greenbaum CJ et al. C-peptide is the appropriate outcome measure for type 1 diabetes clinical trials to preserve beta-cell function. Diabetes. 2004; 53: 250–64. 27. Alejandro R, Lehmann R, Ricordi C et al. Long-term function (6 years) of islet allografts in type 1 diabetes. Diabetes. 1997; 46: 1983–9. 28. Secchi A, Pontiroli AE, Traeger J et al. A method for early detection of graft failure in pancreas transplantation. Transplantation .1983; 35: 344–8. 29. Matsumoto S, Yamada Y, Okitsu T et al. Simple evaluation of engraftment by secretory unit of islet transplant objects for living donor and cadaveric donor fresh or cultured islet transplantation. Transplant Proc. 2005; 37: 3435–7. 30. Yamada Y, Fukuda K, Fujimoto S et al. SUIT, secretory units of islets in transplantation: an index for therapeutic management of islet transplanted patients and its application to type 2 diabetes. Diabetes Res Clin Pract. 2006; 74: 222–6. 31. Faradji RN, Monroy K, Messinger S, Pileggi A, Froud T, Baidal DA, Cure PE, Ricordi C, Luzi L, Alejandro R. Simple measures to monitor b-cell mass and assess islet graft dysfunction. Am J Transpl. 2007; 7: 303–8. 32. Farilla L, Hui H, Bertolotto C, Kang E, Bulotta A, Di Mario U, Perfetti R. Glucagonlike peptide-1 promotes islet cell growth and inhibits apoptosis in Zucker diabetic rats. Endocrinology. 2002;143:4397-408. 33. Farilla L, Bulotta A, Hirshberg B, Calzi SL, Khoury N, Noushmehr H, Bertolotto C, Di Mario U, Harlan DM, Perfetti R. Glucagon-like peptide-1 inhibits cell apoptosis and improves glucose responsiveness of freshly isolated human islets. Endocrinology. 2003;144:5149-58 34. Vilsboll T, Krarup T, Sonnie J, Madsbad S, Volund A, Juul AG, Holst JJ. Incretin secretion in relation to meal size and body weight in healthy subjects and people with type 1 and type 2 diabetes mellitus. J Clin Endocrinol Metab. 2003;88:2706- 13. 35. Sugiyama K, Manaka H, T Kato, Yamatani K, M Tominaga, e Sasaki H. Estimulação da truncado glucagon-like peptide-1 liberação do íleo isolado perfundido canina pela absorção de glicose. Digestão 55:. 24-28, 1994 36. Culnan DM, Albaugh V, Don M, Lynch CJ , Lang CH, Cooney RN. Interposição ileal melhora a tolerância à glicose e a sensibilidade à insulina em ratos obesos 88 Zucker. Am. J. Physiol. Gastrointest Liver Physiol. 2010;299:G751-G750. 37. De Paula AL, Macedo ALV, Schraibam V, Machado CA. Gastrectomia com interposição ileal (freio neuroendócrino) como opção de tratamento cirúrgico da obesidade mórbida. Bariátr Metabol. 2007;1:47-53. 38. Strader AD, Vahl TP, Jandacek RJ, Woods SC, D’Alessio DA, Seeley RJ. Weight loss through ileal transposition is accompanied by increased ileal hormone secretion and synthesis in rats. Am J Physiol Endocrinol Metab.2005;288:E447– E453. 39. Forst T, Hach T, Kunt T, Weber MM, Pfützner A. Molecular effects of C-Peptide in microvascular blood flow regulation. Rev Diabet Stud. 2009; 6:159-167. 89 5.7. O Artigo foi publicado no periódico Journal of Surgical and Clinical Research. 2011;2:42-50. (ISSN: 2179-7889). Hepatectomy for benign and malign diseases in University Hospital Hepatectomia para doenças benignas e malignas em Hospital Universitário Marilia Daniela Ferreira Carvalho, MD; Irami Araújo-Filho, MD, PhD; Amália Cínthia Meneses Rêgo, PhD; Ítalo Medeiros Azevedo, Aldo Cunha Medeiros, MD, PhD. Research performed at University Hospital Onofre Lopes, Department of Surgery, Federal University of Rio Grande do Norte (UFRN), Brazil. Financial support: None. Conflict of interest: None. Correspondence address: Marília Daniela Ferreira Carvalho, Department of Surgery, Federal University of Rio Grande do Norte, at Ave. Nilo Peçanha 620, Natal, RN, Brazil, Email: [email protected]. Submitted: 01 December 2010.Accepted, after review: 27 July 2011. ABSTRACT The hepatectomy is a surgical modality devoted to the treatment of benign and malignant conditions of the liver. This retrospective study aims to analyze the main clinical and technical aspects concerning to 33 Resections performed from July 2006 to July 2010, at the Hospital Universitário Onofre Lopes. Showed agreement between the sexes, most patients in the interior of our state, major comorbid hypertension and complication fistula and mortality of 12%, surgery was performed over the right trissegmentectomy, 21% of pacientes had gallbladder cancer and 12% metastatic colon cancer. The age ranged 25-84th, 51st average. 45% had no comorbidities, 30% were hypertensive. The operative time ranged from 110-660min, mean 314.6 min, length of stay 02-69 days, average 16d. Hepatic surgery has become more feasible in recent years because of the best preoperative evaluation which allowed the control of postoperative complications. Keywords: hepatectomy, liver surgery, liver resections. 90 INTRODUCTION Liver resections characterized a major challenge for the surgeon in the past due to its high mortality, but currently the mortality rate is around 5% in important medical centers1. Today it is a surgical procedure for the treatment of benign hemangiom, hepatocellular adenoma and malignant diseases as the primary hepatocellular carcinoma and hepatoblastoma in childhood, in addition to metastasis of colorectal carcinomas and rare tumors gastrinomas and carcinoids2. Hepatocellular carcinoma (HCC) is the sixth most common cancer in the world and the third most common cause of cancer-related death3. Patients at the early stage of disease are those who present with an asymptomatic single HCC with the nodule < 5 cm in diameter or ≤ 3 in number. Patients exceeding these limits, but free of cancer-related symptoms and vascular invasion or extrahepatic spread, are considered at the intermediate stage. The patients with the cancer-related symptoms and vascular invasion or extrahepatic spread are deemed at the advanced stage. HCC is frequently diagnosed at the late stage and has a high mortality rate4. This increase of cases occurs because of the spread of hepatitis viruses B and C5,6. The liver is a frequent site of metastasis of solid tumors. The treatment of liver metastases of colorectal tumors is already well established, but colorectal tumors for therapy is not well defined7. Currently 15 to 25% of patients diagnosed with colorectal tumors have liver metastasis and 25 to 50% of them will develop metastases within three years. Surgical resection of colorectal metastases is the only curative option and this procedure can guarantee the survival of 25 to 50% in 5 years8. Surgical resection is a potentially curative therapy for HCC. However, only 10%-30% of patients with HCC are eligible for curative hepatectomy9. Radical resection is still the first choice for treatment of HCC10, even at the intermediate or advanced stage11. If radical resection is impractical, palliative resection combined with comprehensive therapy can significantly prolong patients’ survival time12. Despite medical advances with new modalities of treatment for liver, resection is still the best curative therapy8,13. The aim of this work was to analyze the epidemiological data and surgical treatment performed on all the patients submitted to hepatectomy in a University Hospital during a five years interval. 91 METHODS Based on the information stored in the program in 2000 MV ®, developed by VM software and consulting, we selected the surgeries registered as hepatectomies performed between July 2006 and July 2010, at the Onofre Lopes University Hospital, and found 41 procedures, but when performed after reading the charts, only 33 were included. These eight charts were disregarded as they were non-surgical treatments consistent with the proposed surgical or medical records with incomplete information. The data of interest for the work were organized in tables, and these were worked in the Microsoft Office Excel ® 2003 for the construction of statistical data and graphs. RESULTS Demographic characteristics of 33 patients are presented in Figure 1. Female patients predominated (n=17; 51%), and the median age was 51 years (range, 25– 84). 64% of patients were from provincial small towns and 36% from the capital (Figure 2). Figure 1-Distribution by gender. 92 Figure 2 - Distribution by city origin. With regard to co-morbidities, 45% of patients had any associated diseases, 30% were hypertensive, 12% were smokers, 9% alcoholics,12% had a history of diabetes mellitus treatment before surgical resection, and 6% had chronic pancreatitis.The percentage of patients with chronic renal failure, cardiac arrhythmia and Crohn's disease was 3% each (Figure 3). Figure 3 - Distribution of comorbidities. With regard to diseases that originated the hepatectomy, gallbladder cancer occurred in 21% of cases, hepatic metastasis of colon cancer in 12% and GIST in 93 3% of cases. Klatskin tumor, adjacent tumor invasion, metastasis from neuroendocrine tumors, tumors of undetermined origin, benign cysts and hemangiomas contributed with 9%; hepatocellular carcinoma occurred in 6% of patients and iatrogenic lesions of the bile duct in 3% of cases (Figure 4). Figure 4 - Distribution of diseases that originated resections The operative time ranged from 110 to 660 minutes (mean of 314.6 minutes).The length of hospital stay was from 2 to 69 days (average 16 days). The stay in the intensive care unit ranged from 0 to 13 days, with an average of 3 days. 60.6% of patients were transfused during surgery or during hospitalization, and 6% had autotransfusion during surgery; 33.3% were not transfused. Only 9% of patients received i.v. human albumin. Anatomical resection predominated (n=25; 75.7%). Seven of them (21.2%) underwent major resection exceeding hemihepatectomy, and 4 underwent extended bisegmentectomy. Eight patients (24.3%) underwent non-anatomical (atypical) resections. These data are summarized in Table 1. 94 Table 1-Types of resections. The most common complication was fistula (18%), followed by abscess (15%). Nine percent of patients developed sepsis, acute renal failure occurred in 6% and intra- abdominal hematoma in 6%. Other complications such as stroke, bilioma, empyema, pleural fistula, liver failure, coagulopathy, atrial fibrillation, liver failure and pneumonia totalized 3% each (Figure 5). Four patients (12%) died during hospitalization. Figure 5 - Postoperative complications. 95 DISCUSSION Liver resection is a complex surgery to be performed by experienced surgeons in specialized centers. For many years it was associated with increasing morbidity and mortality. After the study of functional anatomy and physiology of liver regeneration, performed by Couinaud, major advances in this area led to the current period that witnessed satisfactory results14. As surgical techniques improved over the last recent decades, after a good understanding of modern liver anatomy15, hepatic resection is now considered a safe procedure and the gold standard of curative treatment. Nevertheless, surgical resection is often contraindicated due to deterioration of hepatic function and excessive tumor burden, both of which may result from delayed diagnosis. Fortunately, early diagnosis of HCC has recently increased because of regular examination of high-risk patients and advancement of radiological diagnostic techniques. One of the most relevant factor of successfull hepatectomy is the advancement of pre-operative radiological workup for the diagnosis and study of injuries, often in early stage, including the intraoperative ultrasonography. This modernization of radiology is reflected not only in diagnosis but also in therapy1. Despite the decrease in surgery-related mortality and the increase in possible surgical approaches, long-term outcome of surgical resection remains unsatisfactory in many cases due to early recurrence16. Analyzing our data with regard to gender, there was a similarity between them. We found that most of our patients came from provincial small towns (interior) of Rio Grande do Norte State, Brazil. This is understandable, since HUOL is a reference public regional hospital. The age had a very wide range (25-84 years). One of the deaths occurred in a young patient (25 years) with colon carcinoma and extensive liver metastasis. In our series there was still a death in a patient with an initial indeterminate diagnosis. The definitive diagnosis revealed benign disease. The mortality in our series was 12% and is consistent with the literature of important centers, around 3-15%2. Most patients who died had malignant disease, jaundice and malnutrition. It was noted high morbidity and mortality, length of intensive care unit and hospital stay in patients undergoing liver resection due to cancer of the bile ducts. Some patients stayed for a long time in intensive care unit because of the need for ventilatory assistance and sepsis. Co-morbidities were conveniently evaluated 96 and treated to minimize postoperative complications. The main comorbidity found was hypertension, which is consistent with the literature, followed by smoking and alcoholism2. The hepatectomy was more frequently performed in cases of gallbladder cancer. This certainly is due to the high prevalence of biliary tract diseases operated in our hospital, not infrequently faced with a pathological diagnosis of malignancy. The metastasis of colon cancer was the cause of our second indication of hepatectomy. Only three patients were operated with benign diseases. Abscess and biliary fistula were the main postoperative complications. Based on these informations we emphasize the real need to encourage studies like this, revealing the particular aspects of our service, for the knowledge of our reality. These findings may guide our future steps in surgical liver diseases. In conclusion, these data showed that morbidity and mortality posthepatectomy was compatible with literature and that radiological and functional assessment permitted hepatectomy including anatomic resection and optimal pathologic margins. Measures to minimize postoperative morbidity were implemented. REFERENCES 1. Marrero JA, Welling T. Modern diagnosis and management of hepatocellular carcinoma. Clin Liver Dis. 2009;13:233-47. 2. Araújo GF, Costa OM, Santos MF et al. Hepatectomias: Análise crítica retrospectiva de 21 casos. Rev Bras Cir. 2002;29:161-5. 3. Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA Cancer J Clin. 2005; 55: 74-108. 4. Rampone B, Schiavone B, Martino A, Viviano C, Confuorto G. Current management strategy of hepatocellular carcinoma. World J Gastroenterol 2009; 15: 3210-6. 5. Zhou Y, Sui C, Li B et al. Repeat hepatectomy for recurrent hepatocellular carcinoma: a local experience and systematic review. World J Surg Oncol. 2010,8: 55. 6. WaechterFL, SampaioJA, PintoRDetal. Utilização das hepatectomias centrais nas cirurgias hepatobiliares. Rev Col Bras Cir. 2000;27:413-21.] 7. Choi EA, Abdalla EK. Patient selections and outcomes of hepatectomy for non colorectal non-neuroendocrine liver metastases. Surg Oncol Clin N Am. 97 2007:16;557-7. 8. Lupinacci R, Penna C, Nordlinger B. Hepatectomy for respectable colorectal cancer metastases-Indicators of prognosis, definition of respectability, thecniques and outcomes. Surg Oncol Clin N Am. 2007:16;493-06. 9. Yau T, Chan P, Epstein R, Poon RT. Evolution of systemic therapy of advanced hepatocellular carcinoma. World J Gastroenterol. 2008; 14: 6437-41. 10. Liu JH, Chen PW, Asch SM, Busuttil RW, Ko CY. Surgery for hepatocellular carcinoma: does it improve survival? Ann Surg Oncol. 2004; 11: 298-303. 11. Wakabayashi H, Ushiyama T, Ishimura K, Izuishi K, Karasawa Y, Masaki T, Watanabe S, Kuriyama S, Maeta H. Significance of reduction surgery in multidisciplinary treatment of advanced hepatocellular carcinoma with multiple intrahepatic lesions. J Surg Oncol. 2003; 82: 98-103. 12. Lin DX, Zhang QY, Li X, Ye QW, Lin F, Li LL. An aggressive approach leads to improved survival in hepatocellular carcinoma patients with portal vein tumor thrombus. J Cancer Res Clin Oncol.2011; 137: 139-49. 13. Jaeck D, Oussoultzoglou E, Rosso E. Hepatectomy for colorectal metastases in presence of extrahepatic disease. Surg Oncol Clin N Am. 2007;16:507-23. 14. Chen J, Huang K, Wu J, Zhu H, Shi Y, Wang Y, Zhao G. Survival after anatomic resection versus non anatomic resection for hepatocellular carcinoma: a metaanalysis. Dig Dis Sci. 2011;56:1626-33. 15. Trivino T, Abib SC. Anatomia cirúrgica do fígado. Acta Cir Bras. 2003;18:407-14. 16. Agrawal S, Belghiti J. Oncologic resection for malignant tumors of the liver. Ann Surg. 2011;253:656-65. 98 5.8. O Artigo foi publicado no periódico Journal of Surgical and Clinical Research. 2011;2:78-86. ISSN: 2179-7889. Sildenafil as a vasodilatatory mediator in the treatment of abdominal sepsis Sildenafil como um mediador vasodilatador no tratamento de sepse abdominal Marília Daniela Ferreira Carvalho, Ingrid Tinôco Silvestre, Amanda Jayne Guedes Risuenho, Amália Cínthia Meneses Rêgo, Irami Araújo-Filho, Ítalo Medeiros Azevedo, Aldo Cunha Medeiros Research performed at Department of Surgery, Federal University of Rio Grande do Norte (UFRN), Brazil. Financial support: CNPq, Brazil. Conflict of interest: None. Correspondence address: Marília Daniela Ferreira Carvalho, Department of Surgery, Federal University of Rio Grande do Norte, at Ave. Nilo Peçanha 620, Natal, RN, Brazil, Email: [email protected] Submitted: 08 October 2011. Accepted, after review: 11 December 2011. ABSTRACT Objective: To analyse the effects of previous treatment with sildenafil in rats with abdominal sepsis induced by cecal ligation and puncture (CLP). Methods: Wistar rats were randomly allocated in 3 groups of 6 each. Sham group (SG): rats were subjected to laparotomy and no induction of sepsis; CLP/sil: rats subjected to cecal ligation and puncture, treated with sildenafil 1mg/Kg via gavage, 60 min before sepsis induction; CLP group: rats with sepsis, no sildenafil. After anesthesia under aseptic technique, we underwent a laparotomy and CLP. Postoperative pain was controlled with tenoxicam 3mg/Kg, i.m. The rats were observed for 24 hs, and examined on the late stage of polymicrobial abdominal sepsis. Body weight, leukogram, C-reactive protein, TNF-α, IL-1β, IL-6, IL-10. Statistical analysis was done by ANOVA and Tukey test, with significance p<0.05. Results: Group CLP rats had their weight reduced in 12% when compared with sham rats (p<0.05). However, comparing the sham and CLP/sil rats the diference on weight loss was not 99 significant. Leukocytes and neutrophils counts were significantly elevated in group CLP rats compared with sham (p<0.05). In CLP/sil group rats a decreased total leukocyte and neutrophil counts were detected, compared with the CLP group (p<0.05). Reduced levels of C-reactive protein in the LPC/sil group were observed, compared with CLP rats (p<0.05). Serum levels of TNF-α, IL-1β and IL-6 were lower in the CLP/sil rats, compared with untreated CLP animals (p<0.05). Increased IL-10 in the CLP/sil rats, compared with CLP rats, demonstrated a protective effect on the vasodilatory sepsis. Conclusion: The data revealed that the pretreatment of abdominal sepsis with the vasodilator sildenafil favorably influenced the evolution of inflammation and immune response in rats. Keywords: Abdominal Sepsis. Treatment. Sildenafil. Vasodilation. Cytokines. Rats. RESUMO Objetivo: Analisar os efeitos do tratamento prévio com sildenafil em ratos com sepse abdominal induzida por ligadura e punção do ceco. Métodos: Ratos Wistar foram distribuídos aleatoriamente em 3 grupos de 6 animais cada. Grupo Sham (GS): Animais submetidos a laparotomia sem indução da sepse; grupo LPC/sil: Ratos submetidos à ligadura e punção do ceco (LPC) tratados com sildenafil 1mg/kg via oral por gavagem, 60 minutos antes da indução da sepse; grupo LPC: indução de sepse, sem uso do sildenafil. Após anestesia e com técnica asséptica, foi realizada laparotomia mediana e LPC. Dor pós-operatória controlada tenoxicam i.m. 3 mg/Kg. Os animais foram observados até completar 24 horas, estágio tardio e hipodinâmico da sepse abdominal polimicrobiana. Foram analisados: Peso dos animais, leucograma, dosagem sérica de proteína C reativa, TNF-α, IL-1β, IL-6 e IL10. Análise estatística pelo ANOVA e teste de Tukey, significância p<0,05. Resultados: Redução de 12% do peso dos animais do grupo LPC quando comparado com grupo sham (p<0,05). Comparação entre o grupo sham e LPC/sil não revelou diferença significante. A quantificação de leucócitos totais e neutrófilos revelou aumento significante nos animais do grupo LPC quando comparado com o grupo sham (p<0,05). No grupo LPC/sil houve redução de leucócitos totais e neutrófilos, comparando-se com o grupo LPC (p<0,05). Houve redução dos níveis de proteína C reativa no grupo LPC/sil, em comparação com o grupo LPC (p<0,05). Redução significante da expressão de TNF-α, IL-1β e IL-6 no grupo LPC/sil em 100 comparação com os animais não tratados (p<0,05). O aumento de IL-10 no grupo LPC/sil, comparado com o grupo LPC sugeriu efeito protetor do vasodilatador sobre o quadro séptico. Conclusão: Os dados permitem afirmar que o pré-tratamento da sepse abdominal com o vasodilatador sildenafil influenciou a evolução favorável da inflamação e da resposta imune em ratos. Descritores: Sepse abdominal. Tratamento. Sildenafil. Vasodilatação. Citocinas. Ratos. INTRODUCTION Sepsis is a disease whose pathophysiology is linked to an imbalance between anti-inflammatory and pro-inflammatory substances that will mediate a response to damage to organs caused by infection. The infection process may be initiated by gram-negative, gram-positive and anaerobic bacteria, fungi, protozoa and/or virus, the latter being in smaller proportions. Gram-negative bacteria are the main cause of sepsis1. In spite of increasing advance on the treatment of sepsis, this is still a major cause of death in intensive care units, has a high cost, as diagnosed in the last two decades, especially in polytraumatized patients in use of catheters, mechanical ventilation, steroid-dependent patients and those with pneumonia2. By using video-microscopy in vivo, investigators have demonstrated in rats models that sepsis is characterized by decreased rate of flow in the microcirculation, increased heterogeneity of flow, increased vascular stasis and decreased capillary perfusion3. The ideal therapy for improving the microcirculation must modulate endothelial function prematurely and cause vasodilation of low flow units. Treatment with vasodilators (prostacyclin) and a mixture of inotropes/vasodilators (dobutamine) have been used for this purpose and have demonstrated an increase in systemic oxygen consumption, suggesting improvement in microcirculation4-6. Recently there has been considerable interest in investigating the role of sildenafil in protecting ischemic and reperfusion injury in animals7. This is a new class of vasoactive drugs that have been developed for the treatment of erectile dysfunction. Its mechanism of action involves active inhibition of type 5 phosphodiesterase enzyme that increases cGMP, nitric oxide (NO) and improves endothelial 101 dysfunction8. Based on these aspects of interaction between microcirculation and its effects on sepsis and in the vasoactive effects of sildenafil, the present experimental model aims to analyze the effects of previous use of sildenafil in abdominal sepsis induced by cecum ligation and puncture in rats. METHODS Rats sample We used 18 Wistar rats weighing 280±18g, from the Center for Health Sciences, Federal University of Rio Grande do Norte, Brazil. The experimental protocol and the care of the animals were in accordance with the Animal Welfare Act and Brazilian Law 11,794/2009. This project was approved by the Institutional Animal Care and Use Committee of UFRN, Brazil. The animals were kept in an adaptive period of seven days and throughout the experiment they were observed at the Nucleus for Experimental Surgery in individual cages with water and standard food for rodents (Labina-Purina ®) ad libitum, subjected to light-dark cycle of 12 hours with humidity and noise control. Experimental design The animals were randomly distributed into 3 groups of 6 animals each, with the following characteristics: Sham group (SG) - Sham-operated rats (control) underwent laparotomy and the cecum was neither ligated nor punctured. Group CPL /sil – The rats underwent cecal ligation and puncture (CLP) and were treated with sildenafil. CPL Group - Induction of sepsis, without sildenafil treatment. Sildenafil treatment In groups SG and CLP/sil the rats were treated with sildenafil (Pfizer, Brazil) suspension 1mg/kg by gavage, 60 minutes before sepsis induction. Operative procedures Rats were fasted overnight (16 h) before the induction of sepsis but allowed water adlibitum. They were anesthetized with ketamine 50mg/kg body weight and xilazine 20 mg/kg (intramuscular), their abdomens were shaved, and a 4-cm ventral 102 midline incision was made. The cecum was exposed and isolated by ligation with a 30 cotton ligature just distally to the ileocecal valve to avoid intestinal obstruction. The cecum was punctured twice at opposite ends with an 18-gauge needle and confirmation of the punctures was established by forcing a small amount of the cecal contents out of the cecum. The ligated and punctured cecum was then returned into the abdominal cavity. The abdominal incision was then closed in two layers using a 4-0 nylon suture and the animals received 3 mL per 100 g body wt of normal saline solution subcutaneously (i.e., fluid resuscitation). Postoperative examinations The animals were observed for 24 hours, considering that 24 hours after CPL represents the late stage of hypodinamic polymicrobial abdominal sepsis1. The following parameters were analyzed: 1) Weighing of the animals at the beginning and end of the experiment on a digital scale. 2) Collection of blood through cardiac puncture at the end of the observation period for leukocytes and neutrophils count in automatic cell counter (AbbottCell-Dyn 3500R-CD 3500 5L, USA). Blood serum was separated by centrifugation at 2000rpm and stored at -40°C for subsequent dosage. C-reactive protein was analyzed by autoanalyzer (BT Plus WeinerLab 3000). TNF-α, IL-1β, IL-6 and IL-10 were assayed by ELISA (enzyme-linked-immunosorbentassay), an analytical methods based on antigen-antibody interaction used to determine specific amounts of protein in tissue samples and body fluids. The reagents were from PeproTech, NJ, USA. Observation of animal behavior (presence or absence of hair bristling, lethargy and dark circles around the eyes), morbidity, mortality and weight control were done. Data were statistically analyzed by ANOVA and the Tukey test, considering differences significant when p <0.05. RESULTS There was a 12% weight loss on the CLP animals compared with sham group (p<0.05). When the comparison was made between the sham group and the CLP/sil group, no significant difference was observed. All animals in LPC group showed lethargy, hair bristling and dark circles around the eyes after 24 hours. These findings were not observed in animals from other groups. 103 The leukocytes and neutrophils counts showed significant increase in CLP group animals when compared to the sham group (p<0.05). Treatment with sildenafil (CLP sil group) reduced the levels of leukocytes and neutrophils, compared with the CLP group (p<0.05). We observed a decrease in the levels of C-reactive protein in the LPC/sil group rats, indicating a lower inflammatory response in this group compared with CLP group (p <0.05), whose numerical data are shown in Table 1. Table 1 - Results of leukocytes, neutrophils counts and measurement of C-reactive protein. *p<0.05 vs. grupos CLP, CLP/Sil; ** p<0.05 vs. grupos Sham, CLP /sil. Inflammatory cytokines The serum levels of proinflammatory cytokines TNF-α, IL-1β and IL-6 showed a significant reduction (p<0.05) in the group previously treated with sildenafil (CLP/sil) compared with untreated animals. The serum level of the anti-inflammatory cytokine L-10 was significantly higher in CLP rats than in CLP/sil animals, meaning a protective effect on the vasodilator sepsis. Numerical data are summarized in Table 2. Table 2 – Values of serum cytokines on each group rats. *p<0.05 vs. CLP, CLP/Sil groups; ** p<0.05 vs. Sham, CLP groups. DISCUSSION Sepsis has a high mortality rate, with estimated values between 20 and 50% 104 and several studies have been developed in the search for more effective therapies to reverse sepsis2,9-11. In the present study, we verified the effectiveness of sildenafil as a protector against the effects of sepsis caused by CLP. The pathophysiology of this disease is related to an inflammatory response to infection. There is an exacerbation in the release of inflammatory modulators and excessive activation of inflammatory cells, meaning that the patients own defense can’t control the disease. This may evolve into a severe sepsis until the failure of multiple organs, leading to death1. The presence of gram-negative bacteria in the peritoneal cavity triggers the release of endotoxins and exotoxins that stimulate the expression of primary modulators through activation of macrophages and monocytes. TNF-α and IL-1β are some of these modulators, particularly TNF-α has been shown to be the most involved in the development of septic shock. In the current study the pretreatment with the vasodilator sildenafil interfered on the level of these pro-inflammatory cytokines by reducing them in significant amounts in comparison with the untreated group. This reduction was important to demonstrate that pretreatment with sildenafil may act in the attenuation of the inflammatory response during sepsis. Cadirci et al demonstrated that sildenafil attenuated exacerbated release of the pro-inflammatory cytokine TNF-α in a study in which sildenafil was also used in rats subjected to CLP12. IL-6 is another cytokine that appears to be the an efficient promoter on hepatic production of acute phase proteins as the C-reactive protein, a very sensitive marker of systemic inflammation. Damas et al13 demonstrated that IL-6 acts as a second messenger released by macrophages, endothelial cells, fibroblasts and other cells in response to sepsis. As seen in the quantitative evaluation of the present study, pretreatment with sildenafil resulted in a significant reduction in IL-6 and Creactive protein levels, suggesting that these two mediators are correlated during development of the sepis. The exaggerated inflammatory response that occurs in sepsis is counterbalanced by the early and sustained expression of potent anti-inflammatory cytokines such as IL-10. In sepsis, IL-10 has been identified as a modulator of the production of frequently lethal proinflammatory cytokines. Neutralization of IL-10 results in increased expression of proinflammatory cytokines and death, while the administration of its recombinant form provides therapeutic protection14. Thus, the increase in IL-10 in rats of CLP/sil group was certainly an important moderating and 105 neutralizing factor on the intense inflammatory process induced by sepsis. Happening pro-inflammatory stimuli, such as IL-1, IL-6 and TNF-α, or oxidative stress15, endothelial activation occurs, leading to a procoagulant environment, proadhesive cell surfaces, dysregulation of vasomotor tone, and compromised barrier function. This inflammatory environment is further propagated by the release of additional cytokines directly from endothelial cells, which leads to local microvascular damage, disrupted tight junctions, edema, and tissue hypoxia1,15. In the presence of infectious focus, endotoxins and cytokines will activate cellular and humoral immune response. The first line of defense against infections after natural barriers are the monocyte-macrophages. Furthermore, the presence of TNF-α, IL-1β and IL-6 also activates other cells or blood components such as the polymorphonuclear cells1. In the present study we detected an increased migration of leukocytes to circulation and to the infectious focus in the CLP rats, showing that there was an intense attraction to the infected site by chemotactic factors. The use of sildenafil, however, by reducing the intensity of the infectious process, required a smaller amount of immune cells during sepsis. This was validated by the reduction of total leukocytes and neutrophils in the rats of CLP/sil group compared to the CLP group. Kukreja et al demonstrated that sildenafil induces cardioprotective effect against ischemia and reperfusion in dogs, rabbits, rats and mice. The effect was attributed to the pharmacological preconditioning mechanism16. Lledo-Garcia et al demonstrated a beneficial effect of sildenafil after renal ischemia. The aim of their experimental study was to determine the hemodynamic, biochemical, and histological effects of sildenafil as a preconditioning vasodilator before a period of warm ischemia17. A similar effect was demonstrated in our laboratory7. Tissue hypoperfusion can be present even in the normal blood pressure and adequate cardiac output, a state sometimes referred to as cryptic shock. This hypoperfusion may be related to preferential maldistribution of blood flow at the regional or microvascular level18,19. Derangements of small vessel perfusion are largely a function of intrinsic events in the microcirculation. The causes of microcirculatory flow alterations in sepsis are multifactorial and include endothelial cell dysfunction, increased leukocyte and platelet adhesion, fibrin deposition, erythrocyte stiffness, altered local perfusion pressures due to regional redistribution of blood flow, and functional shunting20,21. Although research on septic shock is 106 classically focused on macrocirculatory hemodynamics that reflect the distribution of blood flow globally throughout the body, a functioning microcirculation is another critical component of the cardiovascular system that is necessary for effective oxygen delivery to tissues. In the present study we used the pretreatment with sildenafil, a potent vasodilator, in rats with abdominal sepsis, with significant changing in leukocytes, cytokines and reactive C protein. Regardless of the cause, it seems that an early and aggressive hemodynamic intervention can impart the best opportunity to limit the damage caused by tissue hypoperfusion, including attenuating the inflammatory response and endothelial injury22. An ideal therapy to improve microcirculation would modulate endothelial function and vasodilate low-flow units. Pharmacotherapies such as vasodilators (prostacyclin) and mixed inotropes/vasodilators (dobutamine) have been used to this end and have demonstrated an increase in systemic oxygen consumption suggesting microcirculatory recruitment23. De Backer et al demonstrated increases in capillary perfusion independent of systemic hemodynamic effects with dobutamine and recombinant human activated protein C (rhAPC). These effects are likely to be due to the vasodilatory and rheologic action of dobutamine and perhaps to modulation of the leukocyte-endothelial cell interaction by rhAPC6,24. Seen through the lens of the microcirculation, sepsis-induced increases in nitric oxide (NO) may actually be an adaptive response that is an attempt to restore blood flow at the level of capillaries. Contrary to previous lines of investigation, exogenous NO may be viewed as an attractive therapeutic agent in sepsis if it is able to augment microcirculatory flow. NO fulfills the requirement of being a potent vasodilator and modulator of leukocyte-endothelial reactions, as seems to be the sildenafil used in the present experimental model25. Administration of exogenous vasodilator sildenafil, prior to the induction of sepsis, demonstrated important protection against inflammation. One obvious concern about the use of exogenous sildenafil in sepsis is the potential for exacerbation of arterial hypotension, which could attenuate its positive effect on the microcirculation. Studies about this are lacking. Therefore, at present, whether or not exogenous sildenafil administration to patients with sepsis is efficacious and safe is unknown and the subject of ongoing clinical investigation. We are sure that, as promising as targeting the microcirculation in sepsis may appear, the microcirculation 107 is only one of many pathophysiologic factors that contribute to the overall picture of circulatory failure and, ultimately, cellular dysfunction. In conclusion, the data of our study support the statement that pretreatment of abdominal sepsis with the vasodilator sildenafil influenced the favorable evolution of inflammation and immune response in rats. REFERENCES 1. Hotchkiss RS, Karl IE. The pathophysiology and treatment of sepsis. N Engl J Med. 2003;348:138–50. 2. Angus DC, Linde-Zwirble WT, Lidicker J, et al. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29:1303–10. 3. Fries M, Weil MH, Sun S, et al. Increases in tissue Pco2 during circulatory shock reflect selective decreases in capillary blood flow. Crit Care Med. 2006;34:446–52. 4. Centers for Disease Control and Prevention (CDC). Bloodstream infections among patients treated with intravenous epoprostenol or intravenous treprostinil for pulmonary arterial hypertension--seven sites, United States, 2003-2006. MMWR Morb Mortal Wkly Rep. 2007;56:170-2. 5. Zardi EM, Zardi DM, Dobrina A, Afeltra A. Prostacyclin in sepsis: a systematic review. Prostaglandins Other Lipid Mediat. 2007; 83(1-2):1-24. 6. De Backer D, Creteur J, Dubois MJ, et al. The effects of dobutamine on microcirculatory alterations in patients with septic shock are independent of its systemic effects. Crit Care Med. 2006;34:403–8. 7. Medeiros PJ, Villarim Neto A, Lima FP, Azevedo IM, Leão LR, Medeiros AC. Effect of sildenafil in renal ischemia/reperfusion injury in rats. Acta Cir Bras. 2010;25:490-5. 8. Clemmesen JO, Giraldi A,Ott P, Dalhoff K, Hansen BA, Larsen FS. Sildenafil does not influence hepatic venous pressure gradient in patients with cirrhosis. World J Gastroenterol. 2008;14: 6208-12. 9. Lin SM, Huang CD, Lin HC, et al. A modified goal-directed protocol improves clinical outcomes in intensive care unit patients with septic shock: a randomized controlled trial. Shock. 2006;26:551–7. 10. Jones AE, Brown MD, Trzeciak S, et al. The effect of a quantitative resuscitation strategy on mortality in patients with sepsis: a meta-analysis. Crit Care Med. 108 2008;36:2734–9. 11. Otero RM, Nguyen HB, Huang DT, et al. Early goal-directed therapy in severe sepsis and septic shock revisited: concepts, controversies, and contemporary findings. Chest. 2006;130:1579–95. 12. Cadirci E, Halici Z , Odabasoglu F , Albayrak A , Karakus E , Unal D , Atalay F, Ferah I andUnal B. Sildenafil treatment attenuates lung and kidney injury due to overproduction of oxidant activity in a rat model of sepsis: a biochemical and histopathological study. Clin Exp Immunol. 2011;166:374-84. 13. Damas P, Ledoux D, Nys M, Vrindts Y, De Groote D, Franchimont P, Lamy M. Cytokine serum level during severe sepsis in human IL-6 as a marker of severity. Ann Surg. 1992; 215:356-62. 14. Steinhauser ML, Hogaboam CM, Kunkel SL, Lukacs NW, Strieter RM, Standiford TJ. IL-10 is a major mediator of sepsis-induced impairment in lung antibacterial host defense. J Immunol. 1999;162:392-9. 15. Terada LS, Hybertson BM, Connelly KG, et al. XO increases neutrophil adherence to endothelial cells by a dual ICAM-1 and P-selectin-mediated mechanism. J Appl Physiol. 1997;82:866–73. 16. Kukreja, R.C., Salloum, F., Das, A., Ockaili, R., Yin, C., Bremer, Y.A., Fisher, P.W., Wittkamp, M., Hawkins, J.,Chou, E., Kukreja, A.K., Wang, X., Marwaha, V.R., XI, L., Pharmacological preconditioning with sildenafil: basic mechanisms and clinical implications. Vasc Pharmacol. 2005;42: 219–32. 17. Lledo-Garcia E. Rodriguez-Martinez R, Cabello-Benavente I, Moncada-Iribarren A, Tejedor-Jorge E, Dulin C, Hernandez-Fernandez JF, Del Canizo-Lopez. Sildenafil Improves Immediate Posttransplant Parameters in Warm-Ischemic Kidney Transplants: Experimental Study. Transpl Proc. 2007; 39: 1354–6. 18. De Backer D, Creteur J, Preiser JC, et al. Microvascular blood flow is altered in patients with sepsis. Am J Respir Crit Care Med. 2002;166:98–104. 19. Sakr Y, Dubois MJ, De Backer D, et al. Persistent microcirculatory alterations are associated with organ failure and death in patients with septic shock. Crit Care Med. 2004;32:1825–31. 20. Spronk PE, Zandstra DF, Ince C. Bench-to-bedside review: sepsis is a disease of the microcirculation. Crit Care. 2004;8:462–8. 21. Bateman RM, Sharpe MD, Ellis CG. Bench-to-bedside review: microvascular dysfunction in sepsis–hemodynamics, oxygen transport, and nitric oxide. Crit Care. 109 2003;7:359–73. 22. Rivers E, Nguyen B, Havstad S, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345:1368–77. 23. Bihari D, Smithies M, Gimson A, et al. The effects of vasodilation with prostacyclin on oxygen delivery and uptake in critically ill patients. N Engl J Med. 1987;317:397–403. 24. De Backer D, Verdant C, Chierego M, et al. Effects of drotrecogin alfa activated on microcirculatory alterations in patients with severe sepsis. Crit Care Med. 2006;34:1918–24. 25. Gundersen Y, Corso CO, Leiderer R, et al. The nitric oxide donor sodium nitroprusside protects against hepatic microcirculatory endotoxaemia. Intensive Care Med. 1998;24:1257–63. dysfunction in early 110 6. COMENTÁRIOS, CRÍTICAS E SUGESTÕES O câncer colorretal é o terceiro tipo de neoplasia maligna mais frequente no mundo44,46,65-69 e as metástases hepáticas estão presentes em 15% a 25% dos pacientes no momento do diagnóstico44,46,65,70-73. Cerca de 50% dos pacientes desenvolverão metástases hepáticas na evolução da doença53,67-69,73-77 estas são responsáveis por, no mínimo, dois terços das mortes68,72,74,78. O tratamento cirúrgico das metástases hepáticas em pacientes com câncer colorretal já é bem estabelecido na literatura como o que proporciona a maior chance potencial de cura dos pacientes, apesar de todas as outras modalidades terapêuticas44,51,68,72,77-83 como embolização vascular, radioterapia, ablação por radiofrequência, quimioterapia81,84. Porém, apenas 10-25% dos pacientes com metástases hepáticas receberão indicação de cirurgia para ressecção44,46,70,72,76,78-80,83. Esta consiste na capacidade de remover todas as metástases hepáticas com margens livres e de preservar um fígado remanescente futuro de no mínimo 20-30% do volume total em pacientes com fígado saudável67. Na ausência de doença extra-hepática irressecável, este remanescente deve ainda proporcionar fluxo arterial e portal adequados, bem como drenagem biliar e retorno venoso78. Não há diferença importante na morbi-mortalidade perioperatória entre as ressecções simultâneas e em dois tempos, porém há o benefício de uma duração da cirurgia menor e de internação pós-operatória mais curta no grupo operado simultaneamente, bem como menor perda de sangue durante a cirurgia44. Quando um paciente é submetido apenas a cirurgia, a sobrevivência após esta é estimada em várias séries entre 20-58% em 5 anos e 20% aos 10 anos44,49,54,66-70,73,74,76,78,8183,86,87 . A recorrência tem o fígado como o local mais comumente acometido49,79,88. O objetivo desde trabalho foi identificar se há alteração na biodistribuição do radiofármaco fitato-99mtecnécio, usado para realização de cintilografias, bem como avaliar a marcação e morfometria das hemácias, de roedores submetidos a um procedimento cirúrgico de grande porte. Elegemos como representante deste grupo a colectomia associada à hepatectomia pela importância do tratamento e por se tratar de um procedimento que vem crescendo em indicações nos pacientes que possuem CCR com metástase hepática, pelos motivos explicados acima. Este procedimento revolucionou o tratamento do câncer colorretal nas últimas décadas, como descrito previamente, devolvendo em alguns casos a chance de cura aos 111 pacientes com doença avançada. Não foi objetivo deste estudo a carcinogênese do câncer colorretal, logo esta não foi induzida nos animais. Apesar do grande trauma cirúrgico a que estes animais do grupo colectomia+hepatectomia foram submetidos, eles evoluíram bem até o trigéssimo dia do experimento. Na primeira semana este grupo apresentou uma perda de peso importante quando comparado aos outros dois grupos, porém tal perda foi recuperada satisfatoriamente nas três semanas subsequentes. Estes achados colaboram com o fato de que a hepatectomia aumenta a morbidade neste grupo e a regeneração hepática deve compensar as perdas. Ao final deste experimento, quando as amostras obtidas foram analisadas, observou-se que existiam diferenças importantes em alguns parâmetros quando os três grupos foram comparados, como na captação do fitato-pertecnetato pelo fígado do grupo colectomia+hepatectomia que foi significativamente menor que a do grupo sham, porém quando o grupo colectomia+hepatectomia foi comparado ao grupo colectomia não foram observadas divergências. Tal fato pode ser explicado pela hipótese que ao final de 30 dias ocorreu regeneração hepática suficiente para corrigir qualquer disfunção, normalizando a captação do radiofármaco. A literatura refere que a regeneração hepática no rato ocorre muito rapidamente, completandose em aproximadamente uma semana89,90. A biodistribuição do radiofármaco pelo fígado guarda relação com a intensidade da doença que o acomete, com a fibrose, o prognóstico e a função hepática22,90-93. Desse modo, a captação do fitato-pertecnetato pelo fígado é um índice indireto e prático da função hepática23,94-96. Os nossos estudos em laboratório, que seguem esta linha de pesquisa, conseguiram demonstrar que quando a cirurgia realizada é a esplenectomia13 a distribuição do radiofármaco no fígado é maior que nos grupos controles, sugerindo que o procedimento cirúrgico favorece a captação. Este aumento da captação deve resultar da melhora da função hepática, que no estudo foi confirmada pelos melhores níveis de enzimas hepáticas nos ratos esplenectomizados do que nos controles. No presente estudo, a menor absorção de fitato-pertecnetato pelo fígado coincidiu com aumento das enzimas hepáticas (ALT,AST,FA) em ratos colectomia + hepatectomia parcial quando comparados aos ratos sham. Várias patologias são estudadas através de procedimentos de medicina nuclear, que cada vez mais se tornam mais eficazes21 e menos invasivos23,97,98. 112 Além de doenças, outras condições também podem alterar a biodistribuição do pertecnetato ou fixação dos constituintes sanguíneos como: cirurgias, medicações, produtos naturais1-5,11. A alteração da marcação de constituintes sanguíneos no geral é resultado da ação de medicamentos e trauma (cirurgias) devido à: (1) mudança da estrutura da membrana celular ou modificação nos sistemas de transporte de íons de pertecnetato em células, (2) oxidação direta ou geração de radicais livres, (3) inibição direta (ação quelante) dos íons pertecnetato, ou (4) ligação nos mesmos locais nos elementos do sangue27. O estudo em questão observou que a marcação das hemácias com pertecnetato no grupo colectomia+hepatectomia foi menor do que em ratos sham. Tal fato é importante devido à marcação de hemácias ser um procedimento utilizado no diagnóstico de sangramentos digestivos e renais39,41. Os dados obtidos nesta pesquisa podem ser explicados, em parte, através de interações de alguns fatores que resultam da ressecção hepática com os sistemas de transporte de íons pertecnetato, o que culmina com a diminuição da marcação das hemácias pelo pertecnetato. Ao ingressar no Programa de Pós-graduação em Ciências da Saúde da UFRN evidenciei que as diversas disciplinas em carácter multiprofissional contribuíram para diversificar meus conhecimento antes só restritos à área da medicina, pois neste tive contato com alunos e professores de diversas áreas da saúde. Através das disciplinas obrigatórias e complementares, aprendi sobre como tornar a escrita da minha dissertação mais simples, o passo-a-passo da metodologia minimizando os riscos de erros, sobre como pesquisar artigos e avaliar a sua relevância, e pude ter também contato com conceitos avançados em estatística. Ao longo dessa jornada aperfeiçoei a técnica da elaboração de artigos através dos meus artigos publicados, participei de eventos científicos que enriqueceram meus conhecimentos e fizeram com que eu pudesse ter contato com outros pesquisadores. Cada uma dessas etapas foi importante no meu crescimento na pesquisa e ampliou minha visão crítica na prática da minha área de atuação. O conhecimento adquirido neste Mestrado contribuiu para o desenvolvimento de modelos experimentais em outras pesquisas, bem como avançar nesse mesmo modelo, para a verificação de outros resultados. Uma constante no delineamento e execução deste projeto foi a preocupação exaustiva de evitar riscos, buscando seguir rigorosamente as condições metodológicas, para permitir a reprodutibilidade integral de nossos estudos pela comunidade científica objetivando estimular a 113 obtenção de outros resultados que tragam maiores contribuições ao meio acadêmico. Para isso procuramos descrever a metodologia de forma simples e clara, para que todos os pesquisadores possam reproduzir e desenvolver novos modelos experimentais que contribuam com a consolidação de novos conhecimentos nesta área. Durante o desenvolvimento dessa pesquisa pude compreender a importância da pesquisa básica, no sentido de criar subsídios para que a prática clínica na Medicina Nuclear evolua, contribuindo para uma melhor compreensão dos efeitos das intervenções cirúrgicas na funções dos órgãos operados e de outros órgãos à distância que não sofreram intervenções. Tal entendimento sobre esse tema em particular minimizaria erros e interpretações equivocadas de exames que podem prejudicar o diagnóstico e prognóstico de um paciente. Dessa forma estaríamos auxiliando os profissionais da área de Medicina Nuclear com novos conhecimentos, até agora não amplamente elucidados no que diz respeito aos efeitos da colectomia e hepatectomia. A inspiração para realizar este estudo surgiu em primeiro lugar, do contato com meu orientador, cuja linha de pesquisa especulava a influência de cirurgias e outros fatores como medicamentos, plantas medicinais, entre outros nos exames de medicina nuclear. O mesmo já tinha estudado as consequências da colectomia total nesta área da radiologia. A pergunta a ser respondida dizia respeito aos efeitos dessa intervenção cirúrgica associada à hepatectomia parcial, aumentando o porte cirúrgico, na biodistribuição do fitato-99mTcO4, na marcação e morfologia de hemácias e em parâmetros metabólicos. Entretanto repercussões da colectomia associada à hepatectomia têm sido pouco estudadas, como foi constatado em prévio levantamento bibliográfico amplo realizado no início do projeto. Outro aspecto que motivou a realização deste trabalho foi a possibilidade de utilizar os recursos da Medicina Nuclear, em estudos dessa natureza. Houve grande facilidade de manipulação e emprego do radiofármaco, bem como compreensão da sua utilidade para elucidar as alterações na captação da atividade radioativa pelo órgão alvo da pesquisa. Após concluído este trabalho, é continuo o desejo de prosseguir com os estudos nesta área de atuação, desenvolvendo um doutorado nesta mesma base de pesquisa, estudando algo que não foi contemplado neste estudo como os efeitos da colectomia na regeneração hepática, parâmetro de suma importância na cirurgia do 114 fígado. Para prosseguir nesta carreira tenho o total empenho e suporte do meu orientador que é chefe do Núcleo de Cirurgia Experimental, e que já evidenciou ter disponibilidade de continuar minha orientação nesta trajetória. Durante todo tempo em que estive envolvida com essa dissertação trabalhei também, concomitantemente, como professora substituta da Disciplina de Técnica Operatória que faz parte da grade do Curso de Medicina, da qual meu orientador é Professor Titular com dedicação exclusiva. Além disso pude participar de eventos científicos onde meus artigos escritos ao longo deste Mestrado puderam ser apresentados à comunidade científica. Outro aspecto importante foi poder participar como orientadora de Trabalhos de Conclusão de Curso dos alunos da graduação de Medicina. De grande relevância para confecção deste estudo foi o suporte dado pelo Setor de Medicina Nuclear da Liga Norteriograndense Contra o Câncer fornecendo os radiofármacos, e pelo serviço de patologia do Hospital Universitário Onofre Lopes (HUOL)-Universidade Federal do Rio Grande do Norte (UFRN). Além destes, destaca-se a estrutura do Núcleo de Cirurgia Experimental da UFRN, o laboratório onde toda esta pesquisa foi idealizada e executada, e dos funcionários que trabalham neste núcleo de pesquisa. Estes apoios foram fundamentais para a realização dessa dissertação. Sem a participação efetiva de todas essas instituições e seus respectivos serviços e funcionários, não teria sido possível concluir esta dissertação. Os diferentes serviços que contribuíram para realização desta dissertação comprovam o seu carácter multidisciplinar. O rato Wistar foi escolhido como modelo experimental para o estudo, por ser de fácil aquisição, manutenção e manipulação no laboratório. Além disso, trata-se de um modelo animal previamente testado em um número considerável de estudos na área de cirurgia experimental, que suporta muito bem atos anestésicos e procedimentos operatórios como o realizado neste estudo e guarda boa correlação com os objetivos do estudo, realizado de forma segura e satisfatória. Os resultados obtidos neste estudo sugerem que a colectomia associada à hepatectomia alterou a captação do fitato-pertecnetato no fígado e hemácias de ratos, e a atividade enzimática hepática. O estudo mostrou-se relevante, pois além de contribuir sobremaneira para minha formação, ainda elucidou dados até então pouco explorados na literatura 115 Através deste estudo acreditamos haver contribuído para que futuros trabalhos nesta área disponham de parâmetros sobre os efeitos da colectomia e hepatectomia sobre a biodistribuição de radiofármacos. Deseja-se também que as informações levantadas por esta pesquisa sirvam de ponto de partida para novos estudos sobre a avaliação das consequências da colectomia associada à hepatectomia, com potencial para implicações clínicas para pacientes que venham a ser submetidos a esta intervenção cirúrgica e venham a realizar exames de medicina nuclear. Finalmente, esta pesquisa experimental me proporcionou um grande enriquecimento intelectual, me introduziu nesta fascinante área da investigação científica e abriu horizontes para a aplicabilidade clínica de conhecimentos de radiofarmácia adquiridos em laboratório. 116 7. REFERÊNCIAS 1. Paoli S, Giani TS, Presta GA, Pereira MO, Fonseca AS, Brandão-Neto J, Medeiros AC, Santos-Filho SD, Bernardo-Filho M. Efeitos de cravo (L. cravo) relativos à rotulagem dos constituintes sanguíneos com tecnécio-99m e na morfologia das células vermelhas do sangue. Braz Arch Biol Technol. 2007;50:175-82. 2. Rebello BM, Moreno SRF, Ribeiro CG, Neves RF, Fonseca AS, Caldas LQA, Bernardo-Filho M, Medeiros AC. Effect of a peel passion fruit flour (Passiflora edulis f. flavicarpa) extract on the labeling of blood constituents with technetium99m and on the morphology of red blood cells. Braz Arch Biol Technol. 2007;50:153-59. 3. Rêgo ACM, Ramalho RAO, Egito EST, Araújo-Filho I, Azevedo IM, Palestro CJ, Medeiros AC. Biodistribution of technetium-99m pertechnetate after total colectomy in rats. Appl Radiat Isot. 2010;68:2169-73. 4. Rêgo ACM, Araújo-Filho I, Azevedo IM, Jácome DT, Ramalho RAO, Medeiros AC. Biodistribution of technetium-99m pertechnetate after Roux-en-Y gastric bypass (Capella technique) in rats. Acta Cir Bras. 2010;25:9-12. 5. Rêgo ACM, Villarim-Neto A, Azevedo IM, Araújo-Filho I, Egito EST, Medeiros AC. Biodistribution of technetium-99m pertechnetate after total gastrectomy and Roux-en-Y jejunal pouch. J Invest Surg. 2010;23:94-100. 6. Medeiros AC, Rêgo AM, Azevedo IM, Carvalho MDF, Medeiros VB, Araújo-Filho I. Metabolism and gastric remnant changes after Roux-en-Y gastric bypass in rats. J Invest Surg. 2011;24:109-14. 7. Bernardo-Filho M, Santos-Filho SD, Moura EG, Maiworm AI, Orlando MMC, Penas ME, Cardoso VN, Bernardo LC, Brito LC. Drug Interaction with Radiopharmaceuticals: a Review. Braz Arch Biol Technol. 2005;48:13-27. 8. Villarim-Neto A, Açucena MKMT, Pereira KRSG, Rêgo ACM, Azevedo IM, Bernardo-Filho M, Medeiros AC. Biodistribution of samarium-153-EDTMP in rats treated with docetaxel. Acta Cir Bras. 2009;24:62-6. 9. Fonseca AS, Frydman JN, Rocha VC, Bernardo-Filho M. Acetylsalicylic acid decreases the labeling of blood constituents with technetium-99m. Acta Biol Hung. 2007;2:187-98. 10. Spicer JA, Hladik WB, Mulberry WE. The effects of selected antineoplastic agents 117 on the labeling of erythrocytes with technetium-99m using the UltraTag RBC kit. J Nucl Med Technol. 1999;27:132-35. 11. Chacon DA, Araújo-Filho I, Villarim-Neto A, Rêgo ACM, Azevedo IM, BernardoFilho M, Brandão-Neto J, Medeiros AC. Biodistribution of the radiophamarceutical sodium pertechnetate (Na99mTcO) after massive small bowel resection in rats. Acta Cir Bras. 2007;22:430-5. 12. Medeiros AC, Araújo-Filho I, Medeiros VB, Pinheiro LA, Freire FH, Azevedo IM, Brandão-Neto. Comparing reconstruction with ileocecal graft to jejunal interposition pouch after total gastrectomy in rats. J Invest Surg. 2007;20:41-8. 13. Pereira KRSG, Açucena MKMT, Villarim-Neto A, Rêgo ACM, Bernardo-Filho M, Azevedo IM, Araújo-Filho I, Medeiros AC. Biodistribution of the radiopharmaceutical technetium-99m-sodium phytate in rats after splenectomy. Braz Arch Biol Technol. 2008;51:203-07. 14. Pereira JM. Clinical uses of radiopharnaceuticals. Rev OFIL. 2003;13:27-31. 15. Azevedo IM, Fernandes DP, Costa TC, Araújo-Filho I, Rêgo ACM, Medeiros VB, Carvalho MDF, Medeiros AC. Diabetes and biodistribution of pertechnetate (Na99mTcO4) in rats. J Surg Cl Res. 2010;1:13-21. 16. Rebello BM, Moreno SRF, Godinho CR, Neves RF, Fonseca AS, Bernardo-Filho M, Medeiros AC. Effects of Passiflora edulis flavicarpa on the radiolabeling of blood constituents, morphology of red blood cells and on the biodistribution of sodium pertechnetate in rats. Appl Radiat Isot. 2008;66:1788–92. 17. Zink SI, Ohki SK, Stein B, Zambuto DA, Rosenberg RJ, Choi JJ, Tubbs DS. Noninvasive Evaluation of active lower gastrointestinal bleeding: comparison between contrast-enhanced MDCT and 99m Tc-labeled RBC scintigraphy. AJR. 2008;191:1107-14. 18. Schneider A, Attaran M, Gratz KF, Bleck JS, Winkler M, Manns MP, Ott M. Intraportal infusion of 99m technetium-macro-aggregrated albumin particles and hepatocytes in rabbits: assessment of shunting and portal hemodyn changes. Transplantation. 2003;75:296-302. 19. Hunt AP, Frier M, Johnson RA, Berezenko S, Perkins AC. Preparation of Tc-99mmacroaggregated albumin from recombinant human albumin for lung perfusion imaging. Eur J Pharm Biopharm. 2006;6:26–31. 20. Wilson AJW. Functional renal imaging with nuclear medicine. Abdom Imaging. 2003;28:176-9. 118 21. Lodge MA, Braess H, Mahmoud F, Suh J, Englar N, Geyser-Stoops S, Jenkins J, Bacharach SL, Dilsizian V. Developments in nuclear cardiology: transition tomography-computer tomography. J Invasive Cardiol. 2005;17:491-6. 22. Hoefs JC, Wang F, Kanel G. Functional measurement of nonfibrotic hepatic mass in cirrhotic patients. Am J Gastroenterol.1997;92:2054-8. 23. Kikuchi M, Tomita K, Nakahara T, Kitamura N, Teratani T, Irie R, Yokoyama H, Suzuki T, Yokoyama T, Taguchi T, Tanaka S, Noguchi M, Ohkura T, Hibi T. Utility of quantitative 99mTc-phytate scintigraphy to diagnose early-stage non-alcoholic steatohepatitis. Scand J Gastroenterol. 2009;44:229-36. 24. Saha GB. Fundamentals of nuclear pharmacy. 6nd ed. New York: Springer; 2010. 25. Açucena MKMT, Pereira KRSG, Villarim-Neto A, Rêgo ACM, Bernardo-Filho M, Azevedo IM, Araújo-Filho I, Medeiros AC. Influence of the esplenectomy in the biodistribution of technetium-99m dimercaptosuccinic acid (99mTc-DMSA) in rats. Braz Arch Biol Technol. 2008;51:197-202. 26. Technetium-99m radiopharmaceuticals: status and trends. Vienna: International Atomic Energy Agency; 2009. 27. Arano Yasushi. Recent advances in 99m Tc radiopharmaceuticals. Ann Nucl Med. 2002;16:79-93. 28. Almeida EV, Monteiro EG, Alves EV, Silva NG, Fukumori NTO, Barboza MF, Mengatti J, Matsuda MMN, Vasconcellos MBA. Controle de qualidade de EC99m Tc: determinação de pureza radioquímica e investigação da influência de impurezas na biodistribuição. Rev Bras Fis Med. 2010;4:71-4. 29. Holanda CMCX, Oliveira EH, Rocha LG, Barbosa VSA, Spydes MHC, Aragão CFS, Medeiros AC. Effect of paclitaxel (Taxol®) on the biodistribution of sodium pertechnetate (Na99mTcO4) in female wistar rats. Braz Arch Biol Technol. 2008;51:191-6. 30. Alencar SSS, Medeiros AC, Brandt CT, Aguiar JLA, Rocha KBF, Silva MP. Translocação de bactérias marcadas com Tc99m na icterícia obstrutiva em ratos. Acta Cir Bras. 2001;17:35-8. 31. Baert AL, Sartor K, et al. Diagnostic nuclear medicine. 2th ed. Berlim: Springer; 2006. 32. Araújo-Filho I, Rêgo ACM, Brandão-Neto J, Villarim-Neto A, Medeiros AC, Egito EST, Azevedo IM. Biodistribution of the radiopharmaceutical sodium pertechnetate after biliopancreatic bypass with a duodenal switch. Braz Arch Biol 119 Technol. 2007;50:189-97. 33. Abreu PR, Almeida MC, Bernardo RM, Bernardo LC, Brito, LC, Garcia, EA, Fonseca AS, and Bernardo-Filho M. Guava extract (Psidium guajava) alters the labelling of blood constituents with technetium-99m. J Zhejiang Univ Sci B. 2007;7:429-35. 34. Meyer PF, Santos-Filho SD, Ronzio OA, Bonelli L, Fonseca AS, Costa ICC, Brandão-Neto J, Bernardo-Filho Mário, Medeiros AC. Consequences of the magnetic field, sonic and radiofrequency waves and intense pulsed light on the labeling of blood constituents with technetium-99m. Braz Arch Biol Technol. 2007;50:117-22. 35. Fundamentos físicos das imagens cintilográficas.[Acesso em 02 set 2012]. Disponível em: http://www.medicinanuclear-santamaria.com.br/fundamentos.html 36. Nuclear medicine resources manual. Vienna: International Atomic Energy Agency, 2006. 37. Almeida EV, Silva NG, Freire AC, Monteiro EG, Benedetti S, Muramoto E, Fukumori NTO, Matsuda MMN, Vasconcellos MBA. Método cintilográfico não invasivo para estudo de biodistribuição de radiofármacos. Rev Bras Fis Med. 2011;4:53-6. 38. Marcuzzo M. Quantificação de impressões diagnósticas em imagens de cintilografia renal. Porto Alegre. Dissertação. [Mestrado em Ciências da Computação]-Universidade Federal do Rio Grande do Sul; 2007. 39. Howarth DM. The role of nuclear medicine in the detection of acute gastrointestinal bleeding. Semin Nucl Med. 2006;36:133-46. 40. Zink SI, Ohki SK, Stein B, Zambuto DA, Rosenberg RJ, Choi JJ. Noninvasive evaluation of active lower gastrointestinal bleeding: comparison between contrastenhanced MDCT and 99mTc-labeled RBC scintigraphy. AJR. 2008;191:1107–14. 41. Morita S, Ohzono H, Ishibashi M, Hirayama T, Nomura Y, Yoshii T, Takahashi K, Ohtake H, Araki T, Sakamoto T, et al. Diagnosis of acute gastrointestinal bleeding using scintigraphy with 99mTc-labeled red blood cells. Kaku Igaku.1990;27:45966. 42. Schoen RE, Pinsky PF, Weissfeld JL, Yokochi LA, Church T, Laiyemo AO, Bresalier R, Andriole GL, Buys SS, Crawford ED, Fouad MN, Isaacs C, Johnson CC, Reding DJ et al. Colorectal cancer incidence and mortality with screening flexible sigmoidoscopy. N Eng J Med. 2012;366:2345-57. 120 43. Garden OJ, Rees M, Poston GJ, Mirza D, Saunders M, Ledermann J, Primrose JN, Parks W. Guidelines for resection of colorectal cancer liver metastases. Gut. 2006;55(Suppl III):1–8. 44. Jong M, van Vledder M, Ribero D, Hubert C, Gigot J, Choti MA, Schulick RD, Capussott L, Dejong CH, Pawlik TM. Therapeutic efficacy of combined intraoperative ablation and resection for colorectal liver metastases: an international, multi-institutional analysis. J Gastrointest Surg. 2011;15:336–44. 45. Martin R, Paty P, Fong Y, Grace A, Cohen A, DeMatteo R, Jarnagin W, Blumgart L. Simultaneous liver and colorectal resections are safe for synchronous colorectal liver metastasis. J Am Coll Surg. 2003;197:233–42. 46. Poston GJ, Adam R, Alberts S, Curley S, Figueras J, Haller D et al. OncoSurge: A strategy for improving resectability with curative intent in metastatic colorectal cancer. 2005;28: 7125-34. 47. Pawlik TM, Schulick RD, Choti MA. Expanding criteria for resectability of colorectal liver metastases. The Oncologist. 2008;13:51–64. 48. Brasil. Ministério da Saúde. Instituto Nacional do Câncer. Estatística do Câncer. Câncer no Brasil: Dados dos registros de base populacional. Rio de janeiro. 2010. [Acesso em 11 Nov 2012]. Disponível em: http://www.inca.gov.br/regpop/2003/index.asp?link=conteudo_view.asp&ID=11 49. Abbas S, Lam V, Hollands M. Ten-year survival after liver resection for colorectal metastases: systematic review and meta-analysis. ISRN Oncol. 2011. 50. Guillou PJ, Quirke P, Thorpe H, Walker J, Jayne DG, Smith AMH, Health RM, Brown JM. Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet. 2005;365:1718-26. 51. Adam R, Delvart V, Pascal G, Valeanu A, Castaing D, Azoulay D, Giacchetti S, Paule B, Kunstlinger F, Ghe’mard O, Levi F, Bismuth H, Hon FACS. Rescue surgery for unresectable colorectal liver metastases downstaged by chemotherapy. A model to predict long-term survival. Ann Surg. 2004;240:644-58. 52. Lupinacci R, Penna C, Nordlinger B. Hepatectomy for resectable colorectal cancer metastases-indicators of prognosis, definition of resectability, techniques and outcomes. Surg Oncol Clin N Am. 2007;16:493–506. 53. Wu Y, Li B, Wang T, Wang S, Zhou Y. Radiofrequency ablation vs hepatic resection for solitary colorectal liver metastasis: a meta-analysis. World J 121 Gastroenterol. 2011;17: 4143-48. 54. Lochan R, White SA Manas DM. Liver resection for colorectal liver metastasis. Surg Oncol. 2007;16:33–45. 55. Cai GX, Cai SJ. Multi-modality treatment of colorectal liver metastases. World J Gastroenterol. 2012;18:16-24. 56. Carvalho MDF, Araújo-Filho I, Rêgo ACM, Azevedo IM, Medeiros AC. Hepatectomy for benign and malign diseases in University Hospital. J Surg Cl Res. 2011;2:42-50. 57. Abdalla EK, Vauthey JN, Ellis LM, Ellis V, Pollock R, Broglio KR, Hess K, Curley SA. Recurrence and outcomes following hepatic resection, radiofrequency ablation, and combined resection/ablation for colorectal liver metastases. Ann Surg. 2004;239:818–27. 58. Fahy BN, Fischer CP. Synchronous resection of colorectal primary and hepatic metastasis. J Gastrointest Oncol. 2012;3:48-58. 59. Lee WS, Yun SH, Chun HK, Lee WY, Kim SJ, Choi SH, Heo JS, Joh JW, Choi D, Kim SH, Rhim H, Lim HK. Clinical outcomes of hepatic resection and radiofrequency ablation in patients with solitary colorectal liver metastasis. J Clin Gastroenterol. 2008; 42:945-9. 60. Kelbaek H. Technetium-99m labeling of red blood cells: in vitro evaluation of a new approach. J Nucl Med. 1986; 27:1770-73. 61. Braga AC, Oliveira MB, Feliciano GD, Reiniger IW, Oliveira JF, Silva CR, Bernardo-Filho M. The effect of drugs on the labeling of blood elements with technetium-99m. Curr Pharm Des. 2000;6:1179-91. 62. Rocha GS, Pereira MO, Benarroz MO, Frydman JNG, Rocha VC, Pereira MJ, Fonseca AS, Medeiros AC, Bernardo-Filho M. Sucralose sweetener in vivo effects on blood constituents radiolabeling, red blood cell morphology and radiopharmaceutical biodistribution in rat. Appl Radiat and Isot. 2011;69:46–51. 63. Callahan RJ, Rabito, CA. Radiolabeling of erythrocytes with technetium-99m: role of band-3 protein in the transport of pertechnetate across the cell membrane. J Nucl Med. 1990;31:2004-08. 64. Berezina TL, Zaets SB, Machiedo GW. Alterations of red blood cell shape in patients with severe trauma. J trauma. 2004;57:82-7. 65. Morris EJA, Forman D, Thomas JD, Quirke TP, Taylor EF, Fairley L, Cottier IB, Poston G. Surgical management and outcomes of colorectal cancer liver 122 metastases. BJS. 2010;97:1110–18. 66. Robertson DJ, Stukel TA, Gottlieb DJ, Sutherland JM, Fisher ES. Survival After Hepatic Resection of Colorectal Cancer Metastases. A National Experience. Cancer. 2009;752-59. 67. Biasco G, Derenzini E, Di Batista M, Brandi G. The Treatment of Liver Metastases from Colorectal Cancer: Questions More than Answers? Govaresh. 2003;9:132-41. 68. Van den Eynde M, Hendlisz A. Treatment of Colorectal Liver Metastases: A Review. Rev Recent Clin Trials. 2009;4:56-62. 69. Biasco G, Derenzini E, Grazi GL, Ercolani G, Ravaioli M,Pantaleo MA, Brandi G. Treatment of hepatic metastases from colorectal cancer: Many doubts, some certainties. Cancer Treat Rev. 2006;32:214–28. 70. Khatri VP, Petrelli NJ, Belghiti J. Extending the Frontiers of Surgical Therapy for Hepatic Colorectal Metastases: Is There a Limit? J Clin Oncol. 2005;23:8490-99. 71. Fong Y, Blumgart LH, Cohen AM. Surgical Treatment of colorectal metastases to the liver. CA Cancer J Clin. 1995;45:50-62. 72. Vahrmeijer AL, van Dierendonck JH, van de Velde CJH. Treatment of Colorectal Cancer Metastases Confined to the Liver. Eur J Cancer. 1995;31:1238-42. 73. Ismaili N. Treatment of colorectal liver metastases. World J Surg Onc. 2011;9:154. 74. Chedid AD, Villwock MM, Chedid MF, Rohde L. Prognostic factors following liver resection for hepatic metastases from colorectal cancer. Arq Gastroenterol 2003;40:159-65. 75. Mohammad, Balaa FK. Surgical Management of Colorectal Liver Metastases. Clin Colon Rectal Surg. 2009;22:225-32. 76. Yoon SS, Tanabe KK. Surgical Treatment and Other Regional Treatments for Colorectal Cancer Liver Metastases. Oncologist. 1999;4:197-208. 77. Tsoulfas G, Pramateftakis MG, Kanellos I. Surgical treatment of hepatic metastases from colorectal cancer. World J Gastrointest Oncol. 2011;3:1-9. 78. Coimbra FJF, Pires TC, Costa Junior WL, Diniz AL, Ribeiro HSC. Avanços no tratamento cirúrgico das metástases hepáticas colorretais. Rev Assoc Med Bras. 2011;57:220-27. 79. Alberts SR et al. Alternating Systemic and Hepatic Artery Infusion Therapy for Resected Liver Metastases From Colorectal Cancer: A North Central Cancer 123 Treatment Group (NCCTG)/ National Surgical Adjuvant Breast and Bowel Project (NSABP) Phase II Intergroup Trial, N9945/CI-66. J Clin Oncol. 2010;28:853-58. 80. Jaek D, Oussoultzoglou E, Rosso E. Hepatectomy for Colorectal Metastases in the Presence of Extrahepatic Disease. Surg Oncol Clin N Am. 2007;16:507–23. 81. Venook AP, Curley SA. Management of potentially resectable colorectal cancer liver metastases. Acesso em [02 Maio 2012]. Disponível em: http://www.uptodate.com/contents/management-of-potentially-resectablecolorectal-cancer-liver-metastases 82. Penna C, Nordlinger B.. Surgery of liver metastases from colorectal cancer: new promises. Br Med Bull. 2002;64:127–40. 83. Choti et al. Trends in Long-Term Survival Following Liver Resection for Hepatic Colorectal Metastases. Ann. Surg. 2002.235:759–66. 84. Perini MV, Coelho FF, Makdissi FF, Lupinacci RM, Machado MA, Herman P. Estratégias para aumentar a ressecabilidade em pacientes com metástases hepáticas de tumores colorretais. ABCD Arq Bras Cir Dig. 2011;24:324-27. 85. Primrose JM. Surgery for colorectal liver metastases. Brit J Cancer.2010;102:11318. 86. Ballantynes GH, Quin J. Surgical treatment of liver metastases in patient of colorectal cancer. Cancer. 1993;71:4252-66. 87. Nordlinger B, Vaillant JB, Guiguet M, Balladur P, Paris F, Bachellier P, Jaeck D. Survival Benefit of Repeat Liver Resections for Recurrent Colorectal Metastases: 143 Cases. J Clin Oncol. 1993;12:1491-6., 88. Petrowsky H, Gonen M, Jarnagin W, Lorenz M, MD, DeMatteo R, Heinrich S et al. Second Liver Resections Are Safe and Effective Treatment for Recurrent Hepatic Metastases from Colorectal Cancer. Ann Surg. 2002;235:863–71. 89. Ramalho FS, Ramalho LNZ, Zucoloto S, Castro e Silva Jr O. Regeneração hepatica: algumas definições num universe de incertezas. Acta Cir Bras.1993;8:177-89. 90. Aguiar LFR, Nassif PAN, Ribas CAPM, Nascimento MM, Wiederker JC, Pachnicki JPA, Stieven-Filho E. Regeneração do fígado de ratos após oclusão parcial da drenagem venosa hepatica. ABCD Arq Bras Cir Dig. 2009;22:89-95. 91. Groshar D, Slobodin G, Zuckerman E. Quantitation of Liver and Spleen Uptake of 99mTc-Phytate Colloid Using SPECT: Detection of Liver Cirrhosis. J Nucl Med. 2002;43:312–17. 124 92. Drum DE. Optimizing the Clinical Value of Hepatic Scintiphotography. Semin Nucl Med. 1978;8:346-57..D? 93. Hoefs J, Chang K, Wang F, Kanel G, Morgan T, Braunstein P. Perfused Kupffer cell mass. Correlation with histology and severity of chronic liver disease. Dig Dis Sci. 1995;40:552-60. 94. Hoefs JC, Wang F, Kanel G, Braunstein P. The liver-spleen scan as a quantitative liver function test: Correlation with liver severity at peritoneoscopy. Hepatology. 1995;22:1113-21. 95. Duman DG, Dede F, Akin H, Sen F, Turoğlu HT, Celikel C, Tözün N. Colloid scintigraphy in non-alcoholic steatohepatitis: a conventional diagnostic method for an emerging disease. Nucl Med Commun. 2006;27:387-93. 96. Veteläinen RL, Bennink RJ, Bruin K, van Vliet A, van Gulik TM. Hepatobiliary function assessed by 99mTc-mebrofenin cholescintigraphy in the evaluation of severity of steatosis in a rat model. Eur J Nucl Med Mol Imaging. 2006;33:110714. 97. Drane WE. Scintigraphic techniques for hepatic imaging. Radiol Clin N Am. 1998;36:309-18. 98. Minn H, Soini I. 18F-fluorodeoxyglucose scintigraphy in diagnosis and follow up of treatment in advanced breast cancer. Eur J Nucl Med. 1989;15:61-6.
Download