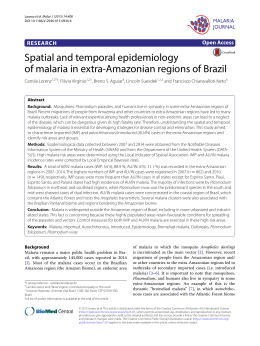
International Journal for Parasitology xxx (2012) xxx–xxx Contents lists available at SciVerse ScienceDirect International Journal for Parasitology journal homepage: www.elsevier.com/locate/ijpara Current Opinion On the pathogenesis of Plasmodium vivax malaria: Perspectives from the Brazilian field Fabio T.M. Costa a,⇑,1, Stefanie C.P. Lopes a,1, Letusa Albrecht a,1, Ricardo Ataíde b,1, André M. Siqueira c,d,1, Rodrigo M. Souza b,e,1, Bruce Russell f,1, Laurent Renia f,1, Claudio R.F. Marinho b,⇑,1, Marcus V.G. Lacerda c,d,⇑,1 a Departamento de Genética, Evolução e Bioagentes, Instituto de Biologia, Universidade Estadual de Campinas (UNICAMP), Campinas, SP, Brazil Departamento de Parasitologia, Universidade de São Paulo (USP), São Paulo, SP, Brazil c Fundação de Medicina Tropical Dr. Heitor Vieira Dourado, Gerência de Malária, Manaus, AM, Brazil d Universidade do Estado do Amazonas, Manaus, AM, Brazil e Centro Multidisciplinar, Universidade Federal do Acre (UFAC), Campus Floresta, Cruzeiro do Sul, AC, Brazil f Singapore Immunology Network, Agency for Science, Technology and Research, Singapore, Singapore b a r t i c l e i n f o Article history: Received 3 May 2012 Received in revised form 18 August 2012 Accepted 21 August 2012 Available online xxxx Keywords: Malaria Plasmodium vivax Clinical complications Cytoadhesion Pregnancy Pathogenesis Amazon Brazil a b s t r a c t Life-threatening Plasmodium vivax malaria cases, while uncommon, have been reported since the early 20th century. Unfortunately, the pathogenesis of these severe vivax malaria cases is still poorly understood. In Brazil, the proportion of vivax malaria cases has been steadily increasing, as have the number of cases presenting serious clinical complications. The most frequent syndromes associated with severe vivax malaria in Brazil are severe anaemia and acute respiratory distress. Additionally, P. vivax infection may also result in complications associated with pregnancy. Here, we review the latest findings on severe vivax malaria in Brazil. We also discuss how the development of targeted field research infrastructure in Brazil is providing clinical and ex vivo experimental data that benefits local and international efforts to understand the pathogenesis of P. vivax. Ó 2012 Australian Society for Parasitology Inc. Published by Elsevier Ltd. All rights reserved. 1. Introduction The assumption that vivax malaria is only associated with ‘benign’ (uncomplicated) syndromes has been challenged by a number of authoritative reviews on the pathogenesis of Plasmodium vivax (Mendis et al., 2001; Anstey et al., 2009; Mueller et al., 2009). Certainly, there have been well-documented reports of severe vivax in Brazil (Alexandre et al., 2010; Siqueira et al., 2010; Lanca et al., 2012). Unfortunately, the increased awareness ⇑ Corresponding authors. Address: Departamento de Genética, Evolução e Bioagentes, Instituto de Biologia, Universidade Estadual de Campinas – UNICAMP, P.O. Box 6109, 13083-970 Campinas, SP, Brazil. Tel.: +55 19 3521 6594; fax: +55 19 3521 6276 (F.T.M. Costa), Departamento de Parasitologia, Instituto de Ciências Biomédicas – ICB II, Universidade de São Paulo – USP, Av. Prof. Lineu Prestes 1374, Sala 44/40, São Paulo, SP 05508-900, Brazil. Tel.: +55 11 3091 7209 (C.R.F. Marinho), Fundação de Medicina Tropical Dr. Heitor Vieira Dourado, Av. Pedro Teixeira 25, Manaus, Amazonas 69040-000, Brazil. Tel.: +55 92 2127 3430 (M.V.G. Lacerda). E-mail addresses: [email protected], [email protected] (F.T.M. Costa), [email protected] (C.R.F. Marinho), [email protected] (M.V.G. Lacerda). 1 All authors equally contributed to this work. of severe syndromes associated with vivax malaria has not yet been matched by data to provide solid answers to why such cases occur. The lack of a robust, reproducible and long-term in vitro culture method has restricted the study of P. vivax pathobiology in humans to endemic areas with well-equipped laboratories (Suwanarusk et al., 2004; Handayani et al., 2009; Carvalho et al., 2010; Chotivanich et al., 2012). In this opinion article, we discuss the relevance of an adequate research infrastructure for the development of reliable in vivo and ex vivo functional assays in Brazilian endemic areas where infected patients can easily access hospitals with adequate facilities and personnel, such as the cities of Manaus (Amazonas State), Cruzeiro do Sul (Acre State) and Porto Velho (Rondônia State). In addition, recent observations regarding the pathogenesis of P. vivax disease are discussed and key questions are addressed. 2. Epidemiology of vivax malaria in Amazonian Brazil In Brazil, malaria transmission is largely confined to the Amazon region (99.8% of reported cases). The National Malaria Control 0020-7519/$36.00 Ó 2012 Australian Society for Parasitology Inc. Published by Elsevier Ltd. All rights reserved. http://dx.doi.org/10.1016/j.ijpara.2012.08.007 Please cite this article in press as: Costa, F.T.M., et al. On the pathogenesis of Plasmodium vivax malaria: Perspectives from the Brazilian field. Int. J. Parasitol. (2012), http://dx.doi.org/10.1016/j.ijpara.2012.08.007 2 F.T.M. Costa et al. / International Journal for Parasitology xxx (2012) xxx–xxx Program dictates all major control policies, which are followed by all states and municipalities. Due to the dramatic enhancement of the control measures, the number of malaria cases reported in Brazil has dropped almost 2-fold, from 635,646 cases in 1999, to less than 310,000 cases in 2009, when 85% of the reported cases were vivax malaria (DATASUS-SIVEP-Malária (http://portalweb04.saude.gov.br/sivep_malaria/default.asp). Despite these major advances achieved during the last decade, Brazil still reports 50–60% of the malaria cases in the Americas (WHO, 2011). Although Brazil’s population has become more urbanised, many inhabitants of the Amazon remain in riverine communities or recently colonised rural settlement areas; both in direct contact with rainforest and associated malaria risk. Thus, malaria remains an important public health issue for Brazil. Aside from the direct costs associated with uncomplicated and severe vivax malaria, this disease is also responsible for a more insidious socioeconomic burden. One specific example is the diminished school performance of Amazonian children associated with P. vivax infection (Vitor-Silva et al., 2009). The combination of rapidly occurring economic changes in the Amazon and the diversity of sociological and environmental settings present a complex interaction of several risk factors imposing relevant barriers for malaria control. Although peaks in Amazonian malaria transmission are correlated with seasonal rainfall patterns, enough basal malaria occurs to ensure a steady enrolment of patients in clinical trials year round. Most cases occur in the outskirts of major cities, where migrants with low or no immunity to malaria live in crowded places with little effective sanitation; such conditions promote outbreaks (Ferreira Goncalves and Alecrim, 2004; Gil et al., 2007). In contrast, people living in riverine communities are commonly exposed to malaria infection from a very young age and they tend to develop a sustained level of clinical ‘immunity’ by the age of 21–26 years (Alves et al., 2002). The epidemiology of malaria in recently colonised rural agroindustrial settlements has a pattern with features of open-cast mines and city outskirts (Camargo et al., 1994). The number of malaria attacks in the Amazon is consistently decreasing, with a marked reduction in the proportion of Plasmodium falciparum cases (Oliveira-Ferreira et al., 2010), making Brazil one of the few endemic areas in which P. vivax malaria is highly predominant. Certainly, in Manaus, P. falciparum malaria was reported in only 0.8% of the cases in 2011. Universal access to diagnostic health facilities throughout the Amazon region, resulting in 60% of patients being diagnosed by optical microscopy and treated within 48 h of presentation of symptoms, and the introduction of artemether/lumefantrine as the first-line of treatment for P. falciparum, have contributed to the decrease in malaria cases since 2007 (OliveiraFerreira et al., 2010). This unique setting allows P. vivax immunity to be evaluated in isolation without a significant confounding influence from sequential or mixed P. falciparum infections. The characteristics that make P. falciparum relatively easy to control (e.g., late gametocyte production and lack of hypnozoites) may result in P. vivax becoming the dominant malaria species in many endemic areas. The emergence of chloroquine-resistant P. vivax in Brazil and the lack of primaquine effectiveness (which are still the first-line drugs for vivax infection in Brazil) is a cause for considerable concern and will strengthen the dominance of this malaria species in the Amazon (de Santana Filho et al., 2007). 3. The development of tropical health research facilities in the Amazon In the Amazon region, every patient with a febrile illness has free access to malaria diagnosis and the appropriate antimalarial treatment, which by law are not sold in general pharmacies. Additionally, there is a robust databank system available on-line (SIVEP-Malária (http://portalweb04.saude.gov.br/sivep_malaria/ default.asp). Brazil has a socialised health system (Sistema Único de Saúde – SUS), providing well-equipped tertiary care centres throughout several urban centres in the Amazon (Fig. 1). Centres such as the Tropical Medicine Foundation Dr. Heitor Vieira Dourado Hospital (FMT-HVD) in Manaus and the Cruzeiro do Sul Maternity Ward (CSMW) in Cruzeiro do Sul, exemplify the type of hospitals in which research on P. vivax malaria clinical severity, drug resistance and pathogenesis can be effectively accomplished. FMT-HVD has 150 hospital beds, many of which are available for clinical trials, treats 30% of the malarial cases reported in Manaus and serves as the referral hospital for complicated cases. The CSMW admitted more than 2,000 pregnant women in 2009, with an estimated prevalence of plasmodial infections of 8.7% and with a predominance of P. vivax (75.2%) (Vale, S.d.C.N., 2011. Malária em gestantes no município de Cruzeiro do Sul pertencente à região amazônica brasileira. Ph.D. Thesis, Universidade de São Paulo, Brazil). Historically, Cruzeiro do Sul has been the municipality within Acre state with the highest number of malaria cases (87% in 2009). In 2011, a hospital dedicated to women and newborn health (the Women’s and Children’s Hospital of Juruá) was inaugurated and coupled to the Gestacional Clinical Malaria Research Centre and the Infectious Diseases Research Laboratory. These well-equipped laboratories in Manaus and Cruzeiro do Sul enable studies on P. vivax immunopathogenic mechanisms by facilitating the collection of P. vivax-infected erythrocytes (Pv-iE) from infected patients, with or without complications, from pregnant women’s peripheral blood and from P. vivax-infected placentas. Collection of human tissues and parasites allows the performance of functional (e.g., cytoadhesion, short-term culture and invasion) and molecular (e.g., genetic sequencing and gene expression) assays. Indeed, we believe that long-term partnerships with local, national and global research institutes will strengthen personnel capacity in situ, improve training of graduate and undergraduate students and enhance research quality. 4. Plasmodium vivax-attributable clinical complications and related pathogenesis The incidence of clinical complications in vivax malaria has been attributed to a variety of factors, such as: transmission intensity, the presence of other endemic or non-communicable disease host characteristics (gender, age and genetic background) and drug resistance. Anaemia and respiratory distress are the most common complications reported from vivax endemic areas (Genton et al., 2008; Tjitra et al., 2008; Kochar et al., 2009; Lacerda et al., 2012). Unusual complications of P. vivax infection, such as rhabdomyolysis (Siqueira et al., 2010), idiopathic thrombocytopenic purpura (Lacerda et al., 2004), splenic rupture (Lubitz, 1949; Lacerda et al., 2007; Gupta et al., 2010) and cerebral malaria (Tanwar et al., 2011) have also been reported in Brazil and southeast Asia. There are also a number of complications related to the haemolytic effect of primaquine in those with glucose-6-phosphate dehydrogenase (G6PD)-deficiency (Ramos Junior et al., 2010), a mutation with a prevalence of approximately 3% amongst males living in endemic areas of the Amazon region (Santana et al., 2009). The diversity of clinical presentations can also be attributed to each host’s unique immune response (Mourao et al., 2012), which may be directly linked to the transmission dynamics in a given area. For example, the recent decrease in P. falciparum cases in Brazil has been accompanied by an increase in P. vivax-related hospitalisations (Santos-Ciminera et al., 2007). Between 1998 and 2008, 234 vivax-associated malaria deaths were reported in Brazil (Oliveira-Ferreira et al., 2010). Within endemic areas of the Please cite this article in press as: Costa, F.T.M., et al. On the pathogenesis of Plasmodium vivax malaria: Perspectives from the Brazilian field. Int. J. Parasitol. (2012), http://dx.doi.org/10.1016/j.ijpara.2012.08.007 F.T.M. Costa et al. / International Journal for Parasitology xxx (2012) xxx–xxx 3 Manaus Amazonas State Population: 1,802,525 Annual Parasitic Index: 9,3 (2011) Plasmodium vivax: 98,7% Porto Velho Rondônia State Population: 435,732 Annual Parasitic Index: 34,4 (2011) Plasmodium vivax: 95,1% Cruzeiro do Sul Acre State Population: 78,444 Annual Parasitic Index: 162,3 (2011) Plasmodium vivax: 85,1% Fig. 1. The transmission of malaria in Brazil occurs almost exclusively in the Amazon region (99.8%). Urban centres such as Manaus, Cruzeiro do Sul and Porto Velho recorded approximately 20% of the national malaria cases in 2011, and in these three municipalities, tertiary care hospitals with the proper infrastructure for clinical research are available. Brazilian Amazon, rural settings have low to moderate vivax transmission rates (da Silva-Nunes et al., 2008; Silva et al., 2010), a stark contrast with the vibrant urban centres of Manaus, Cruzeiro do Sul and Porto Velho, which represent almost 20% of the Brazilian malaria cases (Gil et al., 2007; Saraiva et al., 2009; Costa et al., 2010). Even though urban settings have the best clinical infrastructure for the study of severe vivax malaria, long-term cohort studies in Brazilian urban settings are difficult due to a high level of human population transience. Despite these challenges, we have recently demonstrated that the World Health Organization’s severity criteria for P. falciparum reliably identified P. vivax-infected patients at risk for severe disease admitted to the intensive care unit (Lanca et al., 2012). In vivax endemic areas, the prevalence of both acute and chronic co-morbidities represent another relevant issue (Lampah et al., 2011; Lacerda et al., 2012). To search for other infectious agents causing acute febrile syndromes, an experienced and well-funded health system is needed. Furthermore, study of vivax-associated immunopathological mechanisms is hindered by a lack of post-mortem research, which is restricted by cultural and religious beliefs in many parts of southeast Asia (Anstey et al., 2009; Mueller et al., 2009), with a few exceptions such as the Melanesian populations (Manning et al., 2012). The most frequent complication of malaria in Brazil is anaemia, which causes increased morbidity and mortality in children and pregnant women (Haldar and Mohandas, 2009; Alexandre et al., 2010; Lanca et al., 2012). During vivax infections, erythrocytes are destroyed early on, but anaemia can persist even after parasite clearance. This observation can be explained primarily by the fact that P. vivax infects reticulocytes, and the infection prevents the reestablishment of the normal erythrocyte population (Collins et al., 2003). The growing incidence of severe vivax malaria complications (especially anaemia), or possibly the growing awareness and reporting from experts in the field, may be related to increased chloroquine resistance (Tjitra et al., 2008; Fernandez-Becerra et al., 2009), a situation also observed in Brazil (de Santana Filho et al., 2007), resulting in the longer persistence of the parasite in circulation and in the bone marrow. Respiratory distress is another common complication in vivax malaria reported worldwide (Anstey et al., 2007; Price et al., 2007; Tan et al., 2008), including Brazil (Lacerda et al., 2012). In the largest series of autopsies performed on patients with P. vivax infection in Manaus, acute lung oedema was the major finding in patients with respiratory distress, frequently associated with neutrophil accumulation in the interalveolar space (Lacerda et al., 2012) (Fig. 2). Although rarely observed in Brazil, patients presenting with neurological symptoms (e.g., seizure and/or coma) have been reported (Andrade and Barral-Netto, 2011; Lacerda et al., 2012). The immunopathogenesis of P. vivax is poorly understood. However, it was recently demonstrated that Brazilian patients with severe vivax malaria, who presented with respiratory failure and anaemia, had elevated levels of the inflammatory cytokines TNFa and IFN-c; these patients also had an increased IFN-c/IL-10 ratio and the antioxidant agent superoxide dismutase-1 (SOD-1) and soluble CD163 were also elevated (Andrade et al., 2010; Andrade and Barral-Netto, 2011; Mendonca et al., 2012). Levels of TNF-a and other inflammatory cytokines are higher during P. vivax Fig. 2. Post-mortem lung microscopy from a patient with respiratory distress. Acute oedema was the major finding (H&E staining; 1000 magnification). Scale bar = 20 lm. Please cite this article in press as: Costa, F.T.M., et al. On the pathogenesis of Plasmodium vivax malaria: Perspectives from the Brazilian field. Int. J. Parasitol. (2012), http://dx.doi.org/10.1016/j.ijpara.2012.08.007 4 F.T.M. Costa et al. / International Journal for Parasitology xxx (2012) xxx–xxx infections compared with P. falciparum infections with the same parasite load (Karunaweera et al., 1992; Yeo et al., 2010). Elevated plasma concentrations of microparticles were found in individuals with uncomplicated P. vivax infection in a study conducted in the Brazilian Amazon (Campos et al., 2010). Moreover, despite strong evidence that P. vivax triggers thrombocytopenia at higher levels than P. falciparum (Kochar et al., 2010), any role for these particles in severe P. vivax malaria is unknown. The paradigm of P. vivax red blood cell (RBC) invasion only in Duffy-positive individuals has been recently challenged, as it was shown that Duffy negative individuals can also be infected by P. vivax in Brazil (Cavasini et al., 2007). This finding paves the way, not only for the search of new vaccine candidates, but also for the better understanding of severe disease mechanisms. Regarding host genetics in Brazil, individuals with the Duffy negative Fy (a+b ) phenotype demonstrated a 30–80% reduced risk of clinical vivax, but not falciparum malaria, in a prospective cohort study in the Brazilian Amazon (King et al., 2011). G6PD deficiency, essentially the African type, seemed to protect against malaria based on the past history of enrolled patients in Manaus (Santana et al., 2009). 5. Cytoadhesion and rosetting phenomena in P. vivax malaria Because severe falciparum-like manifestations are increasingly present during vivax malaria, it is possible that the two species share some immunopathological processes. Normally, manifestations of severe P. falciparum infections (e.g., cerebral malaria, malaria in pregnancy (MiP) and respiratory distress) are associated with cytoadhesion, in which the mature-stage of P. falciparuminfected erythrocytes (Pf-iE) attach to the host’s cell-surface receptors. Pf-iE cytoadhesion to the endothelium prevents the circulation of mature parasites, which inhibits parasite clearance by the spleen (Wyler, 1983) and accordingly, mature stage parasites are often not observed in the peripheral circulation (Berendt et al., 1990). Because all stage-forms of P. vivax are found in the peripheral blood, it has been inferred that this parasite does not sequester and thus does not cytoadhere. Nevertheless, sequestration of P. vivax was proposed more than 50 years ago when a disproportionately low number of mature stage-form parasites (schizonts) were observed in the peripheral circulation (Leeson, 1957; Field et al., 1963). However whether sequestration in P. vivax leads to a disproportional organ-specific and peripheral blood parasitaemia remains to be evaluated. We have recently shown that Pv-iE from non-severe patients cytoadhered ex vivo to placental cryosections as well as to human lung (HLEC) and Saimiri brain (SBEC) endothelial cell lines under static and flow conditions (Carvalho et al., 2010). While the number of adhered Pv-iE per mm2 under static conditions was 10–15 times lower than that for Pf-iE, the adhesion strength under physiological (i.e., flow) conditions was similar in both parasites. Moreover, in transfected Chinese hamster ovary (CHO) cells, Pv-iE binding to CHO-ICAM-1 was twice as high as that of mock- or CD36-transfected cells, indicating that ICAM-1 is a potential receptor for P. vivax. Pv-iE were also able to bind to placental cryosections. Adhesion to HLEC was inhibited by soluble chondroitin sulfate A (CSA), but treatment with chondroitinase ABC did not affect binding (Carvalho et al., 2010). The ability of CSA binding has been recently confirmed using Pv-iE collected from 33 patients from Asia-Pacific region (Chotivanich et al., 2012). In this study, all tested isolates adhered to immobilised CSA and hyaluronic acid (HA), and pre-incubation with chondroitinase and hyaluronidase reversed binding (Chotivanich et al., 2012). A family of variant subtelomeric P. vivax genes named vir was described in the early 2000s (del Portillo et al., 2001). Unlike the var genes of P. falciparum, which encode PfEMP-1 proteins, few vir genes (160 of 346) have motifs similar to the Plasmodium export element/vacuolar transport signal (PEXEL/VTS) proteins. PEXEL/ VTS-family proteins mediate protein export to the erythrocyte surface and the cytosol (Marti et al., 2004). In contrast to PfEMP-1, VIRs are not clonally expressed (Fernandez-Becerra et al., 2005) and can be found inside reticulocytes, implying that they have different sub-cellular localisations and functions (Fernandez-Becerra et al., 2005). Based on their variant nature and their presence on the erythrocyte membrane, VIR proteins were evaluated for their role in Pv-iE cytoadhesion to endothelial cells. Polyclonal antibodies against recombinant VIR proteins from two subfamilies (VIRE4 and VIRA5) inhibited Pv-iE adhesion ex vivo to HLEC (Carvalho et al., 2010). Due to the lack of an in vitro P. vivax culture system, Bernabeu and colleagues elegantly assessed the role of VIR proteins in P. vivax cytoadhesion via a transfection assay; P. falciparum 3D7 was transfected with recombinant VIR proteins (VIR17, VIR14 and VIR10) (Bernabeu et al., 2012). Both VIR14 and VIR10 were exported to the cell membrane, but only VIR14 mediated binding to ICAM-1 (Bernabeu et al., 2012). This result corroborated our previous data (Carvalho et al., 2010). Although P. vivax cytoadheres under relatively low shear stresses, whether this is part of a strategy to avoid spleen clearance, as postulated for P. falciparum, is still not determined. If this is indeed the case, it has been proposed that VIR antigens promote Pv-iE adhesion to barrier cells, which are located in protected areas of the spleen, to allow parasite survival and the establishment of a chronic infection (del Portillo et al., 2004). However, such a strategy could be considered in the light that biomechanical modifications of Pv-iE might allow the evasion of splenic clearance. Certainly, Pv-iE are significantly more deformable than P. falciparum-infected erythrocytes (Suwanarusk et al., 2004), and this deformability could allow a certain number of Pv-iE to bypass the splenic sinusoids, thus avoiding pitting (Handayani et al., 2009). While Pv-iE adhesion to cell receptors has been demonstrated, the role of cytoadhesion in P. vivax pathogenesis and severe disease is unknown. A challenge for the study of severe infection is the scarcity of autopsy studies. Early 20th century autopsies of patients with P. vivax infection recorded intra-capillary masses of swollen, infected erythrocytes, malarial pigment and the existence of mature parasites within a red blood cell taking up the entire lumen and in contact with endothelial cells in some brain vessels (reviewed by Anstey et al., 2009). However, as the diagnoses were made exclusively with microscopic evidence, these observations must be analysed carefully because these reports do not exclude the possibility of mixed infections or co-morbidities. One single autopsy performed due to legal reasons in a woman with severe vivax disease, in India, showed alveolar capillaries congested by monocyte infiltrates and diffuse damage to alveolar membranes compatible with ALI/ARDS (Acute Lung Injury/Acute Respiratory Distress Syndrome); in this case, P. falciparum infection was excluded by PCR analysis (Valecha et al., 2009). More recently, 17 patients with microscopical diagnosis of vivax malaria were fully autopsied in Manaus. Infection with a single parasite species was confirmed in 13 cases by PCR performed in paraffin-fixed tissues. In 13 patients, the parasitic infection was related to the cause of death. In one patient who tested negative for peripheral parasitaemia many days after antimalarial treatment, parasites were still detected by confocal microscopy in the lung tissue. These results suggested that the parasite was sequestered in the lungs (Lacerda et al., 2012). Indeed, it has been suggested that the pulmonary vascular sequestration of Pv-iE could be the pathophysiological mechanism that leads to this potentially fatal complication (Anstey et al., 2007), although ex vivo Pv-iE binding assays were not performed in that particular work. Please cite this article in press as: Costa, F.T.M., et al. On the pathogenesis of Plasmodium vivax malaria: Perspectives from the Brazilian field. Int. J. Parasitol. (2012), http://dx.doi.org/10.1016/j.ijpara.2012.08.007 F.T.M. Costa et al. / International Journal for Parasitology xxx (2012) xxx–xxx 5 Fig. 3. Infected erythrocytes and inflammatory cells are present in the placental intervillous spaces of a Plasmodium vivax-infected pregnant woman. (A) H&E staining; scale bar = 20 lm. (B) Giemsa staining; scale bar = 20 lm. Mononuclear cells (arrows), hemozoin within mononuclear cells (arrow heads), terminal villi (stars). The other adhesive phenotype observed in malaria parasites is rosette formation. Many studies on rosetting have focused on P. falciparum (Mercereau-Puijalon et al., 2008), but little is known about rosetting in P. vivax or other Plasmodium spp. Almost 20 years have passed since the first report of rosetting in P. vivax (Udomsanpetch et al., 1995), and to date there are only four studies from southeast Asia that have reported rosette formation by P. vivax (Udomsanpetch et al., 1995; Chotivanich et al., 1998, 2012; Russell et al., 2011). In contrast to P. falciparum, P. vivax rosetting has not been associated with disease severity, parasitaemia or the ABO blood group type (Udomsanpetch et al., 1995; Chotivanich et al., 1998; Russell et al., 2011). Russell and colleagues have shown that enrichment of some P. vivax isolates requires trypsin treatment to disrupt rosettes, suggesting that trypsin-sensitive proteins mediate rosetting in Pv-iEs (Russell et al., 2011). In the four studies that describe rosetting in P. vivax, almost all of the isolates analysed formed rosettes (Udomsanpetch et al., 1995; Chotivanich et al., 1998, 2012; Russell et al., 2011). To date, there is no information about rosette formation or about its biological meaning in Pv-iEs harvested from patients outside of the Asia-Pacific region. 6. Malaria in pregnancy (MiP): a particular syndrome The majority of the studies on P. vivax infection during pregnancy have been conducted in the Asia-Pacific region (Nosten et al., 1991; McGready et al., 2004, 2011; Rijken et al., 2012). There are very few studies from other regions that look specifically at the placental pathology of P. vivax infections and this lack of information urges further studies (Anstey et al., 2009). A single study has systematically evaluated the histopathology of P. vivax in the placenta. In this study, the intervillous spaces of the placenta contained accumulations of parasitised erythrocytes and malarial pigment deposits, but there were no other significant tissue changes (McGready et al., 2011). In Latin America, some studies were based on placental biopsies from P. vivax-infected women, but these were used only as a marker of infection and failed to systematically evaluate the parasite-associated lesions (Parekh et al., 2010; Campos et al., 2011). In Brazil, MiP studies have focused on the epidemiology and on the consequences of malarial infections for both the mother and the newborn (Martinez-Espinosa et al., 2004; Chagas et al., 2009; Carvalho et al., 2011). In those studies, low birth weight, abortion and premature delivery were reported and co-morbidities did not seem to be relevant (reviewed in Lacerda et al. (2012)). Preliminary results from a prospective study, in Cruzeiro do Sul, show that women with P. vivax infections during pregnancy can evolve with parasites and immune cells in the placenta (Fig. 3) besides showing other signs of placental pathology such as increased syncytial knotting, also associated with P. falciparum (Souza, RM, unpublished observations). These results complement those reported elsewhere (McGready et al., 2004), and highlight the importance of studying P. vivax-associated pathology in diverse endemic scenarios where the heterogeneous occurrence of comorbidities in the placental tissue (e.g., syphilis, toxoplasmosis, cytomegalovirus) may occur. 7. More questions than answers Little is known about P. vivax pathogenesis in severe malaria cases. Plasmodium vivax is very difficult to grow in vitro, despite recent advances (Udomsangpetch et al., 2007; Russell et al., 2011), and there are no highly specific and reliable biomarkers for infection severity. These impediments have prevented researchers from addressing crucial issues. To better understand vivax severity, the following key questions are: (i) are co-morbidities such as bacterial infections or dengue fever essential to P. vivax severity? (ii) As PviE cytoadhesion is 10- to 15-fold less than that of Pf-iE in vivo, do non-parasitic factors (e.g., platelets, microparticles and complement molecules) enhance adhesion in vivo, and are co-morbidities responsible for the production of those factors? (iii) Since VIR proteins are not clonally expressed, are there other host receptors besides ICAM-1 and CSA that play a role in Pv-iE binding for the same parasite stage form? (iv) Does rosette formation play a role in P. vivax severity and does this phenomenon enhance parasite RBC infection? (v) What is the real impact of vivax infection on pregnant women and foetal health, and which host or parasite factors are involved? 8. Concluding remarks To better understand P. vivax infections and their clinical complications in Brazil, future studies should focus on the immunopathological mechanisms related to P. vivax severity. The role of Pv-iE cytoadhesion in severe vivax malaria, as well as the major determinants of adhesion, should be better characterised. Autopsy reports of P. vivax-related fatalities with good clinical characterisations should include prospective histopathological descriptions of infected organs, as these details are urgently needed. Plasmodium vivax infections should be thoroughly studied in the general population and in specific severe cases. FMT-HVD (Manaus, Amazonas State) and the CSMW (Cruzeiro do Sul, Acre State) have laboratory facilities and well-equipped hospitals, which amongst others in the Amazon, are at the forefront of P. vivax clinical and epidemiological research in Brazil. Please cite this article in press as: Costa, F.T.M., et al. On the pathogenesis of Plasmodium vivax malaria: Perspectives from the Brazilian field. Int. J. Parasitol. (2012), http://dx.doi.org/10.1016/j.ijpara.2012.08.007 6 F.T.M. Costa et al. / International Journal for Parasitology xxx (2012) xxx–xxx Acknowledgements This work received financial support from Fundação de Amparo a Pesquisa do Estado de São Paulo (FAPESP, Brazil), Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq, Brazil), Instituto Nacional de Tecnologia em Vacinas (CNPq-FAPEMIG, Brazil) and Instituto Nacional de Tecnologia em Doenças Negligenciadas (CNPq, Brazil). S.C.P.L., L.A. and R.A. were sponsored by FAPESP fellowships. R.M.S was supported by a CNPq fellowship. MVGL and FTMC are CNPq fellows. FTMC is enrolled at the Programa Estratégico de Ciência, Tecnologia & Inovação nas Fundações Estaduais de Saúde (PECTI/AM Saúde) from Fundação de Amparo à Pesquisa do Estado do Amazonas (FAPEAM, Brazil). L.R. and B.R. were supported by core grants to the Singapore Immunology Network and the Horizontal programme on Infectious Diseases, Agency for Science, Technology and Research (A⁄STAR), Singapore. The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript. Special thanks to Dr. Tony Hiroshi Katsuragawa (Instituto de Pesquisas em Patologias Tropicais – Porto Velho, Rondônia, Brazil) for the data on the annual parasitic index and the proportion P. vivax cases in Porto Velho. References Alexandre, M.A., Ferreira, C.O., Siqueira, A.M., Magalhaes, B.L., Mourao, M.P., Lacerda, M.V., Alecrim, M.G., 2010. Severe Plasmodium vivax malaria, Brazilian Amazon. Emerg. Infect. Dis. 16, 1611–1614. Alves, F.P., Durlacher, R.R., Menezes, M.J., Krieger, H., Silva, L.H., Camargo, E.P., 2002. High prevalence of asymptomatic Plasmodium vivax and Plasmodium falciparum infections in native Amazonian populations. Am. J. Trop. Med. Hyg. 66, 641– 648. Andrade, B.B., Reis-Filho, A., Souza-Neto, S.M., Clarencio, J., Camargo, L.M., Barral, A., Barral-Netto, M., 2010. Severe Plasmodium vivax malaria exhibits marked inflammatory imbalance. Malar. J. 9, 13. Andrade, B.B., Barral-Netto, M., 2011. Biomarkers for susceptibility to infection and disease severity in human malaria. Mem. Inst. Oswaldo Cruz 106 (Suppl. 1), 70– 78. Anstey, N.M., Handojo, T., Pain, M.C., Kenangalem, E., Tjitra, E., Price, R.N., Maguire, G.P., 2007. Lung injury in vivax malaria: pathophysiological evidence for pulmonary vascular sequestration and posttreatment alveolar-capillary inflammation. J. Infect. Dis. 195, 589–596. Anstey, N.M., Russell, B., Yeo, T.W., Price, R.N., 2009. The pathophysiology of vivax malaria. Trends Parasitol. 25, 220–227. Berendt, A.R., Ferguson, D.J., Newbold, C.I., 1990. Sequestration in Plasmodium falciparum malaria: sticky cells and sticky problems. Parasitol. Today 6, 247– 254. Bernabeu, M., Lopez, F.J., Ferrer, M., Martin-Jaular, L., Razaname, A., Corradin, G., Maier, A.G., Del Portillo, H.A., Fernandez-Becerra, C., 2012. Functional analysis of Plasmodium vivax VIR proteins reveals different subcellular localizations and cytoadherence to the ICAM-1 endothelial receptor. Cell Microbiol. 14, 386–400. Camargo, L.M., Ferreira, M.U., Krieger, H., De Camargo, E.P., Da Silva, L.P., 1994. Unstable hypoendemic malaria in Rondonia (western Amazon region, Brazil): epidemic outbreaks and work-associated incidence in an agro-industrial rural settlement. Am. J. Trop. Med. Hyg. 51, 16–25. Campos, F.M., Franklin, B.S., Teixeira-Carvalho, A., Filho, A.L., de Paula, S.C., Fontes, C.J., Brito, C.F., Carvalho, L.H., 2010. Augmented plasma microparticles during acute Plasmodium vivax infection. Malar. J. 9, 327. Campos, I.M., Uribe, M.L., Cuesta, C., Franco-Gallego, A., Carmona-Fonseca, J., Maestre, A., 2011. Diagnosis of gestational, congenital, and placental malaria in Colombia: comparison of the efficacy of microscopy, nested polymerase chain reaction, and histopathology. Am. J. Trop. Med. Hyg. 84, 929–935. Carvalho, B.O., Lopes, S.C., Nogueira, P.A., Orlandi, P.P., Bargieri, D.Y., Blanco, Y.C., Mamoni, R., Leite, J.A., Rodrigues, M.M., Soares, I.S., Oliveira, T.R., Wunderlich, G., Lacerda, M.V., del Portillo, H.A., Araujo, M.O., Russell, B., Suwanarusk, R., Snounou, G., Renia, L., Costa, F.T., 2010. On the cytoadhesion of Plasmodium vivax-infected erythrocytes. J. Infect. Dis. 202, 638–647. Carvalho, B.O., Matsuda, J.S., Luz, S.L., Martinez-Espinosa, F.E., Leite, J.A., Franzin, F., Orlandi, P.P., Gregoracci, G.B., Lacerda, M.V., Nogueira, P.A., Costa, F.T., 2011. Gestational malaria associated to Plasmodium vivax and Plasmodium falciparum placental mixed-infection followed by foetal loss: a case report from an unstable transmission area in Brazil. Malar. J. 10, 178. Cavasini, C.E., Mattos, L.C., Couto, A.A., Bonini-Domingos, C.R., Valencia, S.H., Neiras, W.C., Alves, R.T., Rossit, A.R., Castilho, L., Machado, R.L., 2007. Plasmodium vivax infection among Duffy antigen-negative individuals from the Brazilian Amazon region: an exception? Trans. R. Soc. Trop. Med. Hyg. 101, 1042–1044. Chagas, E.C., do Nascimento, C.T., de Santana Filho, F.S., Botto-Menezes, C.H., Martinez-Espinosa, F.E., 2009. Impact of malaria during pregnancy in the Amazon region. Rev. Panam. Salud Publica 26, 203–208. Chotivanich, K.T., Pukrittayakamee, S., Simpson, J.A., White, N.J., Udomsangpetch, R., 1998. Characteristics of Plasmodium vivax-infected erythrocyte rosettes. Am. J. Trop. Med. Hyg. 59, 73–76. Chotivanich, K., Udomsangpetch, R., Suwanarusk, R., Pukrittayakamee, S., Wilairatana, P., Beeson, J.G., Day, N.P., White, N.J., 2012. Plasmodium vivax adherence to placental glycosaminoglycans. PLoS One 7, e34509. Collins, W.E., Jeffery, G.M., Roberts, J.M., 2003. A retrospective examination of anemia during infection of humans with Plasmodium vivax. Am. J. Trop. Med. Hyg. 68, 410–412. Costa, K.M., Almeida, W.A., Magalhaes, I.B., Montoya, R., Moura, M.S., Lacerda, M.V., 2010. Malaria in Cruzeiro do Sul (Western Brazilian Amazon): analysis of the historical series from 1998 to 2008. Rev. Panam. Salud Publica 28, 353–360. da Silva-Nunes, M., Codeco, C.T., Malafronte, R.S., da Silva, N.S., Juncansen, C., Muniz, P.T., Ferreira, M.U., 2008. Malaria on the Amazonian frontier: transmission dynamics, risk factors, spatial distribution, and prospects for control. Am. J. Trop. Med. Hyg. 79, 624–635. de Santana Filho, F.S., Arcanjo, A.R., Chehuan, Y.M., Costa, M.R., Martinez-Espinosa, F.E., Vieira, J.L., Barbosa, M.G., Alecrim, W.D., Alecrim, M.G., 2007. Chloroquineresistant Plasmodium vivax, Brazilian Amazon. Emerg. Infect. Dis. 13, 1125– 1126. del Portillo, H.A., Fernandez-Becerra, C., Bowman, S., Oliver, K., Preuss, M., Sanchez, C.P., Schneider, N.K., Villalobos, J.M., Rajandream, M.A., Harris, D., Pereira da Silva, L.H., Barrell, B., Lanzer, M., 2001. A superfamily of variant genes encoded in the subtelomeric region of Plasmodium vivax. Nature 410, 839–842. del Portillo, H.A., Lanzer, M., Rodriguez-Malaga, S., Zavala, F., Fernandez-Becerra, C., 2004. Variant genes and the spleen in Plasmodium vivax malaria. Int. J. Parasitol. 34, 1547–1554. Fernandez-Becerra, C., Pein, O., de Oliveira, T.R., Yamamoto, M.M., Cassola, A.C., Rocha, C., Soares, I.S., de Braganca Pereira, C.A., del Portillo, H.A., 2005. Variant proteins of Plasmodium vivax are not clonally expressed in natural infections. Mol. Microbiol. 58, 648–658. Fernandez-Becerra, C., Pinazo, M.J., Gonzalez, A., Alonso, P.L., del Portillo, H.A., Gascon, J., 2009. Increased expression levels of the pvcrt-o and pvmdr1 genes in a patient with severe Plasmodium vivax malaria. Malar. J. 8, 55. Ferreira Goncalves, M.J., Alecrim, W.D., 2004. Non-planed urbanization as a contributing factor for malaria incidence in Manaus-Amazonas. Braz. Rev. Salud Publica (Bogota) 6, 156–166. Field, J.W., Sandosham, A.A., Fong, Y.L., 1963. A Morphological Study of the Erythrocitic Parasites in Thick Blood Films, the Microscopic Diagnosis Of Human Malaria. The Government Press, Kuala Lumpur, pp. 20–117. Genton, B., D’Acremont, V., Rare, L., Baea, K., Reeder, J.C., Alpers, M.P., Muller, I., 2008. Plasmodium vivax and mixed infections are associated with severe malaria in children: a prospective cohort study from Papua New Guinea. PLoS Med. 5, e127. Gil, L.H., Tada, M.S., Katsuragawa, T.H., Ribolla, P.E., da Silva, L.H., 2007. Urban and suburban malaria in Rondonia (Brazilian Western Amazon) II. Perennial transmissions with high anopheline densities are associated with human environmental changes. Mem. Inst. Oswaldo Cruz 102, 271–276. Gupta, B.K., Sharma, K., Nayak, K.C., Agrawal, T.D., Binani, A., Purohit, V.P., Kochar, D.K., 2010. A case series of splenic infarction during acute malaria in northwest Rajasthan. India. Trans. R. Soc. Trop. Med. Hyg. 104, 81–83. Haldar, K., Mohandas, N., 2009. Malaria, Erythrocytic Infection, and Anemia. Hematology Am. Soc. Hematol. Educ. Program, Washington, pp. 87–93. Handayani, S., Chiu, D.T., Tjitra, E., Kuo, J.S., Lampah, D., Kenangalem, E., Renia, L., Snounou, G., Price, R.N., Anstey, N.M., Russell, B., 2009. High deformability of Plasmodium vivax-infected red blood cells under microfluidic conditions. J. Infect. Dis. 199, 445–450. Karunaweera, N.D., Grau, G.E., Gamage, P., Carter, R., Mendis, K.N., 1992. Dynamics of fever and serum levels of tumor necrosis factor are closely associated during clinical paroxysms in Plasmodium vivax malaria. Proc. Natl. Acad. Sci. USA 89, 3200–3203. King, C.L., Adams, J.H., Xianli, J., Grimberg, B.T., McHenry, A.M., Greenberg, L.J., Siddiqui, A., Howes, R.E., da Silva-Nunes, M., Ferreira, M.U., Zimmerman, P.A., 2011. Fya/Fyb antigen polymorphism in human erythrocyte Duffy antigen affects susceptibility to Plasmodium vivax malaria. Proc. Natl. Acad. Sci. USA 108, 20113–20118. Kochar, D.K., Das, A., Kochar, S.K., Saxena, V., Sirohi, P., Garg, S., Kochar, A., Khatri, M.P., Gupta, V., 2009. Severe Plasmodium vivax malaria: a report on serial cases from Bikaner in northwestern India. Am. J. Trop. Med. Hyg. 80, 194–198. Kochar, D.K., Das, A., Kochar, A., Middha, S., Acharya, J., Tanwar, G.S., Gupta, A., Pakalapati, D., Garg, S., Saxena, V., Subudhi, A.K., Boopathi, P.A., Sirohi, P., Kochar, S.K., 2010. Thrombocytopenia in Plasmodium falciparum, Plasmodium vivax and mixed infection malaria: a study from Bikaner (Northwestern India). Platelets 21, 623–627. Lacerda, M.V., Alexandre, M.A., Santos, P.D., Arcanjo, A.R., Alecrim, W.D., Alecrim, M.G.C., 2004. Idiopathic thrombocytopenic purpura due to vivax malaria in the Brazilian Amazon. Acta Trop. 90, 187–190. Lacerda, M.V.G., Oliveira, S.L., Alecrim, M.G.C., 2007. Splenic hematoma in a patient with Plasmodium vivax malaria. Rev. Soc. Bras. Med. Trop. 40, 96–97. Lacerda, M.V., Mourao, M.P., Alexandre, M.A., Siqueira, A.M., Magalhaes, B.M., Martinez-Espinosa, F.E., Filho, F.S., Brasil, P., Ventura, A.M., Tada, M.S., Couto, V.S., Silva, A.R., Silva, R.S., Alecrim, M.G., 2012. Understanding the clinical Please cite this article in press as: Costa, F.T.M., et al. On the pathogenesis of Plasmodium vivax malaria: Perspectives from the Brazilian field. Int. J. Parasitol. (2012), http://dx.doi.org/10.1016/j.ijpara.2012.08.007 F.T.M. Costa et al. / International Journal for Parasitology xxx (2012) xxx–xxx spectrum of complicated Plasmodium vivax malaria: a systematic review on the contributions of the Brazilian literature. Malar. J. 11, 12. Lacerda, M.V., Fragoso, S.C., Alecrim, M.G., Alexandre, M.A., Magalhaes, B.M., Siqueira, A.M., Ferreira, L.C., Araujo, J.R., Mourao, M.P., Ferrer, M., Castillo, P., Martin-Jaular, L., Fernandez-Becerra, C., Del Portillo, H., Ordi, J., Alonso, P.L., Bassat, Q., 2012. Postmortem characterization of patients with clinical diagnosis of Plasmodium vivax malaria: to what extent does this parasite kill? Clin. Infect. Dis. 55, e67–e74. Lampah, D.A., Yeo, T.W., Hardianto, S.O., Tjitra, E., Kenangalem, E., Sugiarto, P., Price, R.N., Anstey, N.M., 2011. Coma associated with microscopy-diagnosed Plasmodium vivax: a prospective study in Papua. Indonesia. PLoS Negl. Trop. Dis. 5, e1032. Lanca, E.F., Magalhaes, B.M., Vitor-Silva, S., Siqueira, A.M., Benzecry, S.G., Alexandre, M.A., O’Brien, C., Bassat, Q., Lacerda, M.V., 2012. Risk factors and characterization of Plasmodium vivax-associated admissions to pediatric intensive care units in the Brazilian Amazon. PLoS One 7, e35406. Leeson, H.S., 1957. Microscopic diagnosis of human malaria. A morphological-study of erythrocytic parasites. R. Soc. Health J. 2, 694. Lubitz, J.M., 1949. Pathology of the ruptured spleen in acute vivax malaria. Blood 4, 1168–1176. Manning, L., Rosanas-Urgell, A., Laman, M., Edoni, H., McLean, C., Mueller, I., Siba, P., Davis, T.M., 2012. A histopathologic study of fatal paediatric cerebral malaria caused by mixed Plasmodium falciparum/Plasmodium vivax infections. Malar. J. 11, 107. Marti, M., Good, R.T., Rug, M., Knuepfer, E., Cowman, A.F., 2004. Targeting malaria virulence and remodeling proteins to the host erythrocyte. Science 306, 1930–1933. Martinez-Espinosa, F.E., Daniel-Ribeiro, C.T., Alecrim, W.D., 2004. Malaria during pregnancy in a reference centre from the Brazilian Amazon: unexpected increase in the frequency of Plasmodium falciparum infections. Mem. Inst. Oswaldo Cruz 99, 19–21. McGready, R., Davison, B.B., Stepniewska, K., Cho, T., Shee, H., Brockman, A., Udomsangpetch, R., Looareesuwan, S., White, N.J., Meshnick, S.R., Nosten, F., 2004. The effects of Plasmodium falciparum and P. vivax infections on placental histopathology in an area of low malaria transmission. Am. J. Trop. Med. Hyg. 70, 398–407. McGready, R., Lee, S., Wiladphaingern, J., Ashley, E., Rijken, M., Boel, M., Simpson, J., Paw, M., Pimanpanarak, M., Mu, O., Singhasivanon, P., White, N., Nosten, F., 2011. Adverse effects of falciparum and vivax malaria and the safety of antimalarial treatment in early pregnancy: a population-based study. Lancet Infect. Dis. 12, 388–396. Mendis, K., Sina, B.J., Marchesini, P., Carter, R., 2001. The neglected burden of Plasmodium vivax malaria. Am. J. Trop. Med. Hyg. 64, 97–106. Mendonca, V.R., Luz, N.F., Santos, N.J., Borges, V.M., Goncalves, M.S., Andrade, B.B., Barral-Netto, M., 2012. Association between the haptoglobin and heme oxygenase 1 genetic profiles and soluble CD163 in susceptibility to and severity of human malaria. Infect. Immun. 80, 1445–1454. Mercereau-Puijalon, O., Guillotte, M., Vigan-Womas, I., 2008. Rosetting in Plasmodium falciparum: a cytoadherence phenotype with multiple actors. Transfus. Clin. Biol. 15, 62–71. Mourao, L.C., Morais, C.G., Bueno, L.L., Jimenez, M.C., Soares, I.S., Fontes, C.J., Guimaraes Lacerda, M.V., Xavier, M.S., Barnwell, J.W., Galinski, M.R., Braga, E.M., 2012. Naturally acquired antibodies to Plasmodium vivax blood-stage vaccine candidates (PvMSP-1(19) and PvMSP-3alpha(359–798)) and their relationship with hematological features in malaria patients from the Brazilian Amazon. Microbes Infect. 14, 730–739. Mueller, I., Galinski, M.R., Baird, J.K., Carlton, J.M., Kochar, D.K., Alonso, P.L., del Portillo, H.A., 2009. Key gaps in the knowledge of Plasmodium vivax, a neglected human malaria parasite. Lancet Infect. Dis. 9, 555–566. Nosten, F., ter Kuile, F., Maelankirri, L., Decludt, B., White, N.J., 1991. Malaria during pregnancy in an area of unstable endemicity. Trans. R. Soc. Trop. Med. Hyg. 85, 424–429. Oliveira-Ferreira, J., Lacerda, M.V., Brasil, P., Ladislau, J.L., Tauil, P.L., Daniel-Ribeiro, C.T., 2010. Malaria in Brazil: an overview. Malar. J. 9, 115. Parekh, F.K., Davison, B.B., Gamboa, D., Hernandez, J., Branch, O.H., 2010. Placental histopathologic changes associated with subclinical malaria infection and its impact on the fetal environment. Am. J. Trop. Med. Hyg. 83, 973–980. Price, R.N., Tjitra, E., Guerra, C.A., Yeung, S., White, N.J., Anstey, N.M., 2007. Vivax malaria: neglected and not benign. Am. J. Trop. Med. Hyg. 77, 79–87. 7 Ramos Junior, W.M., Sardinha, J.F., Costa, M.R., Santana, M.S., Alecrim, M.G., Lacerda, M.V., 2010. Clinical aspects of hemolysis in patients with P. vivax malaria treated with primaquine, in the Brazilian Amazon. Braz. J. Infect. Dis. 14, 410– 412. Rijken, M.J., Papageorghiou, A.T., Thiptharakun, S., Kiricharoen, S., Dwell, S.L., Wiladphaingern, J., Pimanpanarak, M., Kennedy, S.H., Nosten, F., McGready, R., 2012. Ultrasound evidence of early fetal growth restriction after maternal malaria infection. PLoS One 7, e31411. Russell, B., Suwanarusk, R., Borlon, C., Costa, F.T., Chu, C.S., Rijken, M.J., Sriprawat, K., Warter, L., Koh, E.G., Malleret, B., Colin, Y., Bertrand, O., Adams, J.H., D’Alessandro, U., Snounou, G., Nosten, F., Renia, L., 2011. A reliable ex vivo invasion assay of human reticulocytes by Plasmodium vivax. Blood 118, e74– e81. Santana, M.S., Lacerda, M.V.G., Barbosa, M.G.V., Alecrim, W.D., Alecrim, M.G.C., 2009. Glucose-6-phosphate dehydrogenase deficiency in an endemic area for malaria in Manaus: a cross-sectional survey in the Brazilian Amazon. PLoS One 4, e5259. Santos-Ciminera, P.D., Roberts, D.R., Alecrim, M.G., Costa, M.R., Quinnan Jr., G.V., 2007. Malaria diagnosis and hospitalization trends. Braz. Emerg. Infec. Dis. 13, 1597–1600. Saraiva, M.G., Amorim, R.D., Moura, M.A., Martinez-Espinosa, F.E., Barbosa, M.G., 2009. Urban expansion and spatial distribution of malaria in the municipality of Manaus, State of Amazonas. Rev. Soc. Bras. Med. Trop. 42, 515–522. Silva, N.S., Silva-Nunes, M., Malafronte, R.S., Menezes, M.J., D’Arcadia, R.R., Komatsu, N.T., Scopel, K.K., Braga, E.M., Cavasini, C.E., Cordeiro, J.A., Ferreira, M.U., 2010. Epidemiology and control of frontier malaria in Brazil: lessons from community-based studies in rural Amazonia. Trans. R. Soc. Trop. Med. Hyg. 104, 343–350. Siqueira, A.M., Alexandre, M.A., Mourao, M.P., Santos, V.S., Nagahashi-Marie, S.K., Alecrim, M.G., Lacerda, M.V., 2010. Severe rhabdomyolysis caused by Plasmodium vivax malaria in the Brazilian Amazon. Am. J. Trop. Med. Hyg. 83, 271–273. Suwanarusk, R., Cooke, B.M., Dondorp, A.M., Silamut, K., Sattabongkot, J., White, N.J., Udomsangpetch, R., 2004. The deformability of red blood cells parasitized by Plasmodium falciparum and P. vivax. J. Infect. Dis. 189, 190–194. Tan, L.K., Yacoub, S., Scott, S., Bhagani, S., Jacobs, M., 2008. Acute lung injury and other serious complications of Plasmodium vivax malaria. Lancet Infect. Dis. 8, 449–454. Tanwar, G.S., Khatri, P.C., Sengar, G.S., Kochar, A., Kochar, S.K., Middha, S., Tanwar, G., Khatri, N., Pakalapati, D., Garg, S., Das, A., Kochar, D.K., 2011. Clinical profiles of 13 children with Plasmodium vivax cerebral malaria. Ann. Trop. Paediatr. 31, 351–356. Tjitra, E., Anstey, N.M., Sugiarto, P., Warikar, N., Kenangalem, E., Karyana, M., Lampah, D.A., Price, R.N., 2008. Multidrug-resistant Plasmodium vivax associated with severe and fatal malaria: a prospective study in Papua. Indonesia. PLoS Med. 5, e128. Udomsanpetch, R., Thanikkul, K., Pukrittayakamee, S., White, N.J., 1995. Rosette formation by Plasmodium vivax. Trans. R. Soc. Trop. Med. Hyg. 89, 635–637. Udomsangpetch, R., Somsri, S., Panichakul, T., Chotivanich, K., Sirichaisinthop, J., Yang, Z., Cui, L., Sattabongkot, J., 2007. Short-term in vitro culture of field isolates of Plasmodium vivax using umbilical cord blood. Parasitol. Int. 56, 65– 69. Valecha, N., Pinto, R.G., Turner, G.D., Kumar, A., Rodrigues, S., Dubhashi, N.G., Rodrigues, E., Banaulikar, S.S., Singh, R., Dash, A.P., Baird, J.K., 2009. Histopathology of fatal respiratory distress caused by Plasmodium vivax malaria. Am. J Trop. Med. Hyg. 81, 758–762. Vitor-Silva, S., Reyes-Lecca, R.C., Pinheiro, T.R., Lacerda, M.V., 2009. Malaria is associated with poor school performance in an endemic area of the Brazilian Amazon. Malar. J. 8, 230. WHO, 2011. World Malaria Report. World Health Organisation, Geneva. Wyler, D.J., 1983. Splenic functions in malaria. Lymphology 16, 121–127. Yeo, T.W., Lampah, D.A., Tjitra, E., Piera, K., Gitawati, R., Kenangalem, E., Price, R.N., Anstey, N.M., 2010. Greater endothelial activation, Weibel-Palade body release and host inflammatory response to Plasmodium vivax, compared with Plasmodium falciparum: a prospective study in Papua. Indonesia. J. Infect. Dis. 202, 109–112. Please cite this article in press as: Costa, F.T.M., et al. On the pathogenesis of Plasmodium vivax malaria: Perspectives from the Brazilian field. Int. J. Parasitol. (2012), http://dx.doi.org/10.1016/j.ijpara.2012.08.007
Download