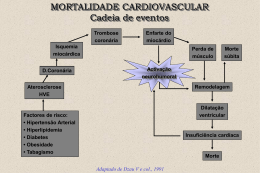
Impacto metabólico e estratégias para redução do risco cardiovascular em DP Roberto Pecoits-Filho Potential conflict of interest • Honoraria – Gambro, Altana, Baxter, Renal Research Institute, Roche, University of Missouri, Genzyme • Research Grants – CNPq, Fundação Araucária, Fundação Pro Renal, Baxter, Astra Zeneca, Amgen, Biogenerix, Genzyme • Consulting – Crescendo Medical Education (www.thekidney.org), Baxter, Roche, Genzyme Kramer HJ et al J Am Soc Nephrol 2006; 17:1453-9 Chan J, et al Nephrology Dialysis Transplantation 2007; 22(4):1100-1106 Increased innate immune response Deffective adaptive immune response Partialy corrected uremia Bone remodeling Insulin resistyance Metabolic syndrome Muscle catabolism Acute phase reactants adipocytokine production appetite REE Endothelial dysfunction Monocyte adhesion SMC proliferation LDL oxidation Hiperglicemia pós PD • Lameire et al – 5 casos de de novo diabetes mellitus em 310 pacientes não diabéticos entre 1979 and 1996 • Outras séries – de novo diabetes em 5% de pacientes Lameire N, et al. Clin Nephrol 1988; 30 (Suppl 1): S53-58. Kurtz SB, et al. Mayo Clin Proc 1983; 58: 633-639. New Onset Hyperglycemia in Non-Diabetic Chinese Patients Started on Peritoneal Dialysis • Glicemia de jejum (fasting after overnight dwell with 1.5% glucose) • 153 DM / 252 non-DM patients • Fasting plasma glucose – 126 - 200 mg/dL - 48 patients (19.0%) – >200mg/dl – 11 patients (4.4%) Szeto CC. Am J Kidney Dis 2007 Apr;49(4):524-32. Gordura corporal em PD Dexa CT scans, 12 pacientes incidentes Peso KG 67.1 68.4 ns % Gordura 27.8 30.9 ns Gordura abdominal (cm2) 130.1 159.7 P<0.02 Fernstrom at al PDI, Vol 18, pp. 166-171, 1998 Disturbances of carbohydrate metabolism in non-diabetic PD patients Fasting glucose (mg/dL) HbA1C (%) HbA1c > 7% (%) HOMA in dex Fibrinogen (mg/d L) PD 9016 6.10.8 6 3.33.2 582183 HD 8114 5.40.5 0 2.12.0 452183 p value <0.005 <0.0001 <0.005 <0.05 <0.001 Fortes et al. ISPD Hong Kong 2006 Metabolic Syndrome and Dialysis % Fortes et al. ASN 2006 Changes in membrane structure and function with time on PD Solute Transport (D/P creat) 0.75 0.7 0.65 0.6 1 6 12 18 24 30 36 42 48 54 60 Months on Peritoneal Dialysis Davies et al, KI, 1998 and Peritoneal Biopsy Registry® Increased vascular area in experimental diabetes De Vriese et al. JASN 2001; 12 1734-41 Problemas metabólicos aumentam nos alto transportadores Reabsorção de glicose Obesidade Dislipidemia Resistência insulínica Aumento da perda proteica Hipoalbuminemia Perda da capacidade antioxidante Edema Falha de UF Sobrecarga de volume Inflamação Aumento de mortalidade % Patient Survival ADEMEX : Diabetes Mellitus p=0.3237 p=0.7203 Months on Study Fasting blood glucose predicts survival in PD patients 1.0 FBS < 100 mg/dL 0.9 actuarial survival FBS 100 to 126 mg/dL FBS > 126 mg/dL 0.8 0.7 pre-existing diabetes 0.6 univariate Cox regression, p = 0.020 0.5 0 6 12 18 24 30 36 follow up (months) Szeto CC. Am J Kidney Dis 2007 Apr;49(4):524-32. PD HD BMI≥30 BMI≥30 BMI<30 BMI<30 Abbott KG et alKidney Int 2004; 65:597-605 Obesidade reduz a sobrevida de pacientes em PD P<0.001 <20 N=9769 Obesity HR 1.35 20-24.9 >30 25-29.9 McDonald SP et al J Am Soc Nephrol 2003; 14: 2894-901 Diferenças da relação entre mortalidade e obesidade: PD e HD • Em diálise peritoneal – a obesidade está relacionada a risco de complicações de cateter e infecções – Mais frequentemente relacionada a acúmulo de gordura no abdomen – Mais frequentemente associada a distúrbios metabólicos P = 0.005 Morioka et al: Diabetes Care 24: 909-913, 2001 Wu et al: NDT 12: 2105-10, 1997 Programas de redução de peso em PD • 11 pacientes com mais de 25 de IMC • Equipe multidisciplinar – Refeições planejadas – Programa de exercícios – Otimização de prescrição Hollis J et al Perit Dial Int 25(Suppl 3): S152-4, 2005 Weight reduction program in PD N=8 0 mo 12 mo P value Weight (kg) 94.6 89.5 0.017 Energy intake (kcal/d) 1824 1208 0.012 PD energy (kcal/d) 350 339 NS PD volume (L/d) 8.75 10.75 NS Kt/V 2.26 2.28 NS % Body fat 41.2 40.2 NS Hollis J et al Perit Dial Int 25(Suppl 3): S152-4, 2005 Volume 17, 2001 Substitution of one glucose exchange with icodextrin results in a significant fall in HbA1c HbA1c % * P <0.05 9.5 9 8.5 8 7.5 7 6.5 6 5.5 5 * Prospective, open label study of 17 PD patients with symptomatic fluid overload A subset of 12 insulin treated diabetic APD and CAPD patients 8.9 7.9 Baseline Glucose Substitution of one 4.25% for Extraneal. All other exchanges remained the same 1 month post Icodextrin Icodextrin Adapted from Johnson DW et al Icodextrin as salvage therapy in peritoneal dialysis patients with refractory fluid overload BMC Nephrology 2001,2 :2 Results Insulin dose Insulin dose (U/d) 10 GLU ICO 5 * p<0.05 ICO vs GLU +p<0.01 ICO vs GLU 0 -5 * * -10 * + + + + + + + -15 0 3 6 Months 9 12 Results Blood glucose Fasting serum Glucose (mg/dL) 100 GLU 75 ICO 50 * p<0.05 ICO vs GLU 25 0 -25 * -50 * -75 -100 0 3 6 Months Mean±EEM *p<0.05; ** p<0.03; *** p<0.01 vs Control ‡p<0.05; ‡ ‡ p<0.03; ‡ ‡ ‡ p<0.01 vs Basal 9 12 Results Hb a1c (%) Glycated hemoglobin 2.0 1.5 1.0 0.5 0.0 -0.5 -1.0 -1.5 -2.0 -2.5 GLU ICO * p<0.05 ICO vs GLU +p<0.01 ICO vs GLU * + 0 3 6 Months Mean±EEM *p<0.05; ** p<0.03; *** p<0.01 vs Control ‡p<0.05; ‡ ‡ p<0.03; ‡ ‡ ‡ p<0.01 vs Basal + * 9 12 Results Serum Triglycerides (mg/dL) Triglycerides 100 GLU 50 ICO 0 * p<0.05 ICO vs GLU +p<0.01 ICO vs GLU -50 + -100 + -150 -200 0 3 6 Months Mean±EEM *p<0.05; ** p<0.03; *** p<0.01 vs Control ‡p<0.05; ‡ ‡ p<0.03; ‡ ‡ ‡ p<0.01 vs Basal 9 12 Results Survival 100 Percent survival GLU ICO 90 80 70 60 log-rank test p<0.01 50 0 3 6 9 Time Mean±EEM *p<0.05; ** p<0.03; *** p<0.01 vs Control ‡p<0.05; ‡ ‡ p<0.03; ‡ ‡ ‡ p<0.01 vs Basal 12 15 PPPP DDDD NEPP Marshall J et al. Kidney Int 2003; 64: 1480-1486 4D Study Wanner C et al N Engl J Med 2005; 353(3):238-48 AURORA Fellstrom B et al. N Engl J Med 2009;10.1056/NEJMoa0810177 Paciente DRC/ HD / DP Cada 6 meses: •Colesterol •TG •HDL, LDL Cada 6 meses: •Colesterol Total •TG •HDL, LDL Sem perfil patológico •Colesterol •TG •HDL, LDL •Enzimas hepaticas Perfil patológico •TG>180mg% •LDL>100mg% •HDL<40mg% Hiperlipidemia combinada estatinas Metat: LDL<1oomg% Não combine!! Hipertligiceridemia Gemfibrozil Meta:: TG<180mg% NDT 2000: Vol 15, Suppl. 5 Martens FM, et al. Drugs 2002; 62: 1463-1480. 24 wks Randomized 52 DM with Stable glycemic control on insulin on PD Insulin + Add on RSZ 4mg daily Insulin alone Wong et al. Am J Kidney Dis 2005 Oct;46(4):713-9 Improve Insulin Resistance Percentage reduction in insulin dosage was markedly more significant in RSZ group than control group [-21% vs -0.5%] Wong TY, …, Li PKT. Am J Kidney Dis 2005 Oct;46(4):713-9 Change in hsCRP 14 p = 0.01 p = 0.03 serum CRP (mg/L) 12 10 8 6 4 2 0 TZD CTL 0 week TZD CTL 24 week Wong TY, …, Li PKT. Am J Kidney Dis 2005 Oct;46(4):713-9 LANDMARK Longitudinal Assessment of Numerous Discrete Modifications of Atherosclerotic Risk factors in Kidney disease (N=200) (49 PD, 78 HD, 73 pre-dialysis) Isbel NM et al Am Heart J 2006; 151(3):745-53 LANDMARK Trial Parameter Usual Care Focused Care Visits 2 Monthly Monthly Smoking Usual Psych, QUIT Lipids TC<5.5, TC<4, LDL<2, LDL<3 TG<2 Hcy No Target Hcy<15 BP <140/90 160/90 Hb 10-12.5 11-12.5 Pi <1.8 <1.6 PTH 2-3 x N 2-3 x N HbA1C No Target <8% Aspirin Clinical Indicn All Patients Isbel NM et al Am Heart J 2006; 151(3):745-53 1.00 v e n t f r e e s u r v i v a l b y r a n d o m i z a t i o n g r o u p 0.50 0.75 E 0.00 0.25 Usual Care Vs Focus Care 0 5 10 15 Survival (months of follow up) randomis = 1 20 25 randomis = 2 Isbel NM et al Am Heart J 2006; 151(3):745-53 HD vs. PD in DM USRDS Mortality 1987-2005 Second Year First year Third year Courtesy Dr. Heaf Conclusões • Alterações do metabolismo de glicose e lípides são comuns em DRC • Absorção de glicose piora os distúrbios em DP, particularmente em alto transportadores • Intervenções são eficazes • Redução na mortalidade ainda precisa ser demonstrada
Download