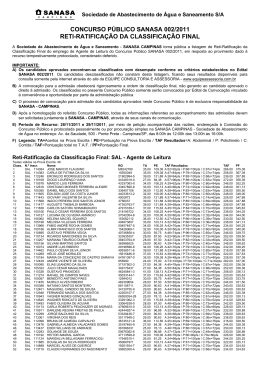
Congresso SBHCI - 2014 Julho, Porto Alegre-RS Terapia antiplaquetária dupla após o implante de SF contemporâneos: onde estamos? Fausto Feres São Paulo- Brazil Instituto Dante Pazzanese de Cardiologia Terapêutica Antiplaquetária Dupla após SF contemporâneo n How did we get to 12 months in the first place? DAPT with first generation DES § § § § § Bare metal stents – one month FIM 1999 (Cypher, sirolimus) – two months RAVEL 2002 (Cypher, sirolimus) – three months SIRIUS 2003 (Cypher, sirolimus) – three months TAXUS IV 2004 (Taxus, paclitaxel) – six months Up to 2006: Smith SC, et al. J Am Coll Cardiol. 2006;47:216-35 Late and Very Late Stent Thrombosis: A “New” Phenomenon Feres F et al. Catheter Cardiovasc Interv. 2006; 68:83-88 A New Mechanism Late Acquired Incomplete Stent Apposition Cypher SES 1216 days pos procedure Taxus PES 331 days pos procedure Feres F et al. Catheter Cardiovasc Interv. 2006; 68:83-88 2007 Updated Guideline King SB, et al. J Am Coll Cardiol. 2008;51:172-209 Guidelines: US & EUROPE Levine GN. Circulation 2011;124:e574-e651 Wijns W. European Heart Journal 2013 Terapêutica Antiplaquetária Dupla após SF contemporâneo n How did we get to 12 months in the first place? n Limitations of prolonged DAPT Limitations of prolonged DAPT • Cost • Convenience • Bleeding Limitations of prolonged DAPT • Cost • Convenience • Bleeding PLATO: Major Bleeding 5.5%- 1st month 15 Major Bleeding PLATO Criteria (%) Ticagrelor 11.6% Clopidogrel 11.2% 10 5 P=0,43 HR: 1,04 ( IC 95%, 0,95–1,13) 0 0 60 120 180 240 300 360 Days after 1st dose No Ticagrelor 9.235 7.246 6.826 6.545 5.129 3.783 3.433 Clopidogrel 9.186 7.305 6.930 6.670 5.209 3.841 3.479 Ambos os grupos incluiram AAS Wallentin L, et al. N Engl J Med. 2009;361:1045–1057. P=NS Scottish Coronary Revascularization Registry 17.797 Stented Pts 2003 - 2007 Non-Cardiac Surgery 1953 pts (11%) BMS 1383 DES 570 4.4% within 1st year ORTHO COSMETIC DIGEST VASCULAR Gruden NLM Circ Cardiovasc Interv. 2010;3:236-42 33% 19% 16% 10% Terapêutica Antiplaquetária Dupla após SF contemporâneo n How did we get to 12 months in the first place? n Limitations of prolonged DAPT n Does the DES type make a difference? Does the DES type make a difference? Raber, L. et al. Circulation 2012 Terapêutica Antiplaquetária Dupla após SF contemporâneo n How did we get to 12 months in the first place? n Limitations of prolonged DAPT n Does the DES type make a difference? n What is the current evidence for shorter DAPT? Scientific Evidence Early Discontinuation DAPT post DES Randomized Trials EXCELLENT PRODIGY RESET OPTIMIZE Registries Metanalysis Everolimus (Xience V) 4 Randomized Trials Zotarolimus (Resolute) Scientific Evidences Early Discontinuation DAPT post DES Randomized Trials EXCELLENT PRODIGY RESET OPTIMIZE Registries Metanalysis Everolimus (Xience V) 4 Randomized Trials Zotarolimus (Resolute) EXCELLENT EXCELLENT: DAPT- 6 vs 12 m 1.443 pacientes tratados com SF de 1ª vs. 2ª gerações EP 1ário: morte cardíaca, IAM e revascularização do vaso-alvo Gwon et al. Circulation 2012;125:505-513 PRODIGY Trial : DAPT 6 vs 24 m Valgimigli al. Circulation 2012;125:2015-2026 PRODIGY: DAPT 6 vs 24 m ~2.000 pts randomized (1:1), 75% ACS 4 stent types (1:1:1:1) – BMS & DES 1ª e 2ª generation 10.1% vs. 10.0% EP 1ário: morte, IAM, AVE Valgimigli al. Circulation 2012;125:2015-2026 RESET Trial Kim et al. J Am Coll Cardiol 2012;60:1340-1348 RESET: DAPT 3 vs 12 m Cardiac Death, AMI, ST, TVR and Bleeding Kim et al. J Am Coll Cardiol 2012;60:1340-1348 OPTIMIZE F Feres and coauthors for the OPTIMIZE Trial Investigators" " Three vs Twelve Months of Dual Antiplatelet Therapy After Zotarolimus-Eluting Stents: The OPTIMIZE Randomized Trial" " Published online October 31, 2013! " " Available jama.com and Availableatat jama.com mobile.jamanetwork.com! mobile jamanetwork.com " " jamanetwork.com OPTIMIZE: A Prospective, Randomized Trial of 3 Months Versus 12 Months of Dual Antiplatelet Therapy with the Endeavor Zotarolimus-Eluting Stent • Fausto Feres, MD, PhD • On behalf of the OPTIMIZE Trial Investigators • Instituto Dante Pazzanese de Cardiologia • São Paulo, Brazil 33 Clinical Sites in Brazil n: 3119 pts Dr. Fausto Feres (624pts) Dr. Roberto Botelho (180pts) Dr. João Eduardo Tinoco (446pt) Dr. Décio Salvadori Jr. (166pts) Dr. José A. Mangione (280pts) Dr. Marcos Gusmão (160pts) Dr. Hélio Castello Junior (135pts) Dr. Eduardo Nicolela Jr. (125pts) Dr. Marco Perin (117pts) Dr. Fernando Devito (106pts) Dr. J. Antônio Marin-Neto (100pts) Dr. George Meireles (91pts) Dr. André Labrunie / Dr. Marden Tebet (70pts) Dr. Nelson Moura de Araújo (58pts) Dr. Andrés Sanchez (55pts) Dr. Sérgio Berti (52pts) Dr. Pablo Teixeirense (49pts) Dr. Adrian Kormann (41pts) Dr. Rone Padilha (40pts) Dr. Rogério Sarmento Leite (35pts) Dr. Augusto Lima Filho e Dr. André Lima (32pts) Dr. Marcio A. dos Santos (24pts) Dr. Helman Martins (24pts) Dr. Gilberto Nunes (21pts) Dr. Paulo Marra da Motta (21pts) Dr. Heloísa Guimarães (17pts) Dr. Luiz E. São Thiago (15pts) Dr. Paulo Caramori (13pts) Dr. Alexandre Zago (9pts) Dr. Jamil A. Saad (6pts) Dr. Edmur Araújo (5pts) Dr. Ari Mandil (2pts) 1st Investigator Meeting November/2009 Primary Endpoint: NACCE at 1 Year (All-Cause Death, MI, Stroke, Major Bleeding) Cumulative Incidence of NACCE (%) 15 12M DAPT No. at risk No. events No. at risk No. events Non-inferiority P-value = 0.002 10 Log-Rank P = 0.84 HR 1.03 (0.77 – 1.38) 6.0 5.8 5 0 Month 3M DAPT 0 3 6 9 Time After Initial Procedure (Months) 12 0 1 3 6 12 1563 18 1556 16 1520 25 1514 25 1504 11 1497 11 1468 18 1466 16 1384 21 1381 22 Landmark at 3M: NACCE (All-Cause Death, MI, Stroke, Major Bleeding) Incidence of NACCE (%) 15 12M DAPT P = 0.86 HR 1.03 (0.71 – 1.51) 10 5 0 Month No. at risk No. events No. at risk No. events 3M DAPT P = 0.91 HR 1.03 (0.66 – 1.60) 3.5 3.3 0 0 1563 18 1556 16 2.6 2.6 3 6 9 Time After Initial Procedure (Months) 1 1520 25 1514 25 3 1504 11 1497 11 6 1468 18 1466 16 12 12 1384 21 1381 22 Stent Thrombosis vs. Bleeding ARC Def./Prob. Stent Thrombosis Any Bleeding* 10 10 Incidence (%) 3M DAPT 12M DAPT P = 0.64 HR 0.81 (0.34-1.96) 5 P = 0.18 HR 3.97 (0.44-35.49) P = 0.78 HR 0.93 (0.56-1.54) 5 0.7 0.6 3 6 9 No at risk 1.0 0.4 0 12 0 3 Time After Initial Procedure (months) Month P = 0.07 HR 0.43 (0.16-1.11) 2.0 1.9 0.3 0.1 0 0 3M DAPT 12M DAPT 6 9 12 Time After Initial Procedure (months) 0 1 3 6 12 1563 1555 1540 1506 1505 Month No at risk 0 1 3 6 12 1563 1538 1516 1482 1439 No events 0 6 3 4 0 No events 4 15 10 4 2 No at risk 1556 1541 1525 1501 1500 No at risk 1556 1528 1501 1472 1387 No events 5 3 3 1 0 No events 11 8 12 6 8 *Any bleeding according to the combined REPLACE-2 and GUSTO criteria. Scientific Evidences Early Discontinuation DAPT post DES Randomized Trials EXCELLENT PRODIGY RESET OPTIMIZE Registries Metanalysis Everolimus (Xience V) 4 Randomized Trials Zotarolimus (Resolute) Everolimus (Xience V) Taxa de TS até 12 meses, % Análise post-hoc envolvendo ~10.615 pacientes incluídos nos estudos SPIRIT V and Women, and Xience V USA and India4 (mundo real), avaliando TS def./prov. (ARC) 4 SEM interrupção de TAD COM interrupção de TAD 3 2 1 1,64 1,63 0,68 0,68 0,21 0 0-3 Meses 0,29 0,2 0 3-12 Meses 0-1 Mês Palmerini T. at TCT 2012, Miami, EUA 1-12 Meses Zotarolimus (Resolute) Taxa de TS até 12 meses, % Análise post-hoc envolvendo ~5.000 pacientes incluídos nos estudos RESOLUTE All-Comers, International, US e Japão (30% diabéticos), avaliando TS def./prov. (ARC) 4 SEM interrupção de TAD COM interrupção de TAD 2,96 3 1,92 2 1 0,78 0,67 0,1 0 0-3 Meses 0,21 0 3-12 Meses 0-1 Mês Bhatt D. at TCT 2013, San Francisco, EUA 0 1-12 Meses Scientific Evidences Early Discontinuation DAPT post DES Randomized Trials EXCELLENT PRODIGY RESET OPTIMIZE Registries Metanalysis Everolimus (Xience V) 4 Randomized Trials Zotarolimus (Resolute) Terapêutica Antiplaquetária Dupla após SF contemporâneo • Recent studies are consistent that shorter DAPT duration post 2nd generation DES might not always require 12 months DAPT to reduce the risk of adverse thrombotic events. • These outcomes may be especially relevant for patients who are at high risk of bleeding complications following PCI, such as the elderly and patients with a history of hemorrhagic events, who might need to stop DAPT earlier.
Download