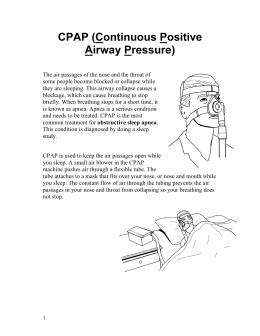
Manejo peri-operatório dos pacientes com SAHOS V Curso Nacional de Ventilação Mecânica II Curso Nacional de Sono 22 a 24 de março de 2012 Realização - SBPT MEDICINA DO SONO HOSPITAL SÍRIO LIBANÊS NÚCLEO AVANÇADO DE TÓRAX (NAT) – HSL PNEUMOLOGIA EPM - UNIFESP Maurício C. Bagnato Síndrome da Hipoventilação-Obesidade - SHO Síndrome da Hipoventilação-Obesidade - SHO Piper 0 A. J. Sleep Med Rews 2010 Síndrome da Hipoventilação-Obesidade - SHO Upper Airway Management of the Adult Patient with Obstructive Sleep Apnea in the Perioperative Period Avoiding Complications. Clinical Practice Review Committee - American Academy of Sleep Medicine SLEEP 2003;26(8):1060-5. Fatores que contribuem para o risco peri-operatório • ↑ Instabilidade de VVAASS devido a anestésicos e analgésicos narcóticos • Efeitos cardiopulmonares devido a SAHOS • ↓ Capacidade residual funcional e reserva oxigenação no obeso • ↓ do “drive” ventilatório devido a agentes anestésicos Upper Airway Management of the Adult Patient with Obstructive Sleep Apnea in the Perioperative Period - Avoiding Complications. Clinical Practice Review Committee - American Academy of Sleep Medicine SLEEP 2003;26(8):1060-5. SAHOS (PSG no prontuário / CPAP ideal / doença residual (↑peso) / CPAP pré e POI S/ diag SAHOS (Hist / EF / menop / acompanhante / questionário / obeso ou não / CPAP empírico no POI se urgência – aceitação?, auto-CPAP? ) Entubação preparo (drogas anti-refluxo e antisilogogas? / pré-oxigenação / masc laríngea? Entubação (s/n fibr óptica / se insucesso – masc, obturador esof,, jet vent transtr s/n traqueo) Anestésico (c/ ou s/ sedação? – melhor sem – geral / se possível bloq regional / epidural? Extubação (perder control VVAA / edema pulmonar / tônus musc adeq / dec elevado apenas? – CPAP POI (primeiras 24hs críticas – UTI / rebote REM / analgesia cautelosa / sinergismo / co- morbidades / PCA c/ limite / Oximetria e Fc c/ alarmes / CPAP adequado se rc ↑ pressão Obstructive Sleep-Related Breathing Disorders in Patients Evaluated for Bariatric Surgery Obesity Surgery, 13, 2003 Summary The incidence of OSRBD in our bariatric study population was very high. Cardiovascular consequences of OSRBD are well documented. These consequences may be increased in the postoperative period when the combination of REM rebound and narcotic analgesia increase oxyhemoglobin desaturations. Health-care providers evaluating patients for bariatric surgery should consider referral for a sleep Obstructive Sleep-Related Breathing Disorders in Patients Evaluated for Bariatric Surgery Obesity Surgery, 13, 2003 Evaluation and PSG as part of the preoperative evaluation.Clinical evaluation with BMI, Epworth Sleepiness Scale and the Mallampati airway classificationfailed to predict the severity of OSRBD. Therapy for OSRBD should be initiated prior to surgeryto minimize the hemodynamic complications of OSRBD and to familiarize the patient with CPAP. Patients should be educated about the importance of CPAP use to correct OSRBD. Continued use of CPAP in the postoperative period will theoretically decrease the potential morbidity and mortality of OSRBD in the hospital and after discharge from the hospital. Evidence Supporting Routine Polysomnography Before Bariatric Surgery Obesity Surgery, 14, 23-26, 2004 Conclusions: In this large patient cohort, sleep apnea was prevalent (77%) independent of BMI, and most cases were not diagnosed before bariatric surgical consultation. These data support the use of routine screening polysomnography before bariatric surgery. Postoperative Complications in Patients With Obstructive Sleep Apnea Syndrome Undergoing Hip or Knee Replacement: A Case-Control Study Mayo Foundation for Medical Education and Research Volume 76(9), September 2001, pp 897-905 CONCLUSIONS In this study, we have shown that the presence of OSAS in patients undergoing elective hip replacement or knee replacement is associated with a considerable number of complications in the postoperative period. Almost one third of the patients with OSAS in our study suffered a substantial respiratory or cardiac complication. Patients who were not using CPAP prior to hospitalization had a significantly higher incidence of serious complications. Patients diagnosed with OSAS have been shown to be heavy consumers of health care resources for several years prior to diagnosis and the utilization decreases after starting treatment in patients who adhere to the treatment. Postoperative Hypoxemia in Morbidly Obese Patients With and Without Obstructive Sleep Apnea Undergoing Laparoscopic Bariatric Surgery (Anesth Analg 2008;107:138 –43) CONCLUSIONS: In morbidly obese subjects, in the first 24 h after laparoscopic bariatric surgery, OSA does not seem to increase the risk of postoperative hypoxemia. Our data confirm that morbidly obese subjects, with or without OSA, experience frequent oxygen desaturation episodes postoperatively, despite supplemental oxygen therapy suggesting that perioperative management strategies in morbidly obese patients undergoing laparoscopic bariatric surgery should include measures to prevent postoperative hypoxemia. Identification of patients at risk for postoperative respiratory complications using a preoperative obstructive sleep apnea screening tool and postanesthesia care assessment. Department of Anesthesiology, Mayo Clinic, Rochester, Minnesota 55905, USA. [email protected] Anestthesiology 2009 Apr;110(4):869-77. CONCLUSIONS: Combination of an obstructive sleep apnea screening tool preoperatively (SACS) and recurrent PACU respiratory events was associated with a higher oxygen desaturation index and postoperative respiratory complications. A two-phase process to identify patients at higher risk for perioperative respiratory desaturations and complications may be useful to stratify and manage surgical patients postoperatively.
Baixar