RENORBIO
Programa de Pós-Graduação em Biotecnologia
Desenvolvimento de Nanosistemas Farmacêuticos para
Terapia Gênica
Lourna Mafra Verissimo
Natal – RN
2011
i
RENORBIO
Programa de Pós-Graduação em Biotecnologia
Desenvolvimento de Nanosistemas Farmacêuticos para
Terapia Gênica
Tese de Doutorado apresentada ao Programa de PósGraduação em Biotecnologia - PPG-B,
Área de concentração: Biotecnologia em Saúde
Lourena Mafra Verissimo
Orientador: Eryvaldo Sócrates Tabosa do Egito
Co-Orientadora: Lucymara Fassarela Agnez Lima
ii
LOURENA MAFRA VERISSIMO
Desenvolvimento de Nanosistemas Farmacêuticos para Terapia Gênica
Defesa de Tese apresentada a Rede Nordeste de Biotecnologia (RENORBIO) para obtenção
do título de Doutor em Biotecnologia.
Área de Concentração: Biotecnologia em Saúde
Aprovada em 14 de março de 2011 por:
Presidente: Prof. Dr. Eryvaldo Sócrates Tabosa do Egito
Rede Nordeste de Biotecnologia (RENORBIO)/ UFRN
_____________________________________
Vice-presidente: Prof a. Dr.a Lucymara Fassarela Agnez Lima
Rede Nordeste de Biotecnologia (RENORBIO)/ UFRN
____________________________________
1 Examinador: Prof. Dr. Elias Fattal
Université Paris Sud XI
____________________________________
2 Examinador: Prof. Dr. Helder Teixeira
Universidade Federal do Rio Grande do Sul
____________________________________
3 Examinador: Prof. Dr. Matheus Freitas
Universidade Federal do Rio Grande do Norte
____________________________________
4 Examinador: Profa. Dra. Selma Maria Bezerra Jeronimo
Rede Nordeste de Biotecnologia (RENORBIO)/ UFRN
____________________________________
iii
SUMÁRIO
1.0 INTRODUÇÃO.......................................................................................................... 2
2.0 REVISÃO DA LITERA TURA .................................................................................5
2.1 Terapia Gênica ..................................................................................................5
2.2 Vetores não virais ..............................................................................................7
2.2.1 Lipossomas....................................................................................................12
2.2.2 Nanoemulsões ............................................................................................. 15
3.0 REFERÊNCIAS BIBLIOGRÁFICAS.....................................................................22
4.0 ARTIGOS DERIVADOS DA TESE....................................................................... 30
4.1 PHARMACEUTICAL EMULSIONS: A NEW APPROACH FOR GENE
THERAPY ..................................................................................................................... 32
ABSTRACT.......................................................................................................... 33
INTRODUCTION..................................................................................................34
GENE DELIVERY SYSTEMS ........................................................................... 36
Viral vectors .........................................................................................................36
Nonviral vectors.................................................................................................... 37
The drawbacks of liposomes ................................................................................ 39
The use of pharmaceutical emulsions, nanoemulsions, and microemulsions .......41
CONCLUDING REMARKS .............................................................................. 45
REFERENCES................................................................................................................47
FIGURE 1.Cationic emulsion system acting as a carrier for DNA. ....................... 55
TABLESLIST .................................................................................................................56
TABLE 1.Some advantages and disadvantages of currently used vectors. ................…56
4.2 CATIONIC NANOEMULSIONS AS A POSSIBLE STRATEGY FOR GENE
DELIVERY
IN
THE
TREATMENT
OF
XERODERMA
PIGMENTOSUM:
PRELIMINARY STUDIES............................................................................................58
ABSTRACT ..........................................................................................................59
INTRODUCTION .................................................................................................60
MATERIALS AND METHODS ..........................................................................61
RESULTS AND DISCUSSION........................................................................... 63
CONCLUDING REMARKS ............................................................................... 67
REFERENCES ......................................................................................................68
TABLES LIST ......................................................................................................71
TABLE 1: Emulsions composition: Basic emulsion (BE), DOTAP containing
iv
emulsion (ED) and Stearylamine containing emulsion (ES). .........................................71
TABLE 2: Characterization of Basic Emulsion (BE), DOTAP Emulsion (ED) and
Stearylamine Emulsion (ES)...........................................................................................71
TABLE 3: Characterization of Stearylamine Emulsions incorporated in Aqueous
Phase (AP) or Oily (Phase).............................................................................................71
FIGURES LIST .....................................................................................................72
FIGURE 1.TEM micrographs of cationic nanoemulsions (A) DOTAP emulsion
and (B) SA emulsion.......................................................................................................72
FIGURE 2: Micro-emultocrit results showing creaming rate of nanoemulsions and
lipoplexes. .......................................................................................................................73
FIGURE 3: Agarose gel electrophoresis picture showing DNA compaction of ED
(A) and ES (B) nanoemulsions. ......................................................................................73
FIGURE 4: Agarose gel electrophoresis picture showing DNA compaction........74
(A) ES AP Nanoemulsions - Lane 1 shows the positive control: plasmid [0.46 μg] and
lane 10 shows the negative control: nanoemulsion. Lanes 2 to 9 show the follow ratios
of EC/DNA (nmol/μg): 25.81; 51.62; 64.53; 77.43; 90.34; 103.24; 116.15 and 129.05.
OC: Open circular form; SC: Supercoiled form.............................................................74
(B)
ES OP (B) nanoemulsions - Agarose gel electrophoresis picture showing DNA
compaction of ES OP. Lane 1 shows the positive control: plasmid [0,46μg] and lane 8
shows the negative control: nanoemulsion. Lanes 2 to 7 show the follow ratios of
EC/DNA (nmol/μg): 64.53; 77.43; 90.34; 103.24; 116.15 and 129.05. OC: Open
circular form; SC: Supercoiled form………….............................................................. 74
4.3
PHYSICOCHEMICAL AND IN VIVO EVALUATION OF LIPOSOMES
RECOVERED BY HYALURONIC ACID FOR TARGETING CD44 RECEPTOR OF
RETINAL CELLULES ................................................................................................. 76
INTRODUCTION................................................................................................. 77
MATERIALS AND METHODS.......................................................................... 78
RESULTS AND DISCUSSION........................................................................... 81
CONCLUSIONS................................................................................................... 83
REFERENCES...................................................................................................... 84
TABLE LEGENDS............................................................................................... 86
FIGURE LEGENDS............................................................................................. 87
5.0 CONSIDERAÇÕES FINAIS................................................................................... 91
6.0 ANEXO.................................................................................................................... 94
v
6.1 RESUMOS PUBLICADOS EM CONGRESSOS ......................................... 94
6.2 ARTIGO PUBLICADO NO JOURNAL OF DRUG TARGETING ............. 98
Keywords ............................................................................................................. 98
6.3 ARTIGO ACEITO NO THE AMERICAN JOURNAL OF PATHOLOGY
…………………………………………………………….......………………...109
MICROGLIA/MACROPHAGES
MIGRATE
THROUGH
RETINAL
EPITHELIUM BARRIER BY A TRANSCELLULAR ROUTE: INVOLVEMENT IN
DIABETIC RETINOPATHY - ROLE OF PKCΖ IN MICROGLIA/MACROPHAGES
TRAFFICKING DURING DIABETIC RETINOPATHY IN GOTO KAKIZAKI
RATS............................................................................................................................ 109
ABSTRACT........................................................................................................ 110
INTRODUCTION............................................................................................... 111
MATERIALS AND METHODS........................................................................ 112
Animals............................................................................................................... 112
Immunohistochemistry on cryostat ocular sections and on flat mounts of retina or
RPE/ choroids............................................................................................................... 112
Western Blotting analyses................................................................................... 114
Intravitreal injection of PKCζ specific inhibitor (PKCζi).................................. 114
Intravitreal injection of rhodamine-liposome (Rh-Lip)...................................... 115
Quantification of activated microglia/macrophages in the neuroretina.............. 115
Quantification of microglia/macrophages infiltrating the eye............................ 116
Quantification and criteria to identify transcellular pores................................... 116
Semi-thin and ultra-thin sections......................................................................... 116
Statistics.............................................................................................................. 116
RESULTS............................................................................................................ 117
Subretinal accumulation of microglia/macrophages and alteration of RPE in
diabetic rats after 12 months of hyperglycemia ........................................................... 117
Trans-epithelial pores are evidenced in RPE cells of diabetic rats..................... 117
The pores: a transcellular route for microglia/macrophages through the RPE... 118
Pores density in RPE from diabetic and non-diabetic rats.................................. 119
Intravitreal injection of the PKCζinhibitor in 12 months old diabetic rats
deactivated microglia/ macrophages, blocked their migration and impaired pore
formation….................................................................................................................. 119
DISCUSSION..................................................................................................... 120
vi
ACKNOWLEDGMENTS................................................................................... 124
REFERENCES.................................................................................................... 125
FIGURE LEGENDS........................................................................................... 128
TABLE 1. Weight and blood glucose concentration in normoglycemic controls
andhyperglycemic diabetic GK rats……..................................................................... 128
FIGURE 1. Microglia/macrophages accumulation in the subretinal space of 12
monthsold diabetic GK rats.......................................................................................... 128
FIGURE
2.
ICAM-1,
CAV-1
expression,
actin
recruitment
and
cell
invaginationstrongly suggest the presence of a transcellular pore in diabetic
RPE……………………………………....................................................................... 128
FIGURE 3. Involvement of PKCζin the pore formation.................................... 129
FIGURE 4. Transcellular migration of microglia/macrophages through RPE pores
………………………………………………………………………………………..129
FIGURE 5. Quantification of the number of pores in RPE cells and CAV-1,
ICAM- 1,PKCζ expression in the time course of diabetes........................................... 130
FIGURE 6. Effects of PKCζinhibition on microglia/macrophages retinal
infiltrationand on the pore density ............................................................................... 131
FIGURE 7. Effects of PKCζon microglia/macrophages activation ................ 131
vii
LISTA DE ABREVIATURAS E SIGLAS
ADA: Adenosine desaminase
ADN: Áácido desoxiribonucléico
AH: Ácido hialurônico
ARVO: Association for Research in Vision and Ophthalmology
CAV-1: caveolin-1
CI: Creaming Index
COX2: Cyclo-oxygenase 2
CTAB: Cetyltrimethylammonium bromide
DC-Chol: 3ß-[N-(N',N'-Dimetilaminoetano)-carbamoil]Colesterol
DOGS: 1,2-Dioleil-sn-Glicerol-3-{[ácido imidoacético N- (5-Amino-1-Carboxipentil)]
Succinato}
DOPE: Dioleilfosfatidiletanolamina
DOTAP: N-[1-(2,3-Dioleoiloxi)propil]-N,N,Ntrimetilamonio metilsulfato
DOTMA: (2,3-bis(oleyl)oxipropyl-trimethylammonium chloride)
DSPC: 1,2-diestearoil-sn-glicerol-3-fosfatidilcolina
DSPEPEG: Fosfatidiletanolamina-N-monometoxi-[PEG]
EA: Estearilamina
ED: DOTAP containing emulsion
ES AP: Aqueous phase stearylamine containing emulsion
ES OP: Oily phase stearylamine containing emulsion
ES: Stearylamine containing emulsion
EtBr: Ethidium bromide
GCL: Ganglion cell layer
GK: Goto Kakizaki
HA-DOPE: Ácido Hialurônico – DOPE
INL: Inner retinal layers
iNOS: Inducible nitric oxide synthase
NAN: Nucleic acid containing nanoparticles
NER: Nucleotide excision repair
OCT: Optimal cutting-temperature
OMS: Organização Mundial de Saúde
ONL: Outer nuclear cell layer
viii
OPL: Outer plexiform layer
OS: Outer segments of photoreceptors
PC: Fosfatidilcolina
PE: Fosfatidiletanlamina
PEG: Polietilenoglicol
PEI: poly(ethylenimine)
PE-Rodamina: Rodaminafosfatidiletanolamine
PI: Polidispersion Index
PKCζ: Protein kinase Cζ
PLL: poly(L-lysine)
Rh-Lip: Rhodamine-liposomes
RNA: Ribonucleic Acid
RPE: Retinal pigment epithelium
SA: Stearylamine containing emulsion
SCID: Severe Combined Immunodeficiency Disease
siRNA: RNA de interferência
TEM: Transmission electron microscopy
TNF-α: Tumor necrosis factor α
VAA: Vírus adenoassociados
XP: Xeroderma Pigmentosum
ZO1: Zonula-occludens-1
ix
AGRADECIMENTOS
Agradeço a Deus, sempre presente na minha vida dando a força necessária para
superar todos os obstáculos.
Agradeço aos meus orientadores, Prof. Dr. Eryvaldo Sócrates Tabosa do Egito e
Elias Fatal e as minhas co-orientadoras Profa. Dra. Lucymara Fassarela Agnez Lima e
Profa. Dra. Amelie Bochot pela oportunidade, confiança, exemplo e, sobretudo pela
amizade. Obrigada.
Ao Laboratório de Sistemas Dispersos (LASID) e ao Laboratório de Biologia
Molecular e Genômica (LBMG) da Universidade Federal do Rio Grande do Norte, onde
foi desenvolvido este trabalho, especialmente aos alunos de iniciação científica André
Leandro Silva e Francisco Alexandrino Júnior, pela importante colaboração durante o
curso deste trabalho, e pela amizade.
A Université Paris Sud XI, onde desenvolvi em estágio doutoral minha
capacidade de adaptação a outros ambientes de trabalho e capacidade de aprendizado.
As minhas companheiras de Bureau na Faculté de Pharmacie em Chatenay
Malabry: Amelie, Simona, Odille e Marion, que de alguma forma contribuíram para a
conclusão deste trabalho.
Ao Laboratório de Cerâmicas e Materiais Especiais (Departamento de Física);
ao Laboratório de Membranas e Colóides, ao Laboratório de Tecnologia de Tensoativos
(Departamento de Química) e ao Laboratório Glicosaminoglicanos II (Departamento de
Bioquímica), todos da Universidade Federal do Rio Grande do Norte, pela colaboração.
Aos meus amigos do LASID e LBMG, por toda colaboração e amizade; e aos
colegas e amigos de pós-graduação pelos vários momentos compartilhados, convívio e
amizade.
À Jussier Lourenço e aos meus amigos natalenses, pela paciência, apoio e
contribuição durante boa parte do período de desenvolvimento deste trabalho.
À minha família da Maison du Brésil pelos momentos de descontração e de
amizade desfrutados durante todo o ano de 2010, em especial a Vânia Oliveira, Eliana
Kuster, Gladson Dalmonech, Alex Leite, Helena Stigger, Fernanda Bruxel, Ana Pernas,
Isabela Gasparini, Estael Pereira, Paulo da Costa, Ramon e Fabiana Rached.
Aos meus irmãos parisienses, Gyselle Holanda, Francelyne Reinauld, Carlille
Campos e Amanda Andriola, pelos vários momentos de apoio e amizade e por estarem
ao meu lado sempre que necessário.
x
À minha família, especialmente avós, irmãos e sobrinhos, pelo companheirismo
e compreensão pelas minhas ausências em várias ocasiões.
Aos meus pais, Maria das Graças e Francisco Veríssimo, pelo carinho, apoio e
compreensão em todos os momentos.
xi
RESUMO
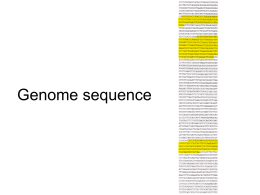
A terapia gênica é um dos maiores desafios propostos pela pesquisa pós-genômica e se
baseia na transferência de material genético a uma célula, tecido ou órgão com o intuito
de curar ou melhorar o estado clínico do paciente. Em sua forma mais simples, a terapia
gênica consiste na inserção de genes funcionais em células com genes defeituosos
objetivando substituir, complementar ou inibir esses genes causadores de doenças. Para
que o DNA exógeno seja expresso em uma população celular faz-se necessária a sua
transferência até o local de ação. Assim, é necessário criar veículos, que transportem e
protejam o DNA até que este chegue a uma população celular alvo. Os obstáculos
encontrados com a utilização de vetores virais têm proporcionado o interesse no
desenvolvimento de vetores não-virais, por serem fáceis de produzir, apresentarem
estabilidade controlável e facilitarem a transfecção gênica. O objetivo deste trabalho foi
avaliar dois diferentes vetores não virais, lipossomas e nanoemulsões catiônicos, e sua
possível utilização na terapia gênica. Para isso, foram utilizados lipídeos catiônicos e
co-tensoativos na produção dos dois sistemas. As nanoemulsões foram produzidas pelo
método de sonicação e compostas por Captex® 355; Tween® 80; Spam® 80; lipídeo
catiônico, Estearilamina (EA) ou N-[1-(2,3-Dioleoiloxi)propil]-N,N,Ntrimetilamonio
metilsulfato (DOTAP); e água ultra-pura (Milli-Q®). Estes sistemas foram
caracterizados quanto ao tamanho médio de gotícula, índice de polidispersão (PI) e
potencial zeta. Avaliou-se ainda a estabilidade dos sistemas e suas capacidades de
compactação do material genético. Os lipossomas foram preparados a partir do método
de hidratação do filme e compostos por DOTAP, Dioleilfosfatidiletanolamina (DOPE),
na presença ou ausência de Rodaminafosfatidiletanolamina (PE-Rodamina) e do
conjugado Ácido Hialurônico – DOPE (HA-DOPE). Estes sistemas foram
caracterizados da mesma forma que as nanoemulsões e também foram avaliados
estabilidade, influência do tempo, tamanho de material genético e presença ou ausência
de endotoxinas na formação dos lipoplexos. Os resultados obtidos permitem afirmar que
os sistemas são promissores para posterior utilização na terapia gênica e que esta área
promete ser uma área fértil de pesquisa científica e clínica por muitos anos, e
provavelmente se tornará uma prática clínica importante neste século. No entanto, da
possibilidade à prática existe um longo caminho a percorrer.
Palavras chaves: Terapia gênica, vetores não-virais, lipídeos catiônicos, nanoemulsões,
lipossomas.
xii
ABSTRACT
Gene therapy is one of the major challenges of the post-genomic research and it is based
on the transfer of genetic material into a cell, tissue or organ in order to cure or improve
the patient’s clinical status. In general, gene therapy consists in the insertion of
functional genes aiming substitute, complement or inhibit defective genes. The
achievement of a foreigner DNA expression into a population of cells requires its
transfer to the target. Therefore, a key issue is to create systems, vectors, able to transfer
and protect the DNA until it reaches the target. The disadvantages related to the use of
viral vectors have encouraged efforts to develop emulsions as non-viral vectors. In fact,
they are easy to produce, present suitable stability and enable transfection. The aim of
this work was to evaluate two different non-viral vectors, cationic liposomes and
nanoemulsions, and the possibility of their use in gene therapy. For the two systems,
cationic lipids and helper lipids were used. Nanoemulsions were prepared using
sonication method and were composed of Captex® 355; Tween® 80; Spam® 80; cationic
lipid, Stearylamine (SA) or 1,2-dioleoyl-3-trimethylammoniumpropane (DOTAP) and
water (Milli-Q®). These systems were characterized by average droplet size,
Polidispersion Index (PI) and Zeta Potential. The stability of the systems; as well as the
DNA compaction capacity; their cytotoxicity and the cytotoxicity of the isolated
components; and their transfection capacity; were also evaluated. Liposomes were
made by hydration film method and were composed of DOTAP; 1,2-dioleoyl-snglycero-3-phosphoethanolamine
(DOPE),
containing
or
not
Rhodaminephosphatidylethanolamine (PE- Rhodamine) and the conjugate Hyaluronic
Acid – DOPE (HA-DOPE). These systems were also characterized as nanoemulsions.
Stability of the systems and the influence of time, size of plasmid and presence or
absence of endotoxin in the formation of lipoplexes were also analyzed. Besides, the
ophthalmic biodistribution of PE-Rhodamine containing liposomes was studied after
intravitreal injection. The obtained results show that these systems are promising nonviral vector for further utilization in gene therapy and that this field seems to be very
important in the clinical practice in this century. However, from the possibility to the
practice, there is still a long way.
Key words: Gene therapy, non-viral vectors, cationic lipids, nanoemulsions, liposomes.
xiii
______________________________
Capítulo 1
Introdução
______________________________
INTRODUÇÃO
1.0 INTRODUÇÃO
A terapia gênica baseia-se no tratamento de doenças pela transferência do material
genético a uma célula, tecido ou órgão com o intuito de curar ou melhorar o estado
clínico do paciente. Em sua forma mais simples, a terapia gênica consiste na inserção de
genes funcionais em células com genes defeituosos objetivando substituir,
complementar ou inibir esses genes causadores de doenças (Verma e Weitzman, 2005).
Para que o ácido desoxiribonucléico (ADN) exógeno seja expresso em uma população
celular faz-se necessária a sua transferência até o local de ação. Assim, é necessário
criar veículos, que transportem e protejam o ADN até que este chegue a uma população
celular alvo. O que ainda é um desafio para a ciência (Brown, Schatzlein et al., 2001).
Os obstáculos encontrados com a utilização de vetores virais têm proporcionado o
interesse no desenvolvimento de vetores não-virais, por serem fáceis de produzir em
quantidade e reprodutibilidade aceitáveis, apresentando baixa imunogenicidade,
estabilidade controlável e baixo custo (Davis, 2002). As duas principais formas de
desenvolvimento de vetores não virais para terapia gênica consistem na associação de
lipídeos catiônicos ou polímeros catiônicos aos ácidos nucléicos, formando
respectivamente, lipoplexos ou poliplexos (Hengge, 2005). Apesar do grande número de
pesquisas relacionadas ao desenvolvimento destes vetores, existem vários problemas
associados a eles, sobretudo com relação à baixa eficiência de transfecção e a
dificuldade de vetorização do gene à área específica da doença.
Neste contexto, o presente trabalho tem como objetivo avaliar diferentes
nanosistemas farmacêuticos como potenciais estratégias para utilização na terapia
gênica. O primeiro sistema consistiu no desenvolvimento de nanoemulsões catiônicas
contendo dois diferentes lipídeos catiônicos, Estearilamina (EA) ou o N-[1-(2,3Dioleoiloxi)propil]-N,N,Ntrimetilamonio
metilsulfato
(DOT AP). Os estudos
preliminares destes sistemas consistiram na avaliação e comparação das suas
propriedades físico-químicas como: granulometria, potencial zeta e PI; da habilidade de
compactação do DNA dos sistemas, através da técnica de retardo da migração do DNA
usando a eletroforese em gel de agarose; e do estudo de estabilidade, utilizando a
técnica de microemultócrito. O segundo
sistema estudado compreendeu o
desenvolvimento de lipossomas recobertos de ácido hialurônico (AH) para vetorização
às células da retina que expressam o receptor CD44 e sua utilização como carreadores
de ácidos nucléicos. Os lipossomas apresentaram em sua composição: DOTAP, DOPE,
2
INTRODUÇÃO
e poderiam conter ou não o lipídeo marcado PE-Rodamina e o conjugado HA-DOPE.
Assim como para as nanoemulsões, as propriedades físico-químicas destes sistemas
(granulometria, potencial zeta e IP) também foram analisadas. Além disso, a
estabilidade dos sistemas e a influência do tempo, do tamanho do plasmídeo e a
presença ou ausência de endotoxinas no plasmídeo utilizado, foi avaliada na formação
dos complexos.
A presente tese será apresentada na seguinte forma:
Inicialmente será apresentada uma introdução, na qual será contextualizada a
importância e os objetivos da tese. Em seguida, será feita uma revisão da literatura com
sua respectiva referência bibliográfica, na qual serão apresentados os fundamentos
teóricos para os capítulos seguintes. A metodologia bem como os resultados e as
discussões desenvolvidas serão apresentados na forma de artigos que foram submetidos
para periódicos. Destaca-se que os artigos são apresentados no formato que foram
enviados para os periódicos. Finalmente, serão apresentadas as considerações finais
sobre o trabalho. Em anexo, encontram-se todos os trabalhos derivados da tese,
incluindo resumos apresentados na forma de pôster e apresentação oral, e ainda, os
resumos expandidos publicados em edições suplementares de periódicos na área de
interesse.
3
______________________________
Capítulo 2
Revisão da Literatura
______________________________
REVISÃO DA LITERATURA
2.0 REVISÃO DA LITERATURA
2.1 Terapia Gênica
A existência de doenças de origem genética e adquiridas, cujas terapias ainda são
ineficientes nos dias atuais, abre espaço para a pesquisa e desenvolvimento de terapias
alternativas que atuem na causa de origem da doença e não apenas nos seus sintomas,
como a terapia gênica. A terapia gênica apresenta enorme potencial para o tratamento de
doenças hereditárias e adquiridas e pode revolucionar o tratamento das doenças que têm
um componente genético. As doenças monogênicas, também conhecidas como
desordens mendelianas, são grandes candidatas à pesquisa na área de terapia gênica.
Elas podem ser classificadas em autossômicas dominantes, autossômicas recessivas e
doenças ligadas ao cromossomo X (Wong e Chiu, 2010). Analisadas separadamente,
estas doenças são extremamente raras, porém, analisadas em conjunto, observa-se que
os vários tipos de doenças monogênicas afetam substancialmente a população, em uma
estimativa de 10 em cada 1000 nascimentos segundo a Organização Mundial de Saúde
(OMS). Diversas outras doenças também têm sido objeto de estudo nesta área como:
câncer, desordens genéticas, desordens imunológicas, desordens degenerativas e
doenças infecciosas incluindo a SIDA (Síndrome da Imunodeficiência Adquirida)
(Nienhuis, 2008).
O princípio básico subjacente à terapia gênica consiste simplesmente na
introdução de material genético no interior celular para que o produto da sua expressão
possa curar ou retardar a progressão da doença. Para tal, é necessário fazer o gene
chegar às células defeituosas, surgindo assim o conceito de transfecção, processo de
entrega e expressão de material genético com sucesso (Verma e Weitzman, 2005).
A função da administração do gene correto é a de compensar o gene defeituoso
contido na célula para deste modo, se conseguir recuperar sua função normal,
eliminando o foco da doença. Porém, ao longo do tempo tem-se verificado uma maior
abrangência do conceito de terapia gênica. Hoje a terapia gênica pode incluir outros
tipos de estratégias para o tratamento de doenças. O gene transfectado pode não estar
necessariamente em falta, mas sua expressão pode ser insuficiente e a administração
exógena do produto da sua expressão ser difícil. Esta forma de terapia gênica tem como
objetivo a produção in vivo de proteínas potencialmente terapêuticas e é chamada
terapia de aumento gênico. Tem-se ainda o direcionamento de genes que quando
expressos podem causar a morte celular, muito estudado para a terapia gênica do câncer
5
REVISÃO DA LITERATURA
(Romano, Mitcheli et al., 2000); a inibição dirigida por expressão gênica, para o
tratamento de doenças onde existe um novo produto gênico ou expressão inapropriada
de um gene, como no caso de câncer e doenças infecciosas (Strachan e Read, 2002); e o
desenvolvimento de vacinas inovadoras promovendo imunização gênica (Felgner,
1998).
É por esse motivo, que a terapia gênica apresenta-se bastante promissora como
alternativa terapêutica para estas doenças, especialmente no que diz respeito aos
carreadores não virais.
Diferentes estratégias podem ser utilizadas no desenvolvimento da terapia gênica,
podendo ser utilizada para substituir um gene defeituoso pelo gene correto; para inibir a
expressão de um gene; ou ainda, para corrigir a expressão de um gene. Atualmente,
pode-se dizer que a terapia gênica refere-se ao uso potencial dos ácidos nucléicos,
incluindo ADN plasmidial, oligonucleotídeos antisenso ou RNA de interferência
(siRNA), para modular a expressão gênica celular com propostas terapêuticas
(Mountain, 2000; Wasungu e Hoekstra, 2006; Bhattacharya e Bajaj, 2009; Liu e Yu,
2010; Verissimo, Lima et al., 2010).
Várias doenças incuráveis pelos métodos terapêuticos convencionais representam
perspectivas futuras para a aplicação da terapia gênica. Contudo, ainda existem
limitações com relação à eficiência e direcionamento dos vetores de transferência
gênica da geração atual. Para que o ADN exógeno seja expresso em uma população
celular faz-se necessário a sua transferência até o local, uma vez que, poucas células
recebem e expressam ADN exógeno (Mountain, 2000). Assim é necessário criar
veículos que transportem e protejam o ADN até que este chegue a uma população
celular alvo. Ao longo do tempo foram surgindo vetores que se encaixam em duas
famílias, os vetores virais e os carreadores não virais. Dentro de cada tipo de vetor
encontra-se uma grande variedade de estratégias e existem vantagens e desvantagens
para cada uma delas. Os requerimentos básicos para uma transfecção efetiva são: a
habilidade de compactar o ADN; de protegê-lo contra degradação e entregá-lo com
especificidade e eficiência à membrana celular; e finalmente, facilitar seu transporte
através dela (Miguel, Pais et al., 2003; Verma e Weitzman, 2005). Os sistemas do tipo
viral, devido à sua elevada eficiência de transferência, são os veículos de transporte e
entrega de material genético mais utilizado tanto em nível experimental (in vivo e in
vitro) quanto em termos de aplicação clínica. No entanto, questões de segurança
relacionadas com a aplicação dos vetores virais, o fato destes vetores poderem assumir a
6
REVISÃO DA LITERATURA
sua forma infecciosa e de poderem induzir resposta inflamatória e imunológica, além da
dificuldade de obtenção e a capacidade de carrear ácidos nucléicos de tamanho limitado,
têm promovido o desenvolvimento de sistemas do tipo não-viral como lipossomas,
nanoemulsões e polímeros catiônicos (Brown, Schatzlein et al., 2001; Davis, 2002;
Smyth Templeton, 2002; Verma e Weitzman, 2005; Tros De Ilarduya, Sun et al., 2010).
2.2 Vetores não-virais
Os vetores não virais apresentam-se como alternativas potenciais a utilização dos
vetores. Os vetores não virais são mais seguros que os virais; apresentam capacidade de
carrear moléculas maiores; são aplicáveis a todos os tipos de células; e são mais fáceis
de serem produzidos. No entanto, apesar de todo o desenvolvimento que têm sido alvo,
este sistema também possui algumas limitações, como o nível de transfecção inferior
aos obtidos pelos vetores virais, a falta de especificidade para a célula alvo e algumas
características físico-químicas que dificultam a sua utilização in vivo (Brown,
Schatzlein et al., 2001; Davis, 2002; Miguel, Pais et al., 2003; Verma e Weitzman,
2005; Tros De Ilarduya, Sun et al., 2010).
Os carreadores catiônicos, lipoplexos e poliplexos, apresentam-se atualmente
como a alternativa mais promissora em relação à utilização dos vetores virais (Abdallah,
Sachs et al., 1995). As moléculas de ADN carregadas negativamente são normalmente
condensadas e/ou complexadas com os reagentes catiônicos antes do seu transporte. O
princípio utilizado é o mesmo para os polímeros e peptídeos catiônicos: os carreadores
catiônicos interagem de uma forma eletrostática com os grupos fosfato do esqueleto do
DNA carregados negativamente levando à formação do complexo (Miguel, Pais et al.,
2003). A presença de surfactantes catiônicos nos lipossomas promove a formação de
uma vesícula com superfície carregada positivamente, o que facilita as fortes interações
entre vesículas e plasmídeos (Bhattacharya e Mandal, 1997). Desta interação resulta a
condensação do DNA em estruturas mais compactas capazes de ultrapassar membranas
biológicas e de proteger da degradação pelas DNAses, dependendo da razão entre a
quantidade de lipídeo e a quantidade de DNA (Miguel, Pais et al., 2003; Barut, Coskun
Ari et al., 2005).
A utilização dos carreadores catiônicos na terapia gênica baseia-se na hipótese de
que os complexos formados são adsorvidos de forma mais eficiente a membrana
plasmática das células devido a interações eletrostáticas. O transporte nuclear do ADN
ainda não está bem esclarecido (Tros De Ilarduya, Sun et al., 2010). As partículas se
7
REVISÃO DA LITERATURA
ligam as superfícies celulares através de interações moleculares não específicas. Os
complexos carregados positivamente e a carga da superfície celular negativa interagem
eletrostaticamente, o que permite sua entrada nas células através dos mecanismos de
endocitose ou “endocitosis-like” após uma ligação aos receptores celulares mediada por
cargas (De Lima, Simoes et al., 2001; Lechardeur e Lukacs, 2002).
Inicialmente, acreditava-se que a fusão entre as membranas lipossomais e
celulares era a primeira etapa na ligação que permitia que lipossomas catiônicos e
aniônicos ultrapassassem a membrana para o interior celular. Tradicionalmente, após
internalização do complexo policátion/ADN por endocitose, grande parte é vetorizado
ao compartimento lisossomal. A liberação citosólica do ADN heterólogo é pré-requisito
para a translocação nuclear e por isso, o aprisionamento e degradação do ADN
plasmidial nos endolisossomos constituem um grande impedimento para uma eficiente
transferência gênica. Apenas uma pequena fração do ADN plasmidial consegue penetrar
no citoplasma. O ADN plasmidial encontra então, barreiras metabólicas e difusionais do
citoplasma, o que resulta ainda em uma diminuição de moléculas de plasmídeo intactas
que conseguem atingir o complexo do poro nuclear. A liberação do ADN no interior
citoplasmático geralmente é atribuída à habilidade dos lipídeos catiônicos em
desestabilizar a membrana do endossomo. Neste caso, a natureza da membrana do
lipoplexo é essencial, pois permite a troca de lipídeos entre a membrana do endossomo
e o lipoplexo, resultando em perturbações da membrana que são pré-requisitos para o
escape do ADN. A translocação nuclear do ADN acontece ou devido à desmontagem do
envelope nuclear, ou por transporte ativo nuclear via o complexo do poro nuclear (Tros
De Ilarduya, Sun et al., 2010). Uma das razões para a baixa eficiência de transfecção
dos lipídeos catiônicos tem sido relacionada à insuficiente proteção do ADN contra as
nucleases intracelulares. A comparação entre vetores virais e o transporte celular de
plasmídeos deve revelar as estratégias utilizadas pelos vírus para solucionar estes
problemas de barreiras que impedem o transporte do ADN através de sistemas não
virais para terapia gênica.
Dados recentes sugerem que tanto a restrita mobilidade, quanto a instabilidade
metabólica do ADN plasmidial relacionadas à barreira nuclear, contribuem para a
eficiência de transfecção limitada destes sistemas (Wattiaux, Laurent et al., 2000;
Brown, Schatzlein et al., 2001; Davis, 2002; Lechardeur e Lukacs, 2002; Lv, Zhang et
al., 2006; Bhattacharya e Bajaj, 2009; Tros De Ilarduya, Sun et al., 2010). Porém,
alguns estudos demonstram que a transcrição parece estar muito mais relacionada a esta
8
REVISÃO DA LITERATURA
limitada eficiência que o próprio transporte do ADN na utilização dos vetores não virais
(Wasungu e Hoekstra, 2006). Atingir o transporte celular eficiente depende de um
grande número de fatores que incluem: a estrutura química dos reagentes catiônicos que
poderão ser utilizados, a estrutura supramolecular dos lipoplexos e poliplexos, as
interações com as membranas celulares, sua internalização e localização intracelular, a
liberação do ADN pelos carreadores catiônicos e o papel dos lipídeos neutros (helper
lipids) nos carreadores catiônicos (Tros De Ilarduya, Sun et al., 2010). A ligação de
radicais específicos aos sistemas como polietilenoglicol (PEG), polietilinoimina (PEI),
poli-L-lisina (PLL), tem sido utilizada com moderado sucesso superando alguns dos
problemas relacionados às barreiras enfrentadas por estes sistemas; enquanto que a
ligação a peptídeos nucleares tem sido uma estratégia utilizada para superar os
problemas relacionados ao escape do endossomo e ao transporte nuclear (Brown,
Schatzlein et al., 2001).
Apesar de serem menos eficientes, especialmente se tratando de estudos in vivo,
sabe-se que os lipoplexos e poliplexos são imunologicamente inertes e potencialmente
mais seguros que os vetores virais. Por serem relativamente fáceis de produzir e
poderem ser modificados quimicamente com o intuito de aperfeiçoar a transfecção,
inúmeras pesquisas nessa área específica tem aumentado drasticamente nos últimos
anos. Portanto, inúmeros dispositivos catiônicos têm sido sintetizados e modificações
estruturais racionais têm sido desenvolvidas de maneira sistemática com o intuito de
correlacionar estrutura e atividade de transfecção. Adicionalmente, o desempenho dos
vetores não virais pode ser otimizado também através da sua vetorização a tipos
celulares específicos e em um modelo de internalização celular distinto, considerando a
possibilidade de que nem todo modelo é efetivamente igual em transportar o ADN ao
citosol, importante passo para o evento de expressão gênica (Wasungu e Hoekstra,
2006).
Os lipídeos catiônicos utilizados na terapia gênica são compostos basicamente de
três domínios básicos: uma cabeça carregada positivamente (com um grupo amônio, por
exemplo); uma cadeia hidrofóbica; e um braço espaçador que liga os dois domínios
anteriores. Os domínios polares e hidrofóbicos parecem apresentar efeitos dramáticos
tanto no que concerne a transfecção quanto aos níveis de toxicidade (Audouy e
Hoekstra, 2001; Lv, Zhang et al., 2006; Wasungu e Hoekstra, 2006; Nam, Park et al.,
2009). Existem dois tipos básicos de domínios hidrofóbicos: as cadeias alifáticas e os
derivados baseados no colesterol. Normalmente, lipídeos catiônicos que apresentam
9
REVISÃO DA LITERATURA
cadeias alifáticas simples são mais tóxicos e menos eficientes que os que apresentam
cadeias duplas. De qualquer forma, existem casos em que os lipídeos com cadeia
simples apresentam melhores resultados que os de dupla cadeia, tornando claro que não
se pode abolir totalmente o uso dos lipídeos de cadeia simples na terapia gênica. Os
efeitos de citotoxicidade estão associados a natureza catiônica dos vetores, que são
determinados principalmente pela estrutura do grupo hidrofílico. A cabeça polar
consiste de sais de amônio primários, secundários, terciários ou quaternários, mas os
grupos guanidino e imidazol também têm sido utilizados. A maioria das ligações nos
lipídeos sintéticos são ligações éter, éster ou amida. Apesar dos compostos com ligação
éter apresentarem melhor eficiência de transfecção, eles apresentam estabilidade
exacerbada o que prejudica sua biodegradação, causando assim, toxicidade (Audouy e
Hoekstra, 2001; Lv, Zhang et al., 2006). A Figura 1 mostra a estrutura dos dois lipídeos
catiônicos utilizados no desenvolvimento deste trabalho, EA e DOTAP.
(A)
(B)
Figura 1. Estrutura química dos lipídeos catiônicos EA (A) e DOTAP (B).
Para incrementar a transfecção, os lipídeos catiônicos são muitas vezes acrescidos
dos lipídeos neutros, como DOPE, com potencial de promover a conversão dos
lipoplexos de fase lamelar em estruturas não lamelares, e colesterol (Figura 2), o que
provavelmente racionaliza sua habilidade de geralmente aumentar o poder de
transfecção destes sistemas (Wasungu e Hoekstra, 2006). Enquanto os lipídeos que
facilitam a transformação dos lipoplexos no tipo de fase não bicamada apresentam alta
taxa de transfecção in vitro; lipídeos como o colesterol, que confere maior estabilidade
10
REVISÃO DA LITERATURA
sérica dos sistemas, são mais adequados para o transporte de genes in vivo (Tros De
Ilarduya, Sun et al., 2010).
(A)
(B)
O maior problema do uso de lipídeos catiônicos como carreadores gênicos é sua
inadequada compatibilidade com o soro e outros fluidos biológicos o que os torna
impróprios para estudos in vivo. A toxicidade dos sistemas e a reduzida eficiência de
transfecção decorrente da instabilidade dos complexos formados com os ácidos
nucléicos em presença de proteínas, também têm sido relatadas (Filion e Phillips, 1998;
Yi, Yune et al., 2000; Choi, Kim et al., 2004). Adicionalmente, a expressão dos genes
exógenos, provindos da vetorização não-viral, tende a ser passageira, e geralmente, as
doenças cuja terapia gênica poderá ser indicada, requer alto nível de expressão do
transgene (Mountain, 2000; Hung, Hwang et al., 2005; Verma e Weitzman, 2005).
Para solucionar este problema, grupos funcionais como PEG têm sido ligados aos
fosfolipídeos para tornar o sistema furtivo. A presença destes grupos funcionais pode
impedir interações excessivas entre os lipoplexos, impedindo assim, a formação de
agregados. Como resultado, o tamanho médio das partículas de lipoplexos resultantes
será menor e pode ser processado pelas células diferentemente dos grandes complexos.
O tamanho e a carga dos vetores não virais são parâmetros importantes, mas seu papel
específico ainda permanece incerto. Geralmente, partículas maiores apresentam taxa de
transfecção mais elevada que as menores, devido provavelmente ao aumento da
11
REVISÃO DA LITERATURA
sedimentação dos sistemas sobre as células. No entanto, o PEG também promove a
formação de uma barreira estável que inibe fortemente a liberação dos ácidos nucléicos
dos endossomos (Wasungu e Hoekstra, 2006).
Carreadores coloidais incluindo lipossomas, nanopartículas lipídicas sólidas,
nanoemulsões e nanopartículas poliméricas são plataformas atrativas para a terapia
gênica (Liu e Yu, 2010). Dentre estes vetores não virais, lipossomas e nanoemulsões
têm particularmente, excelente potencial para aplicações no transporte de genes.
2.2.1 Lipossomas
O uso de lipossomas na terapia gênica é bastante promissor devido principalmente
a sua não imunogenicidade e alta segurança e apresenta uma série de vantagens em
relação aos vetores virais. A maior delas é a ausência de imunogenicidade após
administração in vivo, particularmente após administração sistêmica. Por este motivo, os
complexos lipossomas/ ácidos nucléicos podem ser re-administrados sem danos ao
paciente e sem comprometer a eficácia da terapia gênica não viral (Smyth Templeton,
2002; Kwon, Nam et al., 2008; Bhattacharya e Bajaj, 2009).
Os lipossomas utilizados nos estudos de terapia gênica apresentam tipicamente ao
menos dois componentes: um lipídeo catiônico e um lipídeo neutro. Eles oferecem a
interface carregada positivamente que permite a efetiva complexação com os ácidos
nucléicos via interações eletrostáticas resultando em nanosistemas que oferecem
biocompatibilidade, baixa toxicidade e a possibilidade de produção em larga escala, o
que é necessário para aplicações clínicas in vivo. Ao mesmo tempo, devido à natureza
dos lipoplexos, eles interagem com as cargas negativas das superfícies celulares
favorecendo e permitindo o transporte do ADN ao interior celular. Os lipossomas
catiônicos também protegem o ADN contra o ataque de enzimas como as DNAses
(Smyth Templeton, 2002; Kwon, Nam et al., 2008; Bhattacharya e Bajaj, 2009; Tros De
Ilarduya, Sun et al., 2010).
Apesar de alguns ensaios clínicos estarem em andamento, as aplicações clínicas
dos lipossomas têm sido limitadas devido a sua instabilidade in vivo. Estudos
demonstram que eles formam grandes agregados com componentes sanguíneos,
apresentando sensibilidade sérica, induzindo certa instabilidade, e que estes agregados
ficam presos no leito dos capilares pulmonares. Os estudos realizados com os
lipossomas catiônicos, bem como com os complexos lipossomas catiônicos/ADN, têm
sido direcionados no sentido de superar essas limitações e logo aumentar o potencial
12
REVISÃO DA LITERATURA
terapêutico desses sistemas. Alguns desses estudos passam pela alteração da
composição lipídica dos lipossomas (Bhattacharya e Mandal, 1997; De Lima, Simoes et
al., 2001); pelo desenvolvimento de novas formulações farmacêuticas (Hara, Liu et al.,
1997; Hung, Hwang et al., 2005); pela incorporação de radicais nos complexos, de
forma a aumentar sua especificidade celular e pela incorporação de peptídeos
fusogênicos (Kim, Chung et al., 2001); pela adição de polímeros catiônicos, que
aumentem a taxa de transfecção (Feng, Ruan et al., 2004; Lee, Chun et al., 2005; Lee,
Zhang et al., 2007); e pela incorporação de polímeros hidrofílicos como o PEG, de
modo a aumentar o tempo de circulação dos complexos na corrente sanguínea devido a
um aumento da sua estabilidade física (Hong, Zheng et al., 1997; Teixeira, Rosilio et
al., 2001; Choi, Mackay et al., 2003; Palmer, Chen et al., 2003; Salvati, Ciani et al.,
2006; Bombelli, Faggioli et al., 2007; Buyens, Demeester et al., 2009; Hobel e Aigner,
2009).
Os complexos lipossomas catiônicos/ADN podem ser administrados por diversas
vias in vivo. Estas vias incluem injeção direta (por exemplo: intra-tumoral), intravenosa,
intraperitoneal,
intra-arterial,
intra-esplênica,
mucosa
(nasal,
vaginal,
retal),
intramuscular, subcutânea, trans-dérmica, intra-dérmica, sub-retiniana, intravitreal,
intra-traqueal, intra-cranial e outras (Smyth Templeton, 2002; Kwon, Nam et al., 2008;
Bhattacharya e Bajaj, 2009).
Os fosfolipídios mais amplamente encontrados nas membranas biológicas são a
fosfatidilcolina (PC) ou fosfatidiletanlamina (PE). A cabeça dos fosfolipídios naturais
torna-os uma opção para diminuir a toxicidade dos lipídeos catiônicos (Bhattacharya e
Bajaj, 2009). Em particular, o DOPE forma estruturas do tipo fase hexagonal invertida
HII (não-bicamada) em pH neutro e temperatura fisiológica. No entanto, quando
combinados aos lipídeos catiônicos eles podem participar da formação de bicamadas.
Os lipossomas catiônicos contendo colesterol parecem apresentar-se estruturalmente
mais estáveis em meio fisiológico, permitindo assim que os lipoplexos atinjam seu
tecido alvo intacto, protegendo assim o ADN contra degradação e eventualmente,
facilitando a transfecção. Experimentos de calorimetria de titulação isotérmica indicam
que a interação DOTAP: DOPE (1:1) e ADN é um processo de entropia. Deve-se
observar que a interação entre os lipoplexos e os lipídeos das membranas celulares pode
resultar em estruturas organizacionais diferentes da estrutura original. Logo, a
transferência gênica mediada por lipoplexos não depende apenas da formulação do
lipossoma catiônico e da sua estrutura original, mas também da interação destes com as
13
REVISÃO DA LITERATURA
células e a estrutura resultante (Tros De Ilarduya, Sun et al., 2010) .
Esses complexos são incorporados pelas células, por fusão ou endocitose, sendo a
endocitose a sua principal forma de entrada, o que implica a subseqüente libertação do
endossomo e tráfego do DNA até o núcleo (De Lima, Simoes et al., 2001; Simoes,
Slepushkin et al., 2001). A liberação do DNA no citoplasma é geralmente atribuída à
habilidade dos lipídeos catiônicos em desestabilizar a membrana do endossomo.
Quando os ácidos nucléicos conseguem escapar do endossomo, eles o fazem em um
estágio anterior a endocitose acontecer. Neste caso, a natureza da membrana do
lipoplexo é crucial e permite uma troca de lipídeos entre a membrana do endossomo e o
lipoplexo, resultando em perturbações na membrana que são pré-requisitos para o
escape do ADN do lipossoma. Este mecanismo não está bem esclarecido, mas quando o
DOPE participa da formulação de lipossomas catiônicos, a liberação dos ácidos
nucléicos pode ser beneficiada pela tendência do DOPE em promover mudanças
polimórficas significativas na fase lipídica sob condição fisiológica. O DOPE
particularmente promove prontamente a formação de uma fase hexagonal invertida (a
temperatura ambiente e pH fisiológico) a partir da fase lamelar de líquido cristalino na
maioria das membranas. Por isso, o DOPE proporciona o rompimento do endossomo
devido à fusão da membrana. Uma vez em seu interior, o pH dos compartimentos do
endossomo caem de 7 para 5,5 e parte dos ácidos nucléicos ligados escapa dos
endossomos precoces para o citosol. O transporte citoplasmático dos endossomos tem
um papel importante em trazer o material transfectado para perto da região perinuclear.
O material genético então pode ser liberado e conseqüentemente transcrito. Tem sido
demonstrado que o transporte nuclear é uma barreira significante no transporte genético
e até o momento, não se conhece o mecanismo de transporte através da membrana
nuclear. No entanto, sabe-se que a importação de ácidos nucléicos de grande tamanho
ao núcleo acontece devido a associação de ácidos nucléicos às proteínas requeridas para
o transporte (Bhattacharya e Bajaj, 2009; Tros De Ilarduya, Sun et al., 2010).
Em resumo, a eficiência dos ensaios in vivo dos complexos lipossomas
catiônicos/ácido nucléico depende da sua morfologia, dos mecanismos de transporte da
membrana celular e entrada no núcleo, da habilidade de vetorizá-los para a superfície de
receptores específicos, e da sua habilidade de penetrar através das barreiras e tecidos
específicos. Geralmente, os complexos lipossomas catiônicos/ácido nucléico que se
mostram eficazes em modelos de doenças animais têm alta meia-vida na circulação
sanguínea; são estáveis em contato com o soro; apresentam alta distribuição;
14
REVISÃO DA LITERATURA
encapsulam de maneira eficiente tamanho variado de ácidos nucléicos; são vetorizados
a tipos celulares específicos e órgãos alvos; penetram barreiras estreitas em vários
órgãos e mesmo através do tecido alvo; podem ter a razão lipídeo: ácido nucléico
otimizada em suspensões coloidais in vivo; podem ser fracionados para produzir uma
população homogênea de complexos antes da injeção; e podem ser administrados
repetidamente (Smyth Templeton, 2002).
2.2.2 Nanoemulsões
Emulsões são dispersões termodinamicamente instáveis cujo tamanho de gotículas
tende a aumentar com o tempo culminando com a separação se fases. As nanoemulsões
apresentam uma série de vantagens em relação às emulsões ordinárias, incluindo: maior
área de superfície e energia livre, evitando os fenômenos de instabilidade de cremagem,
floculação, coalescência e separação de fases (Solans, Izquierdo et al., 2005;
Constantinides, Chaubal et al., 2008; Gutierrez, Gonzalez et al., 2008; Liu e Yu, 2010).
As nanoemulsões utilizadas como sistemas de liberação de ácidos nucléicos são
geralmente compostas por um núcleo oleoso de origem vegetal ou semi-sintético
estabilizado na sua superfície por uma mistura binária de fosfolipídios, surfactantes e
lipídeos catiônicos (Yi, Yune et al., 2000; Liu e Yu, 2010).
A seleção do núcleo oleoso é geralmente realizada com base na estabilidade das
formulações e nas propriedades físico-químicas desejadas. Dentre os óleos de vegetais,
o óleo de soja tem amplamente utilizado (Kim, Chung et al., 2000; Yi, Yune et al.,
2000; Kim, Kim et al., 2003; Barut, Coskun Ari et al., 2005). O óleo de linhaça também
tem sido objeto de estudo (Nam, Park et al., 2009). Atualmente, tem-se observado um
interesse crescente no uso dos triglicerídeos sintéticos, especialmente os de cadeia
média (TCM) no preparo de nanoemulsões (Teixeira, Dubernet et al., 1999; Teixeira,
Dubernet et al., 2001; Teixeira, Rosilio et al., 2001; Bivas-Benita, Oudshoorn et al.,
2004; Martini, Fattal et al., 2008).
As emulsões utilizadas como sistemas de liberação de ácidos nucléicos
caracterizam-se por apresentarem uma interface composta por um agente tensoativo
carregado positivamente. Esses têm por objetivo principal a associação dos ácidos
nucléicos com a estrutura coloidal (Teixeira, Dubernet et al., 1999; Teixeira, Dubernet
et al., 2003; Tamilvanan, 2004). A adição do lipídeo catiônico confere carga positiva à
superfície da gotícula, permitindo a associação dos ácidos nucléicos à interface das
emulsões através da formação de um par iônico em meio aquoso. A proporção da fase
15
REVISÃO DA LITERATURA
oleosa das emulsões catiônicas utilizadas como sistemas de liberação de ácidos
nucléicos varia de 5 a 35 % da composição final das formulações (Liu, Yang et al.,
1996; Hara, Liu et al., 1997; Yi, Yune et al., 2000; Chung, Kim et al., 2001; Liu e Yu,
2010). No caso dos polinucleotídeos de elevado peso molecular, como o DNA, a
presença dos surfactantes catiônicos, também chamados lipídeos catiônicos, na interface
tem a função de associar e compactar o ácido nucléico visando a um efetivo transporte
intracelular (Eastman, Siegel et al., 1997; Liu e Yu, 2010).
Os lipídeos utilizados na composição das emulsões podem ser monocatiônicos ou
policatiônicos (Zhang, Xu et al., 2004). Os lipídeos monocatiônicos podem apresentar
funções amina primárias (EA), secundárias, como o 1,2-Dioleil-sn-Glicerol- 3-{[ácido
imidoacético N- (5-Amino-1-Carboxipentil)] Succinato} (DOGS), terciárias 3ß-[N(N',N'-Dimetilaminoetano)-carbamoil] Colesterol
(DC-Chol) ou
ainda quaternárias
(DOTAP). O grupamento amina é responsável pelas interações eletrostáticas que
ocorrem entre os lipídeos catiônicos e os grupamentos fosfato, carregados
negativamente, dos ácidos nucléicos. A utilização de lipídeos policatiônicos tem sido
menos freqüentemente descrita na obtenção de emulsões, em comparação aos lipídeos
monocatiônicos. Contudo, a maior densidade de cargas das membranas dos complexos
devido à utilização dos novos lipídeos multivalentes, tem promovido um incremento na
eficiência de transfecção em comparação com o DOTAP quando utilizados com uma
pequena razão molar de lipídeos neutros. Isto é importante, pois minimiza os efeitos
tóxicos conhecidos dos lipídeos catiônicos. Além dos lipídeos mono e polivalentes,
lipídeos derivados da guanidina, imidazol, colesterol e peptídeos catiônicos também têm
sido utilizados (Zhang, Xu et al., 2004).
Além da utilização dos lipídeos catiônicos, as emulsões catiônicas utilizadas na
terapia gênica geralmente são obtidas a partir de misturas binárias com fosfolipídios
(Liu, Yang et al., 1996; Hara, Liu et al., 1997; Yi, Yune et al., 2000; Chung, Kim et al.,
2001; Hung, Hwang et al., 2005). Os fosfolipídios apresentam um grupamento polar
cuja carga depende do pH do meio além das cadeias hidrocarbonadas que podem ser
saturadas (1,2-diestearoil-sn-glicerol-3-fosfatidilcolina - DSPC) ou insaturadas (DOPE).
Desta forma, a relação de cargas positivas (lipídeos catiônicos) e negativas (ácidos
nucléicos) pode ser otimizada através da utilização destes lipídeos em combinação com
os lipídeos catiônicos. Adicionalmente, a adição de fosfolipídios semi-sintéticos, como
DOPE, é capaz de melhorar a atividade de transfecção in vitro e in vivo de emulsões
catiônicas devido às propriedades fusogênicas deste fosfolipídio (Kim, Chung et al.,
16
REVISÃO DA LITERATURA
2001). Os lipídeos catiônicos mais comumente utilizados na terapia gênica são o DCChol, a EA e o DOTAP. No entanto, novos lipídeos catiônicos formados por um núcleo
aspartato ou glutamato, uma cabeça lisina e duas cadeiais alquil, têm demonstrado
expressão gênica bastante eficiente e citotoxicidade inferior (Liu e Yu, 2010).
O uso de lipídeos catiônicos derivados do colesterol também tem sido descrito na
literatura de sistemas emulsionados, com destaque para o lipídeo catiônico DC-Chol,
que apresenta no seu domínio hidrofóbico um grupamento colesteril, que serve como
âncora hidrofóbica (Hara, Liu et al., 1997; Zhang, Xu et al., 2004).
Para incrementar a estabilidade física das formulações e reduzir as interações de
proteínas com as emulsões catiônicas, os fosfolipídios podem ser ligados
covalentemente
ao
PEG,
como
o
fosfatidiletanolamina-N-monometoxi-[PEG]
(DSPEPEG), e usados em associação com outros fosfolipídeos na composição de
emulsões como veículo de ADN (Kim, Chung et al., 2000; Yi, Yune et al., 2000;
Chesnoy, Durand et al., 2001) e oligonucleotídeos (Teixeira, Dubernet et al., 2001;
Teixeira, Rosilio et al., 2001). De fato, tem sido demonstrado que a presença de lipídeos
conjugados ao PEG na interface de sistemas coloidais cria uma barreira estérica ao
acesso de proteínas, prevenindo assim a agregação das nanoestruturas. Ainda
objetivando incrementar a estabilidade destes sistemas, alguns autores descrevem o uso
de tensoativos não-iônicos na preparação de emulsões contendo ADN (Liu, Yang et al.,
1996; Choi, Mackay et al., 2003; Hung, Hwang et al., 2005); (Liu, Yang et al., 1996;
Hara, Liu et al., 1997; Kim, Chung et al., 2001; Choi, Kim et al., 2004). Os efeitos da
adição de tensoativos não-iônicos na distribuição granulométrica, atividade de
transfecção e sensibilidade sérica dos complexos emulsão/ADN foram avaliados (Liu,
Yang et al., 1996). As emulsões foram preparadas com óleo de castor, DC-Chol e
quatro tipos diferentes de co-tensoativos: Tween®, Span 60®, Brij® e Pluronic®. Foi
observado que a adição de tensoativos não-iônicos promove um incremento na
transfecção celular em presença de soro e que esse incremento depende principalmente
da cabeça polar do tensoativo. Os Tweens® apresentaram os melhores resultados
devido à inibição da formação de agregados de DNA pela presença da cadeia ramificada
de polioxietileno. Outro estudo também avaliou a influência de tensoativos não-iônicos
em emulsões para terapia gênica (Kim, Chung et al., 2001). Neste caso, as emulsões
foram preparadas utilizando lipídios catiônicos, diferentes tipos de tensoativos nãoiônicos e esqualeno. A eficiência de transfecção foi avaliada comparando-as com os
lipossomas de composição idêntica na presença e ausência de soro. Foi observado que a
17
REVISÃO DA LITERATURA
emulsão composta de DOTAP/DOPE/Tween 80® apresentou atividade de transfecção
bem superior à obtida com os lipossomas correspondentes em ensaios de transfecção em
presença de soro. Os tensoativos propostos nessas formulações são geralmente os
ésteres de ácidos graxos do sorbitano, como a série de Tween® e Span®, que são
aprovados em várias farmacopéias para uso parenteral. Aos tensoativos como o Tween
80®, têm sido atribuída a formação de uma barreira estérica na interface através de suas
cadeias de caráter hidrofílico, impedindo assim a aproximação e agregação das
emulsões com proteínas (Hara, Liu et al., 1997; Choi, Kim et al., 2004).
Os avanços alcançados com o desenvolvimento de novas tecnologias na
formulação de nanoemulsões catiônicas para terapia gênica têm permitido o controle
das suas propriedades de superfície como hidrofobicidade e carga da estrutura química.
Quando as emulsões apresentam a superfície carregada positivamente, elas podem
interagir eletrostaticamente como genes terapêuticos devido à formação espontânea do
complexo emulsão catiônica/ADN. Esses complexos nanométricos apresentam
potencial terapêutico, pois a compactação do ADN pode protegê-lo contra a degradação
enzimática que ocorre nos fluidos biológicos e facilitam a entrada celular do ADN com
posterior transporte ao núcleo. Contudo, para que as nanoemulsões catiônicas sejam
utilizadas como promissores carreadores gênicos é imprescindível desenvolver sistemas
reprodutíveis, estáveis e de formulação bem definida. Dentre as várias abordagens, tem
sido demonstrado que as nanoemulsões catiônicas apresentam alto potencial como
vetores não virais para terapia gênica devido: (1) a sua biocompatibilidade já que a
maioria dos seus constituintes são óleos não tóxicos e lipídeos anfifílicos; (2) a sua
capacidade de formação de nanocomplexos com o ADN carregado negativamente,
promovendo proteção do material genético contra a degradação enzimática dos fluidos
biológicos; (3) a sua estabilidade na corrente sanguínea devido ao meno reconhecimento
de sua superfície pelas células relacionadas à imunidade e proteínas séricas; e (4) a
possibilidade de modificação da sua superfície lipídica (Nam, Park et al., 2009).
18
______________________________
Referências Bibliográficas
______________________________
REFERÊNCIAS BIBLIOGRÁFICAS
3. REFERÊNCIAS BIBLIOGRÁFICAS
Abdallah, B., L. Sachs, et al. Non-viral gene transfer: applications in developmental
biology and gene therapy. Biology of the cell / under the auspices of the European Cell
Biology Organization, v.85, n.1, p.1-7. 1995.
Audouy, S. e D. Hoekstra. Cationic lipid-mediated transfection in vitro and in vivo.
Molecular Membrane Biology, v.18, n.2, Apr-Jun, p.129-143. 2001.
Barut, K. D., F. F. Coskun Ari, et al. Development and characterization of a cationic
emulsion formulation as a potential pDNA carrier system. Turkish Journal of
Chemistry, v.29, p.27-40. 2005.
Bhattacharya, S. e A. Bajaj. Advances in gene delivery through molecular design of
cationic lipids. Chemical Communications, n.31, Aug 21, p.4632-56. 2009.
Bhattacharya, S. e S. S. Mandal. Interaction of surfactants with DNA. Role of
hydrophobicity and surface charge on intercalation and DNA melting. Biochimica Et
Biophysica Acta-Biomembranes, v.1323, n.1, Jan, p.29-44. 1997.
Bivas-Benita, M., M. Oudshoorn, et al. Cationic submicron emulsions for pulmonary
DNA immunization. Journal of Controlled Release, v.100, n.1, Nov 5, p.145-155. 2004.
Bombelli, C., F. Faggioli, et al. PEGylated lipoplexes: Preparation Protocols affecting
DNA condensation and cell Transfection efficiency. Journal of Medicinal Chemistry,
v.50, p.6274-6278. 2007.
Brown, M. D., A. G. Schatzlein, et al. Gene delivery with synthetic (non viral) carriers.
International Journal of Pharmaceutics, v.229, n.1-2, Oct 23, p.1-21. 2001.
Buyens, K., J. Demeester, et al. Elucidating the Encapsulation of Short Interfering RNA
in PEGylated Cationic Liposomes. Langmuir, v.25, n.9, p.4886-4891. 2009.
22
REFERÊNCIAS BIBLIOGRÁFICAS
Chesnoy, S., D. Durand, et al. Improved DNA/emulsion complex stabilized by
poly(ethylene glycol) conjugated phospholipid. Pharmaceutical Research, v.18, n.10,
Oct, p.1480-4. 2001.
Choi, J. S., J. A. Mackay, et al. Low-pH-sensitive PEG-stabilized plasmid-lipid
nanoparticles: Preparation and characterization. Bioconjugate Chemistry, v.14, n.2,
Mar-Apr, p.420-429. 2003.
Choi, W. J., J. K. Kim, et al. Low toxicity of cationic lipid-based emulsion for gene
transfer. Biomaterials, v.25, n.27, Dec, p.5893-5903. 2004.
Chung, H., T. W. Kim, et al. Oil components modulate physical characteristics and
function of the natural oil emulsions as drug or gene delivery system. Journal of
Controlled Release, v.71, n.3, Apr, p.339-350. 2001.
Constantinides, P. P., M. V. Chaubal, et al. Advances in lipid nanodispersions for
parenteral drug delivery and targeting. Advanced Drug Delivery Reviews, v.60, n.6,
Mar 17, p.757-67. 2008.
Davis, M. E. Non-viral gene delivery systems. Current Opinion in Biotechnology, v.13,
n.2, Apr, p.128-131. 2002.
De Lima, M. C. P., S. Simoes, et al. Cationic lipid-DNA complexes in gene delivery:
from biophysics to biological applications. Advanced Drug Delivery Reviews, v.47,
n.2-3, Apr, p.277-294. 2001.
Eastman, S. J., C. Siegel, et al. Biophysical characterization of cationic lipid: DNA
complexes. Biochimica Et Biophysica Acta, v.1325, n.1, Apr 3, p.41-62. 1997.
Felgner, P. L. DNA vaccines. Current Biology, v.8, n.16, Aug, p.R551-R553. 1998.
Feng, S. S., G. Ruan, et al. Fabrication and characterizations of a novel drug delivery
device liposomes-in-microsphere (LIM). Biomaterials, v.25, n.21, Sep, p.5181-5189.
2004.
23
REFERÊNCIAS BIBLIOGRÁFICAS
Filion, M. C. e N. C. Phillips. Major limitations in the use of cationic liposomes for
DNA delivery. International Journal of Pharmaceutics, v.162, n.1-2, Mar, p.159-170.
1998.
Gutierrez, J. M., C. Gonzalez, et al. Nano-emulsions: New applications and
optimization of their preparation. Current Opinion in Colloid & Interface Science, v.13,
n.4, p.245-251. 2008.
Hara, T., F. Liu, et al. Emulsion formulations as a vector for gene delivery in vitro and
in vivo. Advanced Drug Delivery Reviews, v.24, n.2-3, Mar, p.265-271. 1997.
Hengge, U. R. Progress and prospects of skin gene therapy: a ten year history. Clinics in
Dermatology, v.23, n.1, Jan-Feb, p.107-114. 2005.
Hobel, S. e A. Aigner. Nonviral delivery platform for therapeutic RNAi: pegylated
siRNA/cationic liposome complexes for targeting of the proto-oncogene bcl-2. Future
Oncology, v.5, n.1, p.13-17. 2009.
Hong, K. L., W. W. Zheng, et al. Stabilization of cationic liposome-plasmid DNA
complexes by polyamines and poly(ethylene glycol)-phospholipid conjugates for
efficient in vivo gene delivery. Febs Letters, v.400, n.2, Jan, p.233-237. 1997.
Hung, C. F., T. L. Hwang, et al. Physicochemical characterization and gene transfection
efficiency of lipid,emulsions with various co-emulsifiers. International Journal of
Pharmaceutics, v.289, n.1-2, Jan, p.197-208. 2005.
Kim, T. W., H. Chung, et al. In vivo gene transfer to the mouse nasal cavity mucosa
using a stable cationic lipid emulsion. Molecules and Cells, v.10, n.2, Apr 30, p.142-7.
2000.
______. Optimization of lipid composition in cationic emulsion as in vitro and in vivo
transfection agents. Pharmaceutical Research, v.18, n.1, Jan, p.54-60. 2001.
24
REFERÊNCIAS BIBLIOGRÁFICAS
Kim, Y. J., T. W. Kim, et al. The effects of serum on the stability and the transfection
activity of the cationic lipid emulsion with various oils. International Journal of
Pharmaceutics, v.252, n.1-2, Feb, p.241-252. 2003.
Kwon, S. M., H. Y. Nam, et al. In vivo time-dependent gene expression of cationic
lipid-based emulsion as a stable and biocompatible non-viral gene carrier. Journal of
Controlled Release, v.128, n.1, May 22, p.89-97. 2008.
Lambert, G., E. Fattal, et al. Polyisobutylcyanoacrylate nanocapsules containing an
aqueous core for the delivery of oligonucleotides. International Journal of
Pharmaceutics, v.214, n.1-2, Feb, p.13-16. 2001.
Lechardeur, D. e G. L. Lukacs. Intracellular barriers to non-viral gene transfer. Current
Gene Therapy, v.2, n.2, May, p.183-94. 2002.
Lee, D., W. Zhang, et al. Thiolated chitosan/DNA nanocomplexes exhibit enhanced and
sustained gene delivery. Pharmaceutical research, v.24, n.1, Jan, p.157-67. 2007.
Lee, M. K., S. K. Chun, et al. The use of chitosan as a condensing agent to enhance
emulsion-mediated gene transfer. Biomaterials, v.26, n.14, May, p.2147-2156. 2005.
Liu, C. H. e S. Y. Yu. Cationic nanoemulsions as non-viral vectors for plasmid DNA
delivery. Colloids Surf B Biointerfaces, v.79, n.2, Sep 1, p.509-15. 2010.
Liu, F., J. Yang, et al. Effect of non-ionic surfactants on the formation of
DNA/emulsion complexes and emulsion-mediated gene transfer. Pharmaceutical
Research, v.13, n.11, Nov, p.1642-6. 1996.
Lv, H., S. Zhang, et al. Toxicity of cationic lipids and cationic polymers in gene
delivery. Journal of Controlled Release, v.114, n.1, Aug 10, p.100-9. 2006.
Martini, E., E. Fattal, et al. Effect of cationic lipid composition on properties of
oligonucleotide/emulsion
complexes: Physico-chemical
and release
studies.
International Journal of Pharmaceutics, v.352, n.1-2, Mar 20, p.280-286. 2008.
25
REFERÊNCIAS BIBLIOGRÁFICAS
Miguel, M. G., A. Pais, et al. DNA-cationic amphiphile interactions. Colloids and
Surfaces A-Physicochemical and Engineering Aspects, v.228, n.1-3, Nov, p.43-55.
2003.
Mountain, A. Gene therapy: the first decade. Trends in Biotechnology, v.18, n.3, Mar,
p.119-128. 2000.
Nam, H. Y., J. H. Park, et al. Lipid-based emulsion system as non-viral gene carriers.
Archives of Pharmacal Research, v.32, n.5, p.639-646. 2009.
Nienhuis, A. The growing clinical impact of gene therapy. Molecular Therapy, v.16,
n.6, Jun, p.995-6. 2008.
Palmer, L. R., T. Chen, et al. Transfection properties of stabilized plasmid-lipid
particles
containing cationic
PEG
lipids.
Biochimica
Et
Biophysica
Acta-
Biomembranes, v.1611, n.1-2, Apr, p.204-216. 2003.
Romano, G., P. Mitcheli, et al. Latest developments in gene transfer technology:
Achievements, perspectives, and controversies over therapeutic applications. Stem
Cells, v.18, n.1, p.19-39. 2000.
Salvati, A., L. Ciani, et al. Physico-chemical characterization and transfection efficacy
of cationic liposomes containing the pEGFP plasmid. Biophysical Chemistry, v.121,
n.1, Apr 20, p.21-9. 2006.
Simoes, S., V. Slepushkin, et al. On the mechanisms of internalization and intracellular
delivery mediated by pH-sensitive liposomes. Biochimica Et Biophysica ActaBiomembranes, v.1515, n.1, Nov, p.23-37. 2001.
Smyth Templeton, N. Liposomal delivery of nucleic acids in vivo. DNA and Cell
Biollogy, v.21, n.12, Dec, p.857-67. 2002.
Solans, C., P. Izquierdo, et al. Nano-emulsions. Current Opinion in Colloid & Interface
26
REFERÊNCIAS BIBLIOGRÁFICAS
Science, v.10, n.3-4, p.102-110. 2005. Strachan, T. e A. P. Read. Genética Molecular
Humana. Porto Alegre: Atmed. 2002
Tamilvanan, S. Oil-in-water lipid emulsions: implications for parenteral and ocular
delivering systems. Progress in Lipid Research, v.43, n.6, p.489-533. 2004.
Teixeira, H., C. Dubernet, et al. Cationic emulsions improves the delivery of
oligonucleotides to leukemic P388/ADR cells in ascite. Journal of Controlled Release,
v.89, n.3, p.473-482. 2003.
______.
Submicron
Cationic
Emulsions
as
a
New
Delivery
System
for
Oligonucleotides. Pharmaceutical Research, v.V16, n.1, p.30-36. 1999.
______. Factors influencing the oligonucleotides release from O-W submicron cationic
emulsions. Journal of Controlled Release, v.70, n.1-2, p.243-255. 2001.
Teixeira, H., V. Rosilio, et al. Characterization of oligonucleotide/lipid interactions in
submicron cationic emulsions: influence of the cationic lipid structure and the presence
of PEG-lipids. Biophysical Chemistry, v.92, n.3, p.169-181. 2001.
Tros De Ilarduya, C., Y. Sun, et al. Gene delivery by lipoplexes and polyplexes. Eur J
Pharm Sci, v.40, n.3, Jun 14, p.159-70. 2010.
Verissimo, L. M., L. F. Lima, et al. Pharmaceutical emulsions: a new approach for gene
therapy. J Drug Target, v.18, n.5, Jun, p.333-42. 2010.
Verma, I. M. e M. D. Weitzman. GENE THERAPY: Twenty-First Century Medicine.
Annual Review of Biochemistry, v.74, p.711-38. 2005.
Wasungu, L. e D. Hoekstra. Cationic lipids, lipoplexes and intracellular delivery of
genes. J Control Release, v.116, n.2, Nov 28, p.255-64. 2006.
Wattiaux, R., N. Laurent, et al. Endosomes, lysosomes: their implication in gene
transfer. Advanced Drug Delivery Reviews, v.41, n.2, Mar 30, p.201-208. 2000.
27
REFERÊNCIAS BIBLIOGRÁFICAS
Wong, G. K. e A. T. Chiu. Gene therapy, gene targeting and induced pluripotent stem
cells: Applications in monogenic disease treatment. Biotechnol Adv, Jul 22. 2010.
Yi, S. W., T. Y. Yune, et al. A cationic lipid emulsion/DNA complex as a physically
stable and serum-resistant gene delivery system. Pharmaceutical Research, v.17, n.3,
Mar, p.314-20. 2000.
Zhang, S., Y. Xu, et al. Cationic compounds used in lipoplexes and polyplexes for gene
delivery. J Control Release, v.100, n.2, Nov 24, p.165-80. 2004.
28
______________________________
Capítulo 4
Artigos Derivados da Tese
______________________________
ARTIGOS DERIVADOS DA TESE
4. ARTIGOS DERIVADOS DA TESE
A seguir serão apresentados os quatro artigos derivados da tese, submetidos para
periódicos na área.
O primeiro artigo intitulado - Pharmaceutical emulsions: a new approach for
gene therapy foi publicado no Journal of Drug Targeting; o segundo artigo encontrase em redação e intitula-se - Cationic nanoemulsions as a possible strategy for gene
delivery in the treatment of xeroderma pigmentosum: preliminary studies; o terceiro
artigo intitulado - Physicochemical and in vivo evaluation of liposomes recovered by
Hyaluronic Acid for targeting CD44 receptor of retinal cellules também está em fase de
redação; e finalmente, o quarto artigo intitulado - Microglia/macrophages migrate
through retinal epithelium barrier by atranscellular route: involvement in diabetic
retinopathy. Role of PKCζ in microglia/macrophages trafficking during diabetic
retinopathy in Goto Kakizaki rats, fruto de uma colaboração com o grupo
Physiopathology of ocular diseases: Therapeutic innovations, Paris, France, liderado
pela Professora Dra. Francine Behar-Cohen, aceito pelo The American Journal of
Pathology, encontra-se nos anexos finais por não se tratar do objeto principal da tese.
30
______________________________
Artigo publicado no Journal of Drug Targeting
______________________________
ARTIGOS DERIVADOS DA TESE
4.1 PHARMACEUTICAL EMULSIONS: A NEW APPROACH FOR GENE
THERAPY
Lourena Mafra Verissimo1
Lucymara Fassarela Agnez Lima2
Lucila Carmem Monte Egito2
Anselmo Gomes de Oliveira3
E. Sócrates Tabosa do Egito1
1
Universidade Federal do Rio Grande do Norte (UFRN), Laboratório de Sistemas
Dispersos (LASID), Natal/RN, Brazil
2
UFRN, Departamento de Biologia Celular e Genética, Laboratório de Biologia
Molecular e Genômica (LBMG), Centro de Biociências, Natal/RN, Brazil
3
Departamento de Fármacos e Medicamentos, Faculdade de Ciências Farmacêuticas,
UNESP, Araraquara, São Paulo, Brasil.
* Corresponding author:
Prof. E. Sócrates Tabosa do Egito
Rua Praia de Areia Branca, 8948, Nata-RN – 509094-450, Brazil.
Fone: 55 84 9431 8816
Fax: 55 84 3215 4346
E-mail: [email protected] or [email protected]
32
ARTIGOS DERIVADOS DA TESE
ABSTRACT
The concept of gene therapy involves the experimental transfer of a therapeutic gene
into an individual’s cells and tissues to replace an abnormal gene aiming to treat a
disease, or to use the gene to treat a disease just like a medicine, improving the clinical
status of a patient. The achievement of a foreigner nucleic acid into a population of cells
requires its transfer to the target. Therefore, it is essential to create carriers (vectors) that
transfer and protect the nucleic acid until it reaches the target. The obvious
disadvantages of the use of viral vectors have directed the research for the development
of a nonviral organized system such as emulsions. In fact, recently, there has been an
increase of interest in its use in biotechnology as a nonviral vector for gene therapy.
This review focuses on the progress of cationic emulsions and the improvement of the
formulations, as a potential delivery system for gene therapy.
Keywords: Cationic emulsions; gene transfection; gene therapy; carrier systems;
delivery systems
33
ARTIGOS DERIVADOS DA TESE
INTRODUCTION
The aim of gene therapy is to modify the genetic material of living cells for
therapeutic purposes. The experimental procedure involves the insertion of a functional
gene into a cell to achieve a therapeutic effect (Verma, 2000). This process is commonly
called transfection. Transfection intends basically to replace, amplify, suppress, or
correct a defective gene, promoting either a cure or a slowdown of the progression of a
disease. In fact, the transfection process permits the selective introduction of a genetic
material for protein synthesis as well as its selective inhibition (antisense or gene
silencing) (Sokolova & Epple, 2008). The development of recombinant DNA
technology, including the ability to clone disease-related genes, the development of
efficient techniques for transfection into cells, the huge interest of an understanding of
the mechanism regulating gene expression, and the ethical reflection about early human
experiments were responsible for the appearance of the concept of gene therapy
(Verma, 2000; Nienhuis, 2008). Q11However, the beginning of gene therapy faced
several failures and deceptions because of the little knowledge about gene diseases,
inefficient techniques for transfection, and ethical problems (Walters, 1991;
Friedmann,1990, 1992).
The more representative experimental gene therapy dates from the 1980s. In this
experiment, lymphocytes of patients carrying Severe Combined Immunodeficiency
Disease (SCID) were treated with a retroviral vector containing the adenosine
desaminase (ADA) gene. The ADA expression was restored (Friedmann, 1992; Berns,
2004). However, five patients developed leukemia as a consequence of insertional
mutagenesis. These leukemia cases have been reported as an insertional activation of a
cellular proto-oncogene (LMO2 gene in the majority of patients) by integrated retroviral
vectors that represented the initiating event for tumorogenesis (Raper, 2005; Staal et al.,
2008). Thus, it seems clear that the use of an efficient and safe vector system to carry
nucleic acid-based medicines is the determinant factor for the successful application of
this promising therapeutic strategy (Staal et al., 2008). The vectors derived from
retroviruses utilize only the transcriptional promoter regions of these viruses (the LTRs)
to direct the gene expression. The main advantage of retroviral-based vectors is the
expression that occurs in most cell types. However, the problems associated with the
use of viral vectors, mainly those related to safety aspects, have prompted investigators
34
ARTIGOS DERIVADOS DA TESE
to develop alternative methods for gene delivery (Niidome & Huang, 2002; Armelini et
al., 2005).
Currently, the importance of nanotechnology in delivery systems has been
continuously demonstrated and has been extensively used as a carrier not only for the
pharmacological active compounds, but also for gene delivery (Egito et al., 1994, 1996,
2004; Bessis, Garcia Cozar, & Boissier, 2004). Moreover, the conclusion of the
―Human Genome Project‖ prompted the hope of new opportunities for gene therapy,
keeping this field as a great novel potential therapeutic modality (Verma& Gage, 2000).
Advances against many of the inherited and acquired diseases were targeted for gene
therapy, including metabolic diseases (Brunetti-Pierri & Lee, 2005); cancer (Cross &
Burmester, 2006; Morille et al., 2008); genetic disorders, such as hemophilia (Roth et
al., 2001) and cystic fibrosis (Hara et al., 1997); immunologic disorders; infectious
diseases, including AIDS; neurological disorders; and various muscle diseases (Raper,
2005; Nienhuis, 2008).
Several viral and nonviral vectors are currently under investigation. Although
viral systems are highly efficient in transfection, the serious side effects related to its
safety, as well as the host immune and inflammatory responses, have limited its use in
clinical applications. On the other hand, nonviral systems, in which plasmid DNA or
oligonucleotide can be complexed with cationic liposomes, polymers, peptides, cationic
emulsions, or other carriers, provide an attractive alternative route for gene delivery
(Kim et al., 2002). Furthermore, gene therapeutics composed of artificial reagents can
be standardized and regulated or safety use. However, each of the gene delivery
strategies has its own advantages and disadvantages. Table 1 shows the main
advantages and disadvantages of some gene vectors.
The obvious disadvantages of the use of viral vectors have directed the research
for the development of a nonviral organized system such as emulsions. In fact, recently,
there has been an increase of interest in its use in biotechnology as a nonviral vector for
gene therapy. This review focuses on the progress of cationic emulsions and the
improvement of the formulations, as a potential delivery system for gene therapy.
35
ARTIGOS DERIVADOS DA TESE
GENE DELIVERY SYSTEMS
Because of their strong negative charge, nucleic acids (DNA, RNA, and
oligonucleotides) alone are not able to penetrate the cell wall in a concentration range
necessary for gene therapy. Therefore, efficient carriers are necessary to introduce them
into the cells. Nanoparticles, which represent any particles with a diameter below the
micron, by their small size, can easily deliver biomolecule drugs into living systems,
usually for a therapeutic purpose (Sokolova & Epple, 2008). Gene delivery systems are
generally divided into two categories: viral and nonviral.
Viral vectors
Viral systems work by the same mechanisms as natural viruses that cause
infectious diseases. They are the most effective but rather dangerous method because of
the risk of recombination, leading to the generation of viruses capable of replication. In
spite of that, the knowledge that some viruses integrate their genetic information into
the genomes of infected cells suggested that it would be possible to mimic the
transformation of cells by these agents to design and construct virus-like particles that
could serve as vectors for introducing therapeutic normal genes into defective cells,
restoring their normal activity. The use of viruses as gene carriers exploits their ability
to deliver genes to the nucleus of a cell and their expression through integration into the
host genome. These recombinant viruses are genetically modified to eliminate their
pathogenicity while retaining their infectivity (Verma &Weitzman, 2005).
The viral vector is the oldest method used for transfection and was first
demonstrated in 1952, by Zinder and Lederberg on a Salmonella model (Zinder
&Lederberg, 1952). With that method, gene therapy was carried out using retroviral
vectors (Friedmann, 1990, 1992). More recently, adenovirus (Armelini et al., 2005),
adeno-associated (Hendrie & Russell, 2005), and herpes virus (Glorioso, DeLuca, &
Fink, 1995) and other viruses have been introduced as viral vectors for gene therapy
(Verma & Weitzman, 2005).
Though most of the studies in the gene therapy field are related to viral vectors,
they present several safety problems. The limited size of the nucleic acid that can be
packaged, the possible recombination of the viral vector with DNA sequences in the
host cell, and the high cost and the high toxicity and immunogenicity are the major
disadvantages related to viral vectors (Wagner, 2008). Inflammatory response and
36
ARTIGOS DERIVADOS DA TESE
carcinogenicity were also attributed to such delivery system (Burand, Summers, &
Smith, 1980; Crystal, 1995; Tripathy et al., 1996; Bessis, Garcia Cozar, & Boissier,
2004). At present, there are nonviral-based vectors which would be safe and efficient on
gene transfection for therapeutical use (Schatzlein, 2001). Therefore, alternative systems
such as hybrid viral vectors (Wagner, 2008), hybrid viral/nonviral vectors, like
magnetic cationic liposomes and retrovirus (Ito et al., 2009), and other innovative
techniques, such as small interfering RNA (siRNA) (Watanabe et al., 2007; Buyens et
al., 2009), transposons, genetic insulators, and new nonviral vectors, are being explored
(Friedmann, 1990,1992; Smyth Templeton, 2002).
Nonviral vectors
Despite the great advances in knowledge of the genetic constitution of man and
the methodologies for gene manipulation, the clinical application of gene therapy
presents several problems in the technical field. It is, therefore, important that more
efforts should be directed toward research and development of new carrier systems that
are safe and able to improve the gene therapy efficiency.
Although most of the clinical trials have been based on the use of viral vectors,
nonviral vectors, including liposomes (Rivest et al., 2007), polyplexes (Niidome &
Huang, 2002), nanoparticles (Li & Szoka, 2007; Roy, Stachowiak, & Bergey, 2008),
magnetic liposomes (Zheng et al., 2009), and nanoemulsions (Martini et al., 2008), in
spite of their lower efficiency in gene transfer than viral systems, are emerging as
promising nonviral carriers for genetic medicines due to their safety and
versatility(Brown, Schätzlein, & Uchegbu, 2001; Montier et al., 2008). In particular,
lipid emulsion formulations are considered to be superior to others due to the fact that
they can be produced on an industrial scale, are stable during storage, and are highly
biocompatible (Hashida, Kawakami, & Yamashita, 2005). These systems can form
complexes electrostatically with anionic genetic materials and are designed as a
nanosized assembly with the genetic material, with some residual positive charge
(Formiga et al., 2007; Nam et al., 2009). DNA compaction is a general phenomenon in
the presence of multivalent ions and positively charged surfaces; because of the high
charge density, there are strong attractive ion correlation effects (Dias et al., 2002;
Miguel et al., 2003; Dias et al., 2004; Höbel & Aigner, 2009). Cationic lipids promote
the condensation of the negatively charged DNA into a more compact structure, capable
of crossing biological membranes. These modifications have greatly reduced the
37
ARTIGOS DERIVADOS DA TESE
chances of enzymatic degradation of the genetic materials in complexes and are in most
cases readily taken up by cells (Miguel et al., 2003; Roy, Stachowiak, & Bergey, 2008;
Nam et al., 2009).
Gene transfection into target cells using naked DNA, which is a simple and safe
approach, has been improved by combining several physical techniques, for example,
electroporation, gene gun, microinjection, ultrasound, and hydrodynamic pressure
(Niidome & Huang, 2002). These methods, however, present several drawbacks. For
example, electroporation is a safe, easy, and rather efficient method, but it needs a large
amount of DNA and has to be optimized for every cell type. Microinjection allows only
one cell at a time to be transfected and is therefore not feasible for a whole organism.
Using the gene-gum technique, a shallow penetration of DNA into the tissue s
accomplished (Sokolova & Epple, 2008).
The current paradigm for designing nonviral systems is to obtain formulations
that may be able to mimic proteins and virus properties, which allow them to be
delivered to the target cell and traverse the cellular membrane to enter the cytoplasm
(Wolff & Rozema, 2008). Two major pathways for the entry of the nucleic acids into
the cells are endocytosis (Wolff & Rozema, 2008) and direct fusion (Smyth Templeton,
2002). A recent approach concerning the development of nanocarriers is
nanotechnology. This method uses the electrostatic attraction between negatively
charged nucleic acid and cationic vectors. These nanoparticle assemblies, by their size,
are easily taken up by cells using endocytosis (Thierry et al., 1997, 2009).
Concerning gene therapy, many different kinds of nanoparticles are known.
Recently, Sokolova and Epple (2008) have reviewed the use of inorganic nanoparticle
as carriers of nucleic acids into cells. The inorganic materials used for DNA delivery
comprise calcium phosphate, carbon nanotubes, silica, gold, magnetite, quantum dots,
strontium phosphate, magnesium phosphate, manganese phosphate, and double
dydroxides (anionic clays) (Sokolova & Epple, 2008). On the other hand, a huge
amount of literature on bio-organic nanoparticle systems such as polycationic (Honget
al., 2006; Srinivasachari, Fichter, & Reineke, 2008), liposomal agents (Templeton,
2002) and dendrimers (Haensler & Szoka, 1993; Ardoin & Astruc, 1995; Tang,
Redemann, & Szoka, 1996; Malik et al., 2000; Guillot-Nieckowski, Eisler, & Diederich,
2007) can currently be found.
Lipid-based carriers have attracted increasing scientific and commercial interest
during the last few years as an alternative for the delivery of nucleic acids (DNA,
38
ARTIGOS DERIVADOS DA TESE
oligonucleotide, or RNA) due to their simplicity, unlimited size of nucleic acid to be
packaged, non immunogenicity, low toxicity, stability, and commercial availability (Liu
et al., 1996; Smyth Templeton, 2002; Rawat et al., 2008). Nevertheless, the efficiency
of transfection with nonviral systems is relatively low and each formulation has its
distinct problem regarding stability, efficacy, or toxicity (Barut, Coskun Ari, & Oner,
2005). Reduced transfection could be due to the instability of the genetic material into
the cell because of its degradation and low availability resulting from multiple targeting
or the chemical properties of delivering molecules (Roy, Stachowiak, & Bergey, 2008).
Some strategies have been used to optimize synthetic vectors, such as the incorporation
of targeting and shielding molecules into the carrier formulations for enhanced and
more specific performance, or empirical screening of various cationic lipids and
polymers which results in greatly improved formulations with high gene transfer
efficiency and low cytotoxicity (Morille et al., 2008; Wagner, 2008).
Recently, alternative experiments involving the association of plasmid DNA or
oligonucleotides with colloidal carrier systems, such as lipid carriers, microspheres and
nanospheres (Masotti & Ortaggi, 2009), nanoparticles, and magnetic systems (Namdeo
et al., 2008) have drawn attention to gene and immunogene delivery (Wolff &Rozema,
2008). Particularly, emulsion-mediated transfection has attracted increasing attention,
and several reports demonstrating the potential of positively charged emulsion particles
as a new delivery system for gene therapy have been published over the past few years
Barut, Coskun Ari, & Oner, 2005).
The drawbacks of liposomes
The majority of the experiments with nonviral systems include liposomes.
Cationic liposome/DNA complexes, named lipoplexes, have been extensively
investigated and widely used in gene therapy to deliver DNA into mammalian cells,
owing to their potential advantages over viral vectors, such as their safety, versatility
and low immunogenicity (Masotti et al., 2009). Over the last years, various
improvements on the development of liposomes for gene delivery, including synthesis
of new cationic lipids and design of new plasmid constructs, have been made, turning
liposomes into a successful gene carrier. Some works detail the process of gene therapy
including the transfection method, the mechanism of gene transfer, the formation of the
cationic lipid/DNA complex, the entry of cationic lipid/DNA complex into cells, the
endosomal escape, the cytoplasmic delivery of nucleic acids, the entry of DNA into the
39
ARTIGOS DERIVADOS DA TESE
nucleus, and nuclear transcription (Smyth Templeton, 2002; Zhang et al., 2004;
Armelini et al., 2005; Lonez, Vandenbranden & Ruysschaert, 2008). Cohen and coworkers (2009), for example, have recently shown, in a study about quantification of
plasmid DNA copies in the nucleus after lipoplex and polyplex transfection, the
importance of considering the processes downstream from nuclear entry for strategies to
improve the efficiency of gene transfer reagents. Additionally, Lentacker and
coworkers, have evaluated new strategies for DNA to conquer cellular and nuclear
membranes, and suggested the use of NAN (nucleic acid containing nanoparticles)
loaded microbubbles and trans-cyclohexane-1,2-diol to induce nuclear uptake of
plasmid DNA (Lentacker et al.,2008). On the other hand, although surface modified
lipoplexes, in which poly(ethylene glycol) monolaurate was inserted into the liposome
surface, presented good tumor regression in mice (Sonoke et al., 2008), a strong
reduction in both the DNA condensation and cell transfection efficiency was also
demonstrated (Bombelliet al., 2007).
It was demonstrated that lipoplexes display different toxicities and transfection
efficiencies depending on their formulation, their size, and the ratio between their lipid
components (charge ratio) (Callow et al., 2009; Masottiet al., 2009). Besides, the
instability of the lipoplex is the main obstacle of this system. One of the major
drawbacks of liposomal formulations is that the lipoplexes are not stable with frequent
and rapid formation of aggregates and flocculates (Zelphati et al., 1998). It is necessary,
therefore, to prepare the complex freshly and use it within a short period of time.
Another important drawback is that, in general, liposomal carriers with cationic
property tend to interact with anionic or amphiphilic blood components and form large
aggregates, resulting in accumulation at the capillary bed of the lung. Owing to their
rapid clearance, liposome/DNA complexes may need to be repeatedly administrated in
order to keep the expression level constant in vivo (Nam et al., 2009). In addition, serum
proteins can decrease transfection efficiency by neutralization of the positive zeta
potential, and by binding to and increasing the particle size of the complexes. The
toxicity may, in part, result from the large size of the complexes, and the high positive
zeta potential required for their uptake. The toxicity is normally closely associated with
the charge ratio between the cationic lipid species and the nucleic acids, as well as the
dose of lipoplexes administered. Higher charge ratios are generally more toxic to a
variety of cell types. In addition, different reagents have different degrees of toxicity to
cells, and toxicity is cell-specific (Formiga et al., 2007). It is also known that the
40
ARTIGOS DERIVADOS DA TESE
transfection activity of cationic liposomes is interfered by serum components which
presumably neutralize the unpaired positive charges in the complexes which are
essential for the binding of a lipoplex to the cell surface (Yi et al., 2000).
Concerning the serum sensitivity of cationic lipid mediated transfection, it is
generally believed that the loss of transfection activity of cationic liposomes is due to
the neutralization of the positive charges on the lipoplex. To overcome these problems,
the development of cationic emulsions, which are physically stable and can facilitate the
transfer of genes successfully in vitro and in vivo, is gaining success (Liu et al., 1996;
Zelphati et al., 1998; Kim et al., 2002).
The use of pharmaceutical emulsions, nanoemulsions, and microemulsions
Lipid emulsions are considered to be superior to liposomes mainly in a scalingup point of view. In fact, such carriers not only can easily be produced on an industrial
scale, but also are stable during storage and are highly biocompatible. In addition, they
possess a high solubilizing capacity as far as lipophilic or amphiphilic drugs are
concerned, because lipid emulsions have an oil phase in particulate form and a large
hydrophilic/lipophilic interface, so they can dissolve large amounts of highly lipophilic
and amphiphilic drugs (Kawakami, Yamashita,& Hashida, 2000).
Emulsions, defined as the dispersion of one immiscible liquid in another
stabilized by a third component, the emulsifying agent (Becher, 1965), present in their
composition three components: oil, water, and surfactants. A normal crude emulsion
possesses a droplet size of around 1 μm, which impeaches its use by intra-venous route.
However, with the development of the nanotechnology, new homogenizators were
developed and a new series of emulsions, named then nanoemulsions could be
achieved. Such emulsion systems present a droplet size distribution of around 200 nm.
On the other hand, microemulsions, defined as thermodynamically stable and
isotropically clear to translucid dispersed oil-in-water or water-in-oil systems stabilized
by an interfacial film of surfactant (Aboofazeli & Lawrence, 1993; Ho, Hsiao, & Sheu,
1996; Constantinides, Chaubal, & Shorr, 2008), were discovered in the 1950s and were
largely used by the chemical industry, and later in the pharmaceutical field. Although
named microemulsions, such systems present a droplet-size distribution of around 80
nm, which at the time of their discovery were impossible to evaluate due to the
limitations in the characterization of nanometric systems. The major difference between
nanoemulsions and microemulsions is their surfactant loaded concentration in the
41
ARTIGOS DERIVADOS DA TESE
formulation. In the former, the surfactant content is in order of 2–5%, while the latter
present a concentration of surfactants of around 20–30%. Therefore, nanoemulsion has
been chosen as a potential lipid carrier for gene therapy.
Lipid-based carrier systems represent drug vehicles composed of physiological
lipids, such as cholesterol, cholesterol esters, phospholipids and triglycerides, and offer
a number of advantages, making them an ideal drug delivery carrier (Egito et al., 1996,
2002; Yi et al., 2000; de Araújo et al., 2005; Constantinides, Chaubal, & Shorr, 2008).
Lipid emulsions have also been used to carry proteins and peptides successfully for the
same reason (Rawat et al., 2008). Adding cationic surfactants to these dispersed systems
makes them suitable for gene delivery (Figure 1). The presence of cationic surfactants
causes the formation of positively charged droplets that promote strong electrostatic
interactions between emulsion and the anionic nucleic acid phosphate groups (Barut,
Coskun Ari, & Oner, 2005; Martini et al., 2008; Marty et al., 2009).
The
most
used
cationic
surfactants
are
DOTAP
(1,2-dioleoyl-3-
trimethylammonium propane), DOTMA (2,3-bis (oleyl)oxipropyl-trimethylammonium
chloride), and DC-Chol (3b[N-(N9,N9-dimethylaminoethane)-carbamoyl]cholesterol).
The co-lipid DOPE (dioleoylphosphatidylethanolamine) is largely used to improve the
ability of cationic liposomes and emulsions to transfect cells due to its fusogenic
properties (Zabner, 1997; Kim et al., 2001; Zhang et al., 2004; Armelini et al., 2005;
Hung et al., 2005). This can be partially explained by the fact that the amine group of
DOPE interacts with DNA phosphate groups, thus weakening the binding affinity
between cationic lipids and DNA (Nam et al., 2009).
Based on the current understanding for cationic lipid mediated transfection, it is
essential for nucleic acid molecules to form a complex with the emulsion in order to
enter the cells and express the gene. To form such a complex, nucleic acid molecules
need to bind to the surface of the emulsion particles via electrostatic interactions
between the negatively charged phosphates of nucleic acids and positively charged
cationic lipids (Liu et al., 1996; Nam et al., 2009).
The progress of cationic nano-emulsions
A wide variety of formulation strategies have so far been employed to improve
the cationic nanoemulsions. A cationic oil-in-water nanoemulsion composed of the
soybean oil and the emulsifying agents, cetyltrimethylammonium bromide (CTAB) and
42
ARTIGOS DERIVADOS DA TESE
Pluronic F68, showed suitable stability and efficient protection of a plasmid against
DNAse digestion (Barut, Coskun Ari, & Oner, 2005).
There
is
also
an
increased
interest
in
characterizing
the
nucleic
acid/nanoemulsion complexes in order to better understand the interaction between
them. Recently, a comparison between the two cationic surfactants DOTAP and
oleylamine demonstrated that droplet size and ζ-potential of its nanoemulsions remained
quite similar, regardless of the cationic lipid used. However, the oligonucleotide
adsorption and release profiles from the o/w interface of nanoemulsions were
significantly lower for oleylamine nanoemulsion when compared with DOTAP
nanoemulsion. The reason is probably that oleylamine nanoemulsion presents a more
fluid interface since this lipid presents a monoleyl chain, limiting the anchorage of
oligonucleotide molecules at the interface, while for DOTAP, besides the electrostatic
interaction also presented with oleylamine, the double acyl chains present in its
molecular structure allow a better anchorage ofoligonucleotides, through the additional
hydrophobic effect (Martini et al., 2008).
The
physical
characteristics
and
serum-resistant
properties
of
the
DNA/nanoemulsion complexes suggest that cationic nanoemulsions could be a more
efficient carrier system for gene and/or immune gene delivery than liposomes (Hara et
al., 1997; Barut, Coskun Ari, & Oner, 2005). The fact that transfection is efficient in the
presence of serum is a big advantage when transfection in serum-containing medium is
beneficial, as in ex vivo applications. One of the reasons for the serum-resistant
properties of the cationic lipid nanoemulsion may be the stability of the
nanoemulsion/DNA complex (Yi et al., 2000). Cationic nanoemulsions were also tested
in vivo, with the results showing that these systems are more suitable for gene delivery
than liposomes because of the higher transfection and lower toxicity (Kwon et al.,
2008). Besides, it was observed that cationic lipids, such as CTAB and oleylamine, may
have dramatic effects on both transfection and toxicity level because of their polar and
hydrophobic single-tailed domains resultingin more toxic and less efficient effects than
double-tailed lipids, such as DOTAP (Zhang et al., 2004; Formiga et al., 2007).
Another example of the great in vivo stability of cationic nanoemulsions is
shown in the study conducted by Kim and co-workers (2005). They demonstrated that
nanoemulsion systems were unable to release its plasmid content in the presence of
destabilizers. The complex between DNA and the nanoemulsion was extremely stable
and resistant to the competitive exchange by ananionic proteoglycan, and as a
43
ARTIGOS DERIVADOS DA TESE
consequence, DNA complexed with nanoemulsion was protected from a DNase attack.
They concluded that the stable nanoemulsion/DNA complex provided a necessary
protection against inactivation by mucosal secretions and a higher accessibility of the
active DNA to airway epithelia than did the liposome/DNA complex.
In order to increase the system stability and its transfection activity, cosurfactants were added to cationic nanoemulsions. It was observed that the inclusion of
nonionic surfactants in the formulation resulted in profound effects on the features of
nanoemulsions. The addition of nonionic surfactants could decrease the nanoemulsion–
DNA interaction and affect the transfection activity, depending on the chain length and
the content of poly (ethylene glycol) (PEG) in the surfactant. The introduction of
nonionic surfactants with a branched PEG headgroup, such as Tween 80®, incremented
nanoemulsion stability and prevented the formation of large DNA/nanoemulsion
complexes, probably because of their steric hindrance and the generation of a
hydrophilic surface that may enhance the stability by preventing physical aggregation.
In contrast, surfactant without the PEG headgroup, such as Span 80® did not improve
the stability of these complexes (Kimet al., 2002). The surfaces decorated with PEG
have the resistance to the protein adsorption, owing to its hydrophilicity and large
excluded volume. Therefore, incorporation of PEG derivatives into the cationic lipid
nanoemulsions may prevent them from enzymatic degradation in blood, resulting in
prolonged circulation in blood. Further, the nanoemulsions with hydrophilic surfactant
are taken up slowly by phagocytic cells (Liuet al., 1996; Hara et al., 1997; Kim et al.,
2002; Buyenset al., 2009).
Aiming to diminish the cytotoxicity and improve the efficacy of lipid-based
nanoemulsions for gene therapy, new cationic lipids, such as 6-lauroxyhexylornithinate
and cationic lipids containing imidazolium or pyridinium polar heads and cationic
polymers, such as poly (ethylenimine) (PEI) and poly (L-lysine) (PLL), have been used
in the formulations (Zhang et al., 2004;Formiga et al., 2007).
To achieve efficient drug delivery, it is important to understand the interactions
of nanoemulsion systems with the biological environment, targeting cell surface
receptors, gene release, stability of therapeutic agents, and the molecular mechanisms of
cell signaling involved in the disease pathology under consideration. Consequently,
studies for the optimization of existing systems and for the development of novel
formulations are ongoing (Suri, Fenniri, & Singh, 2007; Morille et al., 2008).
44
ARTIGOS DERIVADOS DA TESE
Another important aspect of the use of nanoemulsion concerns its droplet size.
Some years ago, Takino and co-workers studied the behavior or nanoemulsion systems
on the body and revealed that after intravenous injection, large nanoemulsions,
containing a droplet size diameter of about 280 nm, rapidly disappeared from the blood
and about 60% of the dose was recovered in the liver within 10 min of its intravenous
injection in mice (Takino et al., 1994). On the other hand, nanoemulsions containing a
droplet-size diameter of about100 nm, named small nanoemulsions, showed a reduced
hepatic uptake and a prolonged blood circulation time. The same group made a
pharmacokinetic analysis that revealed that the small nanoemulsion had an 8−100times
smaller organ distribution clearance by the liver, spleen, and lungs and about a four
times greater are under the plasma concentration−time curve (AUC) than the large
nanoemulsion. Single-pass rat liver perfusion experiments have shown that more than
70% of the large nanoemulsion was extracted by the liver, indicating extensive uptake
of the large nanoemulsion during a single passage (Takino et al., 1995). In addition, the
large nanoemulsion was predominantly recovered from liver non parenchymal cells,
including Kupffer cells, and showed a higher accumulation in the non parenchymal
fraction.
Functionalizing nanoemulsions also play an important role in their uptake. For
example, Finkelstein in1979 and Senior in 1982 demonstrated the influence of
sphingomyelin (SM) in the cellular uptake of nanoemulsions. SM is known to stabilize
the membrane structure of liposomes and the addition of SM to liposomes has been
reported to be effective in reducing their clearance by the Reticuloendothelial System
(RES) (Finkelstein &Weissmann, 1979; Senior & Gregoriadis, 1982). On the other
hand, Takino and coworkers also evaluated the influence of SM on the retention time in
the blood circulation of stable nanoemulsions and revealed that SM charged
nanoemulsions presented an uptake clearance in the liver of about four times less than
that of conventional nanoemulsions, suggesting reduced clearance by the RES (Takino
et al., 1994).
45
ARTIGOS DERIVADOS DA TESE
CONCLUDING REMARKS
Gene delivery is a complex process that needs an efficient carrier to go through
each of the cellular steps involved. For this reason, research should focus on the
development f a vector able to overcome the various barriers that it could encounter.
Over the last few years, the interest in the development of cationic nanoemulsions for
gene therapy has been increasing, and optimizing all components of the delivery system
is allowing broad use of cationic nanoemulsion complexes to treat or cure human
diseases or disorders. Nanoemulsion formulations appeared to have more favorable
physical and biological activities than did traditional cationic liposomes as a gene
delivery system in vivo. In fact, nanoemulsions, by their size of around 200 μm, allow
them an efficient uptake though the cell membrane. Also, nanoemulsions can easily
have their surface functionalized for improving their uptake and generating a short-term
cellular interaction, whereas the oil core composition of their interior allows them to be
biodegradable and biocompatible. For therapeutic application of a vector for gene
therapy, not only is the requirement for high transfection efficiency mandatory, but also
the aspects of biocompatibility, long-term biodegradation, and site-selective application
have to be addressed as well. While the transfection efficiency of cationic
nanoemulsions is still lower than that of their viral counterparts, a number of
adjustments could improve this category of carriers, turning them into very promising
systems for gene delivery.
46
ARTIGOS DERIVADOS DA TESE
REFERENCES
Aboofazeli R, Lawrence MJ.(1993). Investigations into the formation
and
characterization of phospholipid microemulsions. 1. Pseudo-ternary phasediagrams of systems containing water lecithin-alcohol-isopropyl myristate. Int J
Pharma, 93(1–3):161–175.
Ardoin N, Astruc D. (1995). Molecular trees—from syntheses towards applications.
Bull De La Societe Chim De France, 132(9):875–909.
Armelini MG, Muotri AR, Marchetto MC, de Lima-Bessa KM,Sarasin A, Menck CF.
(2005). Restoring DNA repair capacity of cells from three distinct diseases by
XPD gene-recombinant adenovirus. Cancer Gene Ther, 12: 389–396.
Barut KD, Coskun Ari FF, Oner F. (2005). Development and characterization of a
cationic emulsion formulation as a potential pDNA carrier system. Turkish Chem,
29: 27–40.
Becher P. (1965). Emulsions, Theory and Practice. New York:Reinhold.
Berns A. (2004). Good news for gene therapy. N Engl J Med, 350:1679–1680.
Bessis N, GarciaCozar FJ, Boissier MC. (2004). Immune responses togene therapy
vectors: influence on vector function and effect or mechanisms. Gene Ther, 11
Suppl 1: S10–S17.
Bombelli C, Faggioli F, Luciani P, Mancini G, Sacco MG. (2007).PEGylated
lipoplexes: preparation protocols affecting DNA condensation and cell
transfection efficiency. J Med Chem, 50:6274–6278.
Brown MD, Schätzlein AG, Uchegbu IF. (2001). Gene delivery with synthetic (non
viral) carriers.Int J Pharm, 229: 1–21.
Brunetti-Pierri N, Lee B. (2005). Gene therapy for inborn errors of liver metabolism.
Mol Genet Metab, 86: 13–24.
Burand JP, Summers MD, Smith GE. (1980). Transfection with baculovirus DNA.
Virology, 101: 286–290.
Buyens K, Demeester J, De Smedt SS, Sanders NN. (2009). Elucidating the
encapsulation of short interfering RNA in PEGylated cationic liposomes.
Langmuir, 25: 4886–4891.
47
ARTIGOS DERIVADOS DA TESE
Callow P, Fragneto G, Cubitt R, Barlow DJ, Lawrence MJ.(2009).Interaction of cationic
lipid/DNA complexes with model membranes as determined by neutron
reflectivity.Langmuir, 25:4181–4189.
Cohen RN, van der Aa MA, Macaraeg N, Lee AP, Szoka FC Jr. (2009).Quantification
of plasmid DNA copies in the nucleus after lipoplex and polyplex transfection. J
Control Release, 135:166–174.
Constantinides PP, Chaubal MV, Shorr R. (2008). Advances in lipid nanodispersions
for parenteral drug delivery and targeting. Adv Drug Deliv Rev, 60: 757–767.
Cross D, Burmester JK. (2006). Gene therapy for cancer treatment: past, present and
future. Clin Med Res, 4: 218–227.
Crystal RG. (1995). Transfer of genes to humans: early lessons and obstacles to success.
Science, 270: 404–410.
de Araújo IB, Damasceno BP, de Medeiros TM, Soares LA,do Egito ES. (2005).
Decrease in Fungizone toxicity induced by the use of Lipofundin as a dilutent: an
in vitro study. Curr DrugDeliv, 2: 199–205.
Dias R, Antunes F, Miguel M, Lindman S, Lindman B. (2002). DNA lipid systems.A
physical chemistry study. Braz J Med Biol Res,35: 509–522.
Dias RS, Pais A, Miguel MG, Lindman B. (2004). DNA and surfactants in bulk and at
interfaces. Colloids Surf A—Physicochem EngAspects, 250(1–3): 115–131.
Egito ES, Araújo IB, Damasceno BP, Price JC. (2002). Amphotericin B/emulsion
admixture interactions: an approach concerning the reduction of amphotericin B
toxicity. J Pharm Sci, 91:2354–2366.
Egito EST, Fessi H, Appel M, Barratt G, Legrand P, Bolard J,Devissaguet JP. (1996). A
morphological study of an amphotericin B emulsion-based delivery system. Int J
Pharm, 145(1–2):17–27.
Egito EST, Fessi H, Appel M, Puisieux F, Bolard J, Devissaguet JP.(1994). New
techniques for preparing submicronic emulsions - application to Amphotericin-B.
STP Pharma Sci, 4(2): 155–162.
Finkelstein MC, Weissmann G. (1979). Enzyme replacement via liposomes. Variations
in lipid compositions determine liposomal integrity in biological fluids. Biochim
Biophys Acta,587: 202–216.
Formiga FR, Fonseca IA, Souza KB, Silva AK, Macedo JP, Araújo IB, Soares LA,
Egito ES. (2007). Influence of a lipophilic drug on the stability of emulsions: an
48
ARTIGOS DERIVADOS DA TESE
importantapproach on the development of lipidic carriers. Int J Pharm,344: 158–
160.
Friedmann T. (1990). The evolving concept of gene therapy. Hum GeneTher, 1: 175–
181.
Friedmann T. (1992). A brief history of gene therapy. Nat Genet,2: 93–98.
Glorioso JC, De Luca NA, Fink DJ. (1995). Development and application of herpes
simplex virus vectors for human gene therapy. Annu Rev Microbiol, 49: 675–710.
Guillot-Nieckowski M, Eisler S, Diederich F. (2007). Dendritic vectors for gene
transfection. New J Chem, 31(7): 1111–1127.
Haensler J, Szoka FC Jr. (1993). Polyamidoamine cascade polymers mediate efficient
transfection of cells in culture. Bioconjug Chem,4: 372–379.
Hara T, Liu F, Liu DX, Huang L. (1997). Emulsion formulations as a vector for gene
delivery in vitro and in vivo. Adv Drug Deliv Rev,24(2–3): 265–271.
Hashida M, Kawakami S, Yamashita F. (2005). Lipid carrier systems for targeted drug
and gene delivery. Chem Pharm Bull,53: 871–880.
Hendrie PC, Russell DW. (2005). Gene targeting with viral vectors.Mol Ther, 12: 9–17.
Ho HO, Hsiao CC, Sheu MT. (1996). Preparation of microemulsions using polyglycerol
fatty acid esters as surfactant for the delivery of protein drugs. J Pharm Sci, 85:
138–143.
Höbel S, Aigner A. (2009). Nonviral delivery platform for therapeutic RNAi: pegylated
siRNA/cationic liposome complexes for targeting of the proto-oncogene bcl-2.
Future Oncol, 5: 13–17.
Hong S, Leroueil PR, Janus EK, Peters JL, Kober MM, Islam MT,Orr BG, Baker JR Jr,
Banaszak Holl MM. (2006). Interaction of polycationic polymers with supported
lipid bilayers and cells: nanoscale hole formation and enhanced membrane
permeability. Bioconjug Chem, 17: 728–734.
Hung CF, Hwang TL, Chang CC, Fang JY.(2005). Physicochemical characterization
and gene transfection efficiency of lipid emulsions with various co-emulsifiers.
Int J Pharm, 289: 197–208.
Ito A, Takahashi T, Kameyama Y, Kawabe Y, Kamihira M. (2009).Magnetic
concentration of a retroviral vector using magnetite cationic liposomes. Tissue
Eng Part C Methods, 15: 57–64.
49
ARTIGOS DERIVADOS DA TESE
Kawakami S, Yamashita F, Hashida M. (2000). Disposition characteristics of emulsions
and incorporated drugs after systemic or local injection. Adv Drug Deliv Rev, 45:
77–88.
Kim TW, Chung H, Kwon IC, Sung HC, Jeong SY. (2001). Optimization of lipid
composition in cationic emulsion as in vitro and in vivo transfection agents.
Pharm Res, 18: 54–60.
Kim TW, Chung H, Kwon IC, Sung HC, Shin BC, Jeong SY. (2005).Airway gene
transfer using cationic emulsion as a mucosal gene carrier. J Gene Med, 7: 749–
758.
Kim TW, Kim YJ, Chung H, Kwon IC, Sung HC, Jeong SY. (2002). The role of nonionic surfactants on cationic lipid mediated gene transfer. J Control Release, 82:
455–465.
Kwon SM, Nam HY, Nam T, Park K, Lee S, Kim K, Kwon IC, Kim J,Kang D, Park JH,
Jeong SY. (2008). In vivo time-dependent gene expression of cationic lipid-based
emulsion as a stable and biocompatible non-viral gene carrier. J Control Release,
128:89–97.
Lentacker I, Vandenbroucke RE, Lucas B, Demeester J, De Smedt SC,Sanders
NN.(2008). New strategies for nucleic acid delivery to conquer cellular and
nuclear membranes. J Control Release,132: 279–288.
Li W, Szoka FC Jr. (2007). Lipid-based nanoparticles for nucleic acid delivery. Pharm
Res, 24: 438–449.
Liu F, Yang J, Huang L, Liu D. (1996). Effect of non-ionic surfactantson the formation
of DNA/emulsion complexes and emulsion mediated gene transfer. Pharm Res,
13: 1642–1646.
Lonez C, Vandenbranden M, Ruysschaert JM. (2008). Cationic liposomal lipids: from
gene carriers to cell signaling. Prog Lipid Res,47: 340–347.
Malik N, Wiwattanapatapee R, Klopsch R, Lorenz K, Frey H,Weener JW, Meijer EW,
Paulus W, Duncan R. (2000).
Dendrimers: relationship between structure and biocompatibility in vitro, and
preliminary studies on the biodistribution of 125I-labelled polyamidoamine
dendrimers in vivo. J Control Release, 65: 133–148.
Martini E, Fattal E, de Oliveira MC, Teixeira H. (2008). Effect of cationic lipid
composition on properties of oligonucleotide/emulsion complexes: Physicochemical and release studies. Int J Pharm,352: 280–286.
50
ARTIGOS DERIVADOS DA TESE
Marty R, N’soukpoé-Kossi CN, Charbonneau D, Weinert CM,Kreplak L, Tajmir-Riahi
HA. (2009). Structural analysis of DNA complexation with cationic lipids.
Nucleic Acids Res, 37:849–857.
Masotti A, Mossa G, Cametti C, Ortaggi G, Bianco A, Grosso ND,Malizia D, Esposito
C. (2009). Comparison of different commercially available cationic liposomeDNA lipoplexes: Parameters influencing toxicity and transfection efficiency.
Colloids Surf B Biointerfaces, 68: 136–144.
Masotti A, Ortaggi G. (2009). Chitosan micro- and nanospheres: fabrication and
applications for drug and DNA delivery. Mini Ver Med Chem, 9: 463–469.
Miguel MG, Pais A, Dias RS, Leal C, Rosa M, Lindman B. (2003). DNA cationic
amphiphile interactions. Colloids Surf A—Physicochem Eng Aspects, 228(1–3):
43–55.
Montier T, Benvegnu T, Jaffrès PA, Yaouanc JJ, Lehn P. (2008). Progress in cationic
lipid-mediated gene transfection: a series of bio-inspired lipids as an example.
Curr Gene Ther, 8: 296–312.
Morille M, Passirani C, Vonarbourg A, Clavreul A, Benoit JP. (2008).Progress in
developing cationic vectors for non-viral systemic gene therapy against cancer.
Biomaterials, 29: 3477–3496.
Nam HY, Park JH, Kim K, Kwon IC, Jeong SY.(2009). Lipid-based emulsion system as
non-viral gene carriers. Arch Pharm Res, 32:639–646.
Namdeo M, Saxena S, Tankhiwale R, Bajpai M, Mohan YM, Bajpai SK.(2008).
Magnetic nanoparticles for drug delivery applications. J Nanosci Nanotechnol, 8:
3247–3271.
Nienhuis A. (2008). The growing clinical impact of gene therapy. Mol Ther, 16: 995–
996.
Niidome T, Huang L. (2002). Gene therapy progress and prospects: nonviral vectors.
Gene Ther, 9: 1647–1652.
Raper SE. (2005). Gene therapy: the good, the bad, and the ugly. Surgery, 137: 487–
492.
Rawat M, Singh D, Saraf S, Saraf S. (2008). Lipid carriers: a versatile delivery vehicle
for proteins and peptides. Yakugaku Zasshi,128: 269–280.
Rivest V, Phivilay A, Julien C, Bélanger S, Tremblay C, Emond V,Calon F.
(2007).Novel liposomal formulation for targeted gene delivery. Pharm Res, 24:
981–990.
51
ARTIGOS DERIVADOS DA TESE
Roth DA, Tawa NE Jr, O’Brien JM, Treco DA, Selden RF; Factor VIII Transkaryotic
Therapy Study Group. (2001). Nonviral transfer of the gene encoding coagulation
factor VIII in patients with severe hemophilia A. N Engl J Med, 344: 1735–1742.
Roy I, Stachowiak MK, Bergey EJ. (2008). Nonviral gene transfection nanoparticles:
function and applications in the brain. Nanomedicine, 4: 89–97.
Schatzlein AG. (2001). Non-viral vectors in cancer gene therapy: principles and
progress. Anticancer Drugs, 12: 275–304.
Senior J, Gregoriadis G. (1982). Stability of small unilamellar liposomes in serum and
clearance from the circulation: the effect of the phospholipid and cholesterol
components. Life Sci,30: 2123–2136.
Smyth Templeton N. (2002). Liposomal delivery of nucleic acids in vivo. DNA Cell
Biol, 21: 857–867.
Sokolova V, Epple M. (2008). Inorganic nanoparticles as carriers of nucleic acids into
cells. Angew Chem Int Ed Engl, 47: 1382–1395.
Sonoke S, Ueda T, Fujiwara K, Sato Y, Takagaki K, Hirabayashi K,Ohgi T, Yano J.
(2008). Tumor regression in mice by delivery ofBcl-2 small interfering RNA with
pegylated cationic liposomes. Cancer Res, 68: 8843–8851.
Srinivasachari S, Fichter KM, Reineke TM. (2008). Polycationic beta-cyclodextrin
―click clusters‖: monodisperse and versatile scaffolds for nucleic acid delivery. J
Am Chem Soc,130: 4618–4627.
Staal FJ, Pike-Overzet K, Ng YY, van Dongen JJ.(2008). Sola dosis facitvenenum.
Leukemia in gene therapy trials: a question of vectors, inserts and dosage?
Leukemia, 22: 1849–1852.
Suri SS, Fenniri H, Singh B. (2007). Nanotechnology-based drug delivery systems.J
Occup Med Toxicol, 2: 16.
Takino T, Konishi K, Takakura Y, Hashida M. (1994). Long circulating emulsion
carrier systems for highly lipophilic drugs. Biol PharmBull, 17: 121–125.
Takino T, Nagahama E, Sakaeda T, Yamashita F, Takakura Y,Hashida M. (1995).
Pharmacokinetic disposition analysis of lipophilic drugs injected with various
lipid carriers in the single pass rat-liver perfusion system. Int J Pharm, 114(1): 43–
54.
Tang MX, Redemann CT, Szoka FC Jr. (1996). In vitro gene delivery by degraded
polyamidoamine dendrimers. Bioconjug Chem,7: 703–714.
52
ARTIGOS DERIVADOS DA TESE
Templeton NS. (2002). Liposomal delivery of nucleic acids in vivo.DNA Cell Biol,
21(12): 857–867.
Thierry AR, Norris V, Molina F, Schmutz M. (2009).Lipoplex nanostructures reveal a
general self-organization of nucleic acids. Biochim Biophys Acta, 1790: 385–394.
Thierry AR, Rabinovich P, Peng B, Mahan LC, Bryant JL, Gallo RC.(1997).
Characterization of liposome-mediated gene delivery: expression, stability and
pharmacokinetics of plasmid DNA. Gene Ther, 4: 226–237.
Tripathy SK, Black HB, Goldwasser E, Leiden JM. (1996). Immune responses to
transgene-encoded proteins limit the stability of gene expression after injection of
replication-defective adenovirus vectors. Nat Med, 2: 545–550.
Verma IM, Gage FH. (2000). Genome and gene therapy. Mol Ther,2: 95.
Verma IM, Weitzman MD. (2005). Gene therapy: twenty-first century medicine. Annu
Rev Biochem, 74: 711–738.
Verma IM. (2000). Gene therapy: beyond 2000. Mol Ther, 1: 493.
Verma IM. (2000). Gene therapy: the need for basic science. Mol Ther,2: 531.
Wagner E. (2008). Converging paths of viral and non-viral vector engineering. Mol
Ther, 16: 1–2.
Walters L. (1991). Human gene therapy: ethics and public policy. Hum Gene Ther, 2:
115–122.
Watanabe T, Umehara T, Yasui F, Nakagawa S, Yano J, Ohgi T,Sonoke S, Satoh K,
Inoue K, Yoshiba M, Kohara M. (2007). Liver target delivery of small interfering
RNA to the HCV gene by lactosylated cationic liposome. J Hepatol, 47: 744–750.
Wolff JA, Rozema DB. (2008). Breaking the bonds: non-viral vectors become
chemically dynamic. Mol Ther, 16: 8–15.
Yi SW, Yune TY, Kim TW, Chung H, Choi YW, Kwon IC, Lee EB,Jeong SY. (2000).
A cationic lipid emulsion/DNA complex as a physically stable and serum-resistant
gene delivery system. Pharm Res, 17: 314–320.
Zabner J. (1997). Cationic lipids used in gene transfer. Adv Drug Deliv Rev, 27: 17–28.
Zelphati O, Uyechi LS, Barron LG, Szoka FC Jr. (1998).Effect of serum components on
the physico-chemical properties of cationic lipid/oligonucleotide complexes and
on their interactions with cells. Biochim Biophys Acta, 1390: 119–133.
Zhang S, Xu Y, Wang B, Qiao W, Liu D, Li Z. (2004). Cationic compounds used in
lipoplexes and polyplexes for gene delivery. J Control Release, 100: 165–180.
53
ARTIGOS DERIVADOS DA TESE
Zheng XL, Lu JP, Deng L, Xiong Y, Chen JM. (2009). Preparation and characterization
of magnetic cationic liposome in gene delivery. Int J Pharm, 366(1–2): 211–217.
Zinder ND, Lederberg J. (1952). Genetic exchange in Salmonella. J Bacteriol, 64: 679–
699.
54
ARTIGOS DERIVADOS DA TESE
FIGURES LIST
FIGURE 1.Cationic emulsion system acting as a carrier for DNA.
55
ARTIGOS DERIVADOS DA TESE
TABLES LIST
TABLE 1.Some advantages and disadvantages of currently used vectors.
56
______________________________
Artigo em Redação
______________________________
4.2 CATIONIC NANOEMULSIONS AS A POSSIBLE STRATEGY FOR GENE
DELIVERY IN THE TREATMENT OF XERODERMA PIGMENTOSUM:
PRELIMINARY STUDIES
Lourena Mafra Verissimo1, 2,3
André Leandro Silva1, 2
Francisco Alexandrino Júnior1, 2
Kattya Gyselle de Holanda e Silva2,3
Lucymara Fassarela Agnez Lima2
Elias Fatal3
E. Sócrates Tabosa do Egito1
1
Universidade Federal do Rio Grande do Norte (UFRN), Laboratório de Sistemas
Dispersos (LASID), Natal/RN, Brazil
2
UFRN, Departamento de Biologia Celular e Genética, Laboratório de Biologia
Molecular e Genômica (LBMG), Centro de Biociências, Natal/RN, Brazil
3
Paris Sud 11 University, UMR CNRS 8612, Pharmacie Galenique, Faculty of
Pharmacy, Châtenay-Malabry, France
* Correspondingauthor:
Prof. E. Sócrates Tabosa do Egito
Rua Praia de Areia Branca, 8948, Natal-RN – 509094-450,Brazil.
Fone: 55 84 9431 8816
Fax: 55 84 3215 4346
E-mail: [email protected] or [email protected]
ARTIGOS DERIVADOS DA TESE
ABSTRACT
Xeroderma Pigmentosum (XP) is an autosomal syndrome characterized by a high
frequency of skin tumors, especially in areas exposed to sunlight, and, occasionally,
developmental and neurological abnormalities. Traditional XP treatment is still
inefficient and therefore, this syndrome has a great potential for the research in gene
therapy. The obvious disadvantages of the use of viral vectors have directed the research
for the development of a nonviral organized system such as cationic nanoemulsions. In
fact, recently, there has been an increase of interest in its use in biotechnology as a
nonviral vector for gene therapy. The aim of this work was to evaluate different
nanoemulsions formulations intended for the use in gene therapy, as a possible strategy
for the treatment of XP. Stearylamine (SA) and 1,2-dioleoyl-3-trimethylammoniumpropane (DOTAP) were used as cationic surfactants and the results show that
nanoemulsions containing DOTAP presents better potential for the use in gene therapy.
However, when dispersed in aqueous phase during the preparation, SA nanoemulsions
increase its DNA compaction capacity, which is essential for the use in gene therapy,
turning these systems also suitable for gene delivery.
Keywords: Gene therapy, cationic nanoemulsions, cationic lipids, xeroderma
pigmentosum.
59
ARTIGOS DERIVADOS DA TESE
INTRODUCTION
Xeroderma Pigmentosum (XP) is a rare human, autosomal-inherited, skin and
neurodegenerative disease in which exposure to sunlight can result in a high incidence
of skin and mucous membrane cancer, including squamous and basal cell carcinomas
and melanomas. It is characterized by photosensitivity, pigmentary changes, premature
skin ageing and malignant tumour development resulting from the defect in DNA repair
[1-3]. This sensitivity is directly related to a defect in the nucleotide excision repair
(NER) of damaged DNA [4]. Despite the fact that skin cancer is one of the most
surgically tractable forms of cancer, XP individuals suffer multiple skin cancers,
including malignant melanoma. Besides surgical removal of individual skin cancers,
sometimes accompanied by reconstructive surgery using unexposed tissue from the
same patient, current therapies only involve isotretinoin or fluorouracil application. The
only topical treatment to date that has shown efficacy in reducing the risk of actinic
keratoses is sunscreen, but this requires very careful and constant pre-treatment. Oral
retinoid therapies are largely experimental and have potentially serious and almost
always inconvenient side-effects [5, 6].
Skin is a highly accessible organ for gene therapy and compared to other tissues, it
offers the advantage of being easily accessible for manipulations and monitoring. In
addition, skin fibroblasts and keratinocytes are interesting candidates for this purpose
since they are well-studied primary cells and are relatively easy to isolate and grow in
vitro, thus permitting self-renovating epithelial transplants by procedures currently used
in the treatment of burns or other cutaneous disorders [5, 7, 8].
The use of gene therapy for the treatment of XP has been investigated using viral
vectors, more specifically, the adenovirus. The most important limitation of the use of
adenovirus vectors for gene correction protocols is that they elicits strong immune
responses in the host. This feature reduces transgene expression in vivo and the
efficiency of repeated vector administration [4, 5]. To overcome the problems related to
viral vectors, nonviral vectors have been developed and special attention has been done
to cationic nanoemulsions [9].
Cationic nanoemulsions have been investigated as non-viral gene carriers in
therapeutic gene delivery due to the disadvantages related to the use of viral vectors
(scale-up control, immunogenicity, oncogenicity and the limited size of nucleic acid that
can be packed). These systems consist of two immiscible liquids containing an oil core
60
ARTIGOS DERIVADOS DA TESE
(natural or semi-synthetic) stabilized by co-surfactants and cationic surfactants, which
are responsible for the positive charge in the droplet surface. The presence of cationic
surfactants allows the complexation with the negatively charged DNA via electrostatic
interactions, resulting in DNA compaction and consequently nanocomplexes formation
of emulsion/DNA [9, 10].
Liposomes has already been tested for cutaneous gene therapy and it was
demonstrated that the topical application of liposomes containing DNA repair enzymes
to sun damaged skin of patients with XP lowered the rate of development of two forms
of these lesions during a year of treatment [6]. However, liposomes usually present
serum sensitivity due to the neutralization of the positive charges on the lipoplex which
is generally related to loss of transfection activity. Therefore, the development of
cationic emulsions, which are physically stable and can facilitate the transfer of genes
successfully in vitro and in vivo, is gaining success [11-13]. In this study, different
cationic nanoemulsion formulations were analyzed as gene carriers using the XPA gene
as an alternative to the use of viral vectors for the treatment of XP syndrome.
MATERIALS AND METHODS
Chemicals
Nanoemulsions were prepared using medium-chain triglycerides (MCT)
Captex® 355 (Abitec, USA); the co-surfactants Sorbian Monoleate (Span 80®) (Sigma,
USA) and poly (oxyethylene sorbitan monooleate) (Tween 80®) (Sigma, USA) and one
of the two cationic lipids: Stearylamine (SA) (Sigma, USA) or 1,2-dioleoyl-3trimethylammonium-propane (DOTAP) (Avanti Polar Lipids, USA).
Plasmid DNA
The plasmid pIRES2-EGFP (Clontech, USA) was kindly provided by Professor
Menck (USP, São Paulo). It expresses the EGFP (Enhanced Green Fluorescent Protein)
under CMV promoter and was used to assess transfection as well as expression
efficiency. The plasmid DNA was amplified using the DH10B strain of Escherichia coli
and the XPA gene (910 pb) was cloned at the restriction site of EcoRI. Plasmid DNA
purity was determined by agarose gel electrophoresis as well as the measurement of
61
ARTIGOS DERIVADOS DA TESE
optical densities (ODs) by Nanovue (GE Health Systems, USA). In all experiments, the
purified plasmid DNA used had a ratio of OD260/OD280 ≥ 1.8.
Nanoemulsions preparation and characterization
The emulsions were produced by the sonication method as previously described
[14]. Three different systems were prepared, a Basic emulsion (BE), a DOTAP
containing emulsion (ED) and a SA containing emulsion (ES). Because SA presents low
solubility in water and oil, two groups of ES were prepared to investigate its
interference on the incorporation in both emulsion phases, aqueous and oil one.
Additionally, the emulsions were prepared by two different ways. SA was incorporated
into the aqueous (ES AP) or oil phase (ES OP), respectively. Table 1 shows the final
composition of all formulations. The mean droplet size, polydispersity index (PI) and ζpotential of the emulsions were determined by photon correlation spectroscopy (PCS)
and electrophoretic mobility, respectively, at 25°C and at an angle of 173° (Malvern
Zetasizer Instrument, England). The samples were adequately diluted in 1mM NaCl
solution for size and ζ-potential measurements. For all experiments, three replicates
were performed in order to determine mean and standard deviation (SD). Morphologic
examination of emulsions containing either SA or DOTAP was performed by means of
transmission electron microscopy (TEM). A drop of nanoemulsion was placed on
cooper electron microscopy grids. Before analysis, the nanoemulsions were stained by a
1% phosphotungstic acid aqueous solution. TEM analysis was performed using a
Philips EM208 (Netherlands) instrument equipped with CCD camera “grand champ
AMT”.
Stability studies
Nanoemulsions and lipoplexes stability studies were performed by the microemultocrit technique [15]. The micro-emultocrit was performed by filling 75% of a
heparin-free capillary tube with each formulation and placing it in a microcentrifuge
(Fanen, São Paulo, SP, Brazil) at 11500g for 10 minutes. After the centrifugation cycle,
the capillary tubes were placed against a microhematocrit scale, and the creaming index
(CI) was directly measured. The creaming was, then, followed by the measurement of
the CI value, which was obtained by the ratio between the cream layer and the total
emulsion layer according to the equation:
%CI = (HC/HO) x 100,
62
ARTIGOS DERIVADOS DA TESE
where HC is the numeric value of the height of the cream layer and HO is the numeric
value of the total height of the emulsion.
Agarose Gel Electrophoresis
The structures of cationic lipid nanoemulsions/DNA complex were examined by
a gel retardation assay to confirm the compact association of plasmid DNA with
cationic lipids. The degree of DNA condensation and restrictive access to ethidium
bromide (EtBr) was assessed using agarose gel electrophoresis and expressed as
cationic lipid nanoemulsion/DNA ratio (C/D) (nmol/μg) and by evaluating the
retardation of DNA migration by fluorescence measurements of EtBr. 8.5 μg of plasmid
were mixed with crescent quantities of nanoemulsions (0.5 to 15.0 μL), which means a
C/D value between 0.07 to 2.02 nmol/μg for ED nanoemulsions, and 0.17 to 5.3
nmol/μg for ES nanoemulsions. The time of complexation was 30 min at room
temperature. The complexes were then loaded onto 0.7% agarose gels containing EtBr
(0.5 mg/ml) at 40 mM Tris acetate and 1mM EDTA gel running buffer. The gel was run
at 80 mV for 60 min. The trapping efficiency of the plasmid to lipid emulsion was
determined as the DNA being no longer accessible to EtBr intercalation. ES
nanoemulsions were analyzed using a higher C/D ratio (25.81 to 129.05 nmol/μg for ES
AP nanoemulsions and 64.52 to 129.05 for ES OP nanoemulsions, respectively) and the
difference between them were also evaluated.
RESULTS AND DISCUSSION
Nanoemulsions characterization
Nanoemulsions were prepared using an O/W method, as previously reported [14].
First, liposomes were produced by sonication of dried lipid thin film in distilled water,
and these were immediately mixed with MCT oil core, followed by sonication. The
nanoemulsions thus produced were well-dispersed and very stable in aqueous solution.
Table 2 shows the results for droplet size, zeta and PI of BE, ED e ES nanoemulsions.
The mean droplet size of emulsions was under 200 nm while the PI varied from 0.169 to
0.244. PI indicates the particle size distribution and the smaller it is, the more consistent
the size distribution of dispersion is. ζ-potential characterizes the surface charge of
particles which is an indicator of the long term stability. ζ-potential absolute values of ≥
30mV represent a stable formulation [16]. The inversion of ζ- potential value of BE
63
ARTIGOS DERIVADOS DA TESE
from negative to positive caused by the addition of both cationic surfactants SA or
DOTAP, confirms that the cationic surfactants are successfully placed on the
of
the
emulsion droplets.
Transmission
interface
electron microscopy investigations
of the oil droplets showed the typical appearance of an O/W emulsion with droplets
displaying a size lower that 200 nm (Figure 1), confirming the PCS experiments. These
results are in agreement with results previously reported for emulsions obtained by
sonication emulsification procedures [17-19].
In order to evaluate the influence of the poor solubility of SA in oil and water, the
cationic surfactant was incorporated separately in the two phases of the ES emulsions,
aqueous (ES AP) or oily phase (ES OP), and the systems were characterized. The
results were compared by the Wilcoxon Test using a significance level of 95% and are
shown in Table 3. The results from the Wilcoxon Test for the two groups of emulsions
(ES AP and ES OP) showed a P value of 0.2500 e 0.6000 for mean particle size and ζpotential, respectively. The high P values obtained by the comparison of mean particle
size and ζ-potential demonstrate that they do not present any significant difference.
Therefore, during the process of preparation of cationic nanoemulsions, SA can be
incorporated in both phases and no difference between their physicochemical aspects
can be observed.
The nanoemulsions described in this study are not only stable, but also welldispersed with a diameter smaller than 200 nm in an aqueous solution. The good physicchemical characteristics of these systems can be related to their compositions. Besides
the cationic surfactants, SA and DOTAP, the presence of non-ionic surfactants has
already been demonstrated to increment the suitability of cationic nanoemulsions for
gene therapy [20]. As a non-ionic surfactant, Tween 80® is used in formulations for
gene therapy because of the ethylene glycol domains in lipid structures are reported to
improve the transfection ability. In addition, Tween 80® was shown to be an effective
surfactant to avoid formation of oil aggregates in emulsions [13, 16]. Concerning the
class of the sorbitans, it was also demonstrated that the use of sorbitan trioleate (Span
85®), as an emulsifier to produce solid lipid nanoparticles for gene delivery, helps to
maintain the stability of oil droplets in emulsions [21]. This may also be applied to Span
80®.
It is important to recognize that the suitability of the cationic systems for gene
delivery is not determined only by one part of the cationic lipid, but by a combination of
them. The characteristics of the hydrophobic head group and their linker segments that
64
ARTIGOS DERIVADOS DA TESE
determine optimal gene transfer depend upon the overall structure of the lipid. DOTAP,
presents a quaternary ammonium head group [–N+(CH3)3] which allows steric
hindrance at the nitrogen atom and electronic effects of substitutions and the presence of
hydrophilic groups, increasing its transfection efficiency [22]. SA nanoemulsions
present a more fluid interface because of its monostearyl chain, which can limit the
anchorage of DNA molecules [23]. The occurrence of an additional contribution of
hydrophobic interactions between oligonucleotides and mixed lipid monolayers
composed of DOTAP/lecithin, as compared to SA/lecithin, due to the presence of
double acyl chains in the DOTAP molecular structure has been previously described
[24]. It is possible that lipids with 1 or 2 hydrocarbon chains decrease the rigidity of
bilayers (lower phase transition temperature) and favor a higher inter-membrane transfer
rate and lipid mixing, resulting in potential disruption of the endosome and consequent
DNA escape from endosomal degradation [22]. The positive charge of the cationic
lipids can provide a superficial charge to the emulsions and further interact with
negatively charged DNA to form cationic lipid nanoemulsion/DNA complexes [16].
Stability studies
Figure 2 shows the results of the micro-emultocrit analyzes. ED, ES AP and ES
OP nanoemulsions and lipoplexes showed a CI of 2%. The same results were found for
the all lipoplexes demonstrating that the addition of DNA into the nanoemulsion
systems does not interfere in their stability. It is known that emulsions are
thermodynamically unstable systems and therefore, one of the most important prerequisites in formulating an emulsion is to maintain its physical stability. It has been a
long-standing aim to formulate stable emulsions with small particles since the
stabilization of emulsion could be achieved by particle size reduction [25]. The longterm physical stability of nanoemulsions (with no apparent flocculation or coalescence)
makes them unique and they are sometimes referred to as “approaching thermodynamic
stability” [26]. However, it is important to analyze the stability of nanoemulsions after
incorporation of actives, especially if they are charged, as nucleic acids, which can
disturb the system. The maintenance of stability of the nanoemulsions evaluated in this
work shows that the stability of these systems are not disturbed by the incorporation of
nucleic acids.
65
ARTIGOS DERIVADOS DA TESE
Agarose Gel Electrophoresis
The capacity of the cationic lipid nanoemulsions to bind DNA was further
evaluated using different cationic lipid nanoemulsion/DNA ratios by agarose gel
electrophoresis. The physical characteristics of the cationic lipid nanoemulsions/DNA
complex were investigated as a function C/D (nmol/μg). The amount of DNA
wasmaintained constant (8.5 μg) and several rates of emulsions (0.5 to 15.0 μL) were
tested, which means a variation of C/D ratio from 0.07 to 5.23 nmol/μg. Figure 3 shows
the results of the first group of emulsions: ED (A) and ES AP (B). As expected, when
the C/D ratio was less than 1, migration of naked plasmid DNA was observed,
indicating a poorly compact structure of the cationic lipid nanoemulsion/DNA complex
[19]. However, no migration of plasmid DNA was observed when 14 μL of the ED
emulsion was added into the 8.5 μg DNA, which means a C/D rate of 1.9 nmol/μg. The
ES AP emulsion could not compact all the DNA content even at a C/D rate of 5.23
nmol/μg (15.0 μL of nanoemulsion). This could be explained by the existence of
additional hydrophobic interactions due to the presence of a double acyl chain in
DOTAP compared to stearylamine. These data are in agreement with others studies [24,
27].
In order to evaluate the complex formation capacity of ES nanoemulsions, a
higher C/D ratio was tested and the difference between ES AP and ES OP were also
evaluated. These results are shown in Figure 4. Concerning ES AP nanoemulsion, when
the lipid nanoemulsion was mixed with the DNA solution, free DNA disappeared when
the C/D was 51.6 nmol/μg (4 μL of nanoemulsion). In the case of ES OP nanoemulsion,
100% of the complexes were formed at a C/D ratio value of 129.0 nmol/μg (10 μL of
nanoemulsion). Free DNA that did not form a complex with the lipid emulsion was
clearly visible at the position of migration of naked DNA at lower complex ratios. At
low emulsion concentrations, a pale fluorescent band was observed, sometimes, in the
well indicating that the cationic lipid nanoemulsion/DNA complex remained in the well
and was stained by EtBr. In some cases, the complex is detected in the agarose gel well
by necked eyes, but the EtBr fluorescence was not detected under UV light. It means
that the cationic emulsion can also condense the plasmid DNA so strong that the
cationic EtBr could not intercalate the base of DNA [28].
The difference between the composition of the systems, as well as the
methodology used to produce them, seems to be very important in the formation of the
complexes and interfere in the DNA compaction ability. Previous studies have found
66
ARTIGOS DERIVADOS DA TESE
diverse C/D ratios, but each one has its own formulation and methodology [13, 21, 2932]. The overall results show the ability of all the emulsions studied in compact DNA,
which is mandatory to a successful transfection. However, they present different
compaction abilities and therefore, different suitability for the use in gene therapy. ED
seems to be the best formulation to be used in gene therapy because of its better
capacity of compact DNA. This can be explained by the presence of the cationic lipid
DOTAP, which has already been noticed to present better interaction with nucleic acids
than SA [23, 33, 34]. Concerning ES nanoemulsions, the ES AP presents better ability
to compact DNA than ES OP, and, therefore, is more suitable for the use in gene
therapy.
CONCLUDING REMARKS
In summary, DOTAP and SA were evaluated as possible core oils for
nanoemulsion formulations as possible carries in the treatment of XP syndrome. Also,
the influence of loading process concerning SA containing nanoemulsions in AP or OP
was evaluated. Our findings suggest that ED nanoemulsions are the most promising
system to be used as gene carrier since it presents suitable physical-chemical properties
(size, ζ-potential and PI), good stability, even after lipoplex formation and higher
capacity of DNA compaction. Concerning ES nanoemulsions, no difference was found
when physical- chemical properties and stability of ES AP and ES OP were compared.
However, the compaction capacity of ES AP is higher than the compaction capacity of
ES OP. Therefore, it is preferable to disperse the SA in the aqueous phase than in oily
phase. It is already known that cationic lipid nanoemulsions/DNA complexes maintain
physical integrity and protect the DNA from enzymatic degradation thus facilitating the
transfer of genes into cells and tissues [35]. Moreover, the next step of this work is to
evaluate the capacity of DNA protection, transfection activity and cytotoxicity of the
systems described in this work.
67
ARTIGOS DERIVADOS DA TESE
REFERENCES
[1] F. M. Butt, J. R. Moshi, S. Owibingire, and M. L. Chindia, J Craniomaxillofac Surg
38 (2010) 534.
[2] M. G. Armelini, K. M. Lima-Bessa, M. C. Marchetto, A. R. Muotri, V. Chigancas,
R. A. Leite, H. Carvalho, and C. F. Menck, Human & experimental toxicology 26
(2007) 899.
[3] J. E. Cleaver, E. T. Lam, and I. Revet, Nat Rev Genet 10 (2009) 756.
[4] A. R. Muotri, M. C. N. Marchetto, L. F. C. Zerbini, T. A. Libermann, A. M.
Ventura, A. Sarasin, and C. F. M. Menck, Human Gene Therapy 13 (2002) 1833.
[5] M. C. N. Marchetto, A. R. Muotri, D. K. Burns, E. C. Friedberg, and C. F. M.
Menck, Proceedings of the National Academy of Sciences of the United States of
America 101 (2004) 17759.
[6] D. Yarosh, J. Klein, A. O'Connor, J. Hawk, E. Rafal, and P. Wolf, Lancet 357
(2001) 926.
[7] F. Jacobsen, J. Mertens-Rill, J. Beller, T. Hirsch, A. Daigeler, S. Langer, M.
Lehnhardt, H. U. Steinau, and L. Steinstraesser, J Biomed Biotechnol 2006 (2006)
26060.
[8] U. R. Hengge, Clinics in Dermatology 23 (2005) 107.
[9] L. M. Verissimo, L. F. Agnez Lima, L. C. Monte Egito, A. G. de Oliveira, and E. S.
do Egito, J Drug Target (2009)
[10] H. Y. Nam, J. H. Park, K. Kim, I. C. Kwon, and S. Y. Jeong, Archives of
Pharmacal Research 32 (2009) 639.
[11] M. A. Liu, B. Wahren, and G. B. K. Hedestam, Human Gene Therapy 17 (2006)
1051.
[12] O. Zelphati, L. S. Uyechi, L. G. Barron, and F. C. Szoka, Jr., Biochimica Et
Biophysica Acta 1390 (1998) 119.
[13] T. W. Kim, Y. J. Kim, H. Chung, I. C. Kwon, H. C. Sung, and S. Y. Jeong, Journal
of Controlled Release 82 (2002) 455.
[14] L. M. Verissimo, in Programa de Pós-Graduação em Biologia Molecular e
Genética Vol. Mestre, Universidade Federal do Rio Grande do Norte, Natal, 2007, p.
56.
[15] J. P. F. Macedo, L. L. Fernandes, F. R. Formiga, M. F. Reis, T. Nagashima, L. A.
L. Soares, and E. S. T. Egito, Aaps Pharmscitech 7 (2006).
68
ARTIGOS DERIVADOS DA TESE
[16] C. H. Liu and S. Y. Yu, Colloids Surf B Biointerfaces 79 (2010) 509.
[17] T. W. Kim, H. Chung, I. C. Kwon, H. C. Sung, and S. Y. Jeong, Pharmaceutical
Research 18 (2001) 54.
[18] Y. J. Kim, T. W. Kim, H. Chung, I. C. Kwon, H. C. Sung, and S. Y. Jeong,
International Journal of Pharmaceutics 252 (2003) 241.
[19] S. M. Kwon, H. Y. Nam, T. Nam, K. Park, S. Lee, K. Kim, I. C. Kwon, J. Kim, D.
Kang, J. H. Park, and S. Y. Jeong, Journal of Controlled Release 128 (2008) 89.
[20] F. Liu, J. Yang, L. Huang, and D. Liu, Pharmaceutical Research 13 (1996) 1642.
[21] C. Olbrich, U. Bakowsky, C.-M. Lehr, R. H. Muller, and C. Kneuer, Journal of
Controlled Release 77 (2001) 345.
[22] S. Bhattacharya and A. Bajaj, Chem Commun (Camb) (2009) 4632.
[23] E. Martini, E. Fattal, M. C. de Oliveira, and H. Teixeira, International Journal of
Pharmaceutics 352 (2008) 280.
[24] H. Teixeira, C. Dubernet, V. Rosilio, A. Laigle, J. R. Deverre, D. Scherman, S.
Benita, and P. Couvreur, Journal of Controlled Release 70 (2001) 243.
[25] H. Chung, T. W. Kim, M. Kwon, I. C. Kwon, and S. Y. Jeong, Journal of
Controlled Release 71 (2001) 339.
[26] K. Bouchemal, S. Briancon, E. Perrier, and H. Fessi, International Journal of
Pharmaceutics 280 (2004) 241.
[27] C. F. Hung, T. L. Hwang, C. C. Chang, and J. Y. Fang, International Journal of
Pharmaceutics 289 (2005) 197.
[28] S. W. Yi, T. Y. Yune, T. W. Kim, H. Chung, Y. W. Choi, I. C. Kwon, E. B. Lee,
and S. Y. Jeong, Pharmaceutical Research 17 (2000) 314.
[29] S. Bhattacharya and S. S. Mandal, Biochimica Et Biophysica Acta-Biomembranes
1323 (1997) 29.
[30] S. J. Eastman, C. Siegel, J. Tousignant, A. E. Smith, S. H. Cheng, and R. K.
Scheule, Biochimica Et Biophysica Acta 1325 (1997) 41.
[31] T. W. Kim, H. Chung, I. C. Kwon, H. C. Sung, B. C. Shin, and S. Y. Jeong,
International Journal of Pharmaceutics 295 (2005) 35.
[32] H. S. Yoo, S. M. Kwon, Y. J. Kim, H. Chung, I. C. Kwon, J. Kim, and S. Y. Jeong,
Journal of Controlled Release 98 (2004) 179.
[33] H. Teixeira, C. Dubernet, F. Puisieux, S. Benita, and P. Couvreur, Pharmaceutical
Research V16 (1999) 30.
[34] H. Teixeira, V. Rosilio, A. Laigle, J. Lepault, I. Erk, D. Scherman, S. Benita, P.
69
ARTIGOS DERIVADOS DA TESE
Couvreur, and C. Dubernet, Biophysical Chemistry 92 (2001) 169.
[35] H. S. Yoo, O. Mazda, H. Y. Lee, J. C. Kim, S. M. Kwon, J. E. Lee, I. C. Kwon, H.
Jeong, Y. S. Jeong, and S. Y. Jeong, Journal of Controlled Release 112 (2006) 139.
70
ARTIGOS DERIVADOS DA TESE
TABLES LIST
Table 1: Emulsions composition: Basic emulsion (BE), DOTAP containing emulsion
(ED) and Stearylamine containing emulsion (ES)
Component
BE
ED
ES
Captex® 355 (MCT)
5.0%(w/w)
5.0%(w/w)
5.00%(w/w)
Span 80®
0.80%(w/w)
0.80%(w/w)
0.80%(w/w)
Stearylamine
--
--
0.16%(w/w)
Tween 80®
1.20%
1.20%
1.20%
DOTAP
--
0.08%
--
Distilledwater
Qsp. 100%
Qsp. 100%
Qsp. 100%
Table 2: Characterization of Basic Emulsion (BE), DOTAP Emulsion (ED) and
Stearylamine Emulsion (ES).
Formulation Size (nm)
Zeta Potential (ζ) (mV)
PI
BE
175± 1
-17± 2
0.244
ED
177 ± 1
+33± 1
0.238
ES
141 ± 3
+48 ± 9
0.169
Table 3: Characterization of Stearylamine Emulsions incorporated in Aqueous Phase
(AP) or Oily (Phase).
Formulation Size (nm)
Zeta Potential (ζ) (mV)
PI
AP
141 ± 3
+48 ± 9
0.201
OP
115 ± 2
+54 ± 2
0.173
71
ARTIGOS
ARTIGOS DERIVADOS
DERIVADOS DA
DA TESE
TESE
FIGURES
LIST
FI
GURES L
I ST
Figure 1.TEM
FIGURE
1.TEMmicrographs
micrographsofofcationic
cationicnanoemulsions
nanoemulsions(A)
(A)DOTAP
DOTAPemulsion
emulsion and
and (B)
(B)
SA emulsion.
emulsion.
SA
(A)
(B)
72
ARTIGOS DERIVADOS DA TESE
Figure 2: Micro-emultocrit results showing creaming rate of nanoemulsions and
lipoplexes.
Creaming Index (%)
% of Creaming
2
1,5
1
Without DNA
0,5
With DNA
0
ED
ES AP
ES OP
Formulation
Figure 3: Agarose gel electrophoresis picture showing DNA compaction of ED (A) and
ES (B) nanoemulsions.
A
B
73
ARTIGOS DERIVADOS DA TESE
Figure 4: Agarose gel electrophoresis picture showing DNA compaction.
(A) ES AP Nanoemulsions - Lane 1 shows the positive control: plasmid [0.46 μg] and
lane 10 shows the negative control: nanoemulsion. Lanes 2 to 9 show the follow ratios
of EC/DNA (nmol/μg): 25.81; 51.62; 64.53; 77.43; 90.34; 103.24; 116.15 and 129.05.
OC: Open circular form; SC: Supercoiled form.
(B) ES OP (B) nanoemulsions - Agarose gel electrophoresis picture showing DNA
compaction of ES OP. Lane 1 shows the positive control: plasmid [0,46μg] and lane 8
shows the negative control: nanoemulsion. Lanes 2 to 7 show the follow ratios of
EC/DNA (nmol/μg): 64.53; 77.43; 90.34; 103.24; 116.15 and 129.05. OC: Open
circular form; SC: Supercoiled form.
(A)
(B)
74
______________________________
Artigo em Redação
______________________________
4.3 PHYSICOCHEMICAL AND IN VIVO EVALUATION OF LIPOSOMES
RECOVERED BY HYALURONIC ACID FOR TARGETING CD44 RECEPTOR
OF RETINAL CELLULES
Lourena Mafra Verissimo1, 2
Chiara Faedo2 Sophie Rey2
E. Sócrates Tabosa do Egito1
Francine Behar-Cohen3
Amelie Bochot2
Elias Fatal2
1
Universidade Federal do Rio Grande do Norte (UFRN), Laboratório de Sistemas
Dispersos (LASID), Natal/RN, Brazil
2
Paris Sud 11 University, UMR CNRS 8612, Pharmacie Galenique, Faculty of
Pharmacy, Châtenay-Malabry, France
3
Centre de Recherche des Cordeliers, Pierre et Marie Curie University, UPMC UMRS
872, Paris, France
* Corresponding author:
Prof. Elias Fattal
University of Paris Sud 11
School of Pharmacy
5 rue JB Clément 92296
Châtenay-Malabry France
Tel: 33146835582 Fax: 33146835946
E-mail: [email protected]
76
ARTIGOS DERIVADOS DA TESE
INTRODUCTION
The eye is a promising target organ for gene therapy because of its unique
features like easy accessibility and convenient methods of direct assessment of visual
function as an effect of therapy. It presents a small volume tissue to be treated, the need
of drug concentration for treatment is low and the diffusion of active products from the
eye into the circulation is minimal. Besides, the eye benefits from a relative immune
privilege, minimizing the potential immune and inflammatory reactions that may follow
the intraocular injection of foreign antigens (1, 2).
Many eye diseases are chronic and progressive, like macular degeneration and
glaucoma, and others are due to genetic mutations, like retinal degeneration. Several
methods of nucleic acids delivery to ocular cells have been investigated. Thought viral
vectors has been widely studied, nonviral vectors for potential gene replacement and
therapy have been developed in order to overcome the drawbacks of viral vectors (3).
Nanocarriers such as polymeric micelles are promising methods of corneal gene
delivery (4, 5) and various nonviral vectors as liposomes and polymers, have been
studied for gene delivery to the retina (1, 6).
All types of nucleic acids have been developed for the treatment of ocular
diseases, mainly infectious and cell proliferative diseases affecting mostly the posterior
segment of the eye. However, to improve the efficiency of such molecules, the use of
controlled and/or targeted delivery systems is surely needed since they allow protection
against degradation, increase the intracellular penetration and permit the long-term
delivery avoiding repeated administrations (7).
Hyaluronan (HA), a multifunctional, high molecular weight glycosaminoglycan,
is a component of the majority of extracellular matrices. It exerts a biological effect by
binding to families of cellular receptors, the hyaladhedrins. Receptor binding activates
signal pathways in endothelial cells leading to proliferation, migration and
differentiation collectively termed angiogenesis (8). It appears to exert its biological
effects through binding interactions with at least two cell surface receptors: CD44 and
receptor for HA-mediated motility (RHAMM). RHAMM and CD44, through
interactions with their ligands, are both important to processes required for the
formation of new blood vessels (9).
It has also been demosntrated in animal models that introduction of reagents
interfering with CD44–ligand interactions can inhibit inflammatory responses, local
77
ARTIGOS DERIVADOS DA TESE
tumour growth and metastatic spread indicating that CD44 may be a potential target for
therapeutic intervention in these disease states (10, 11). Lipoplexes containing a
Hyaluronic acid-dioleoylphosphatidylethanolamine (HA- DOPE) conjugate were
designed to target the CD44 receptor on breast cancer cells (12) and lung cancer cells
(13). They demonstrated that cationic liposomes containing the HA-DOPE conjugate
mediated good transfection on CD44 expressing cell lines in culture.
It has been shown that CD44 receptor and Hyaluronic acid (HA) are both present
on the ocular surface and retina and play an important role in the physiology of corneal
hydration and epithelial regeneration. Besides, the presence of hyaluronan in a
formulation for ocular gene delivery might increase the residence time due to its
mucoadhesive properties (14-17). Therefore, the aim of this study was analyze the
biodistribution of lipoplexes recovered by HA to evaluate the possibility of its use as
gene delivery system for ophthalmic maladies.
MATERIALS AND METHODS
Chemicals
The lipids L-alpha-dioleoylphosphatidylethanolamine (DOPE) and N-[1-(2,3Dioleoyloxy)propyl]-N,N,Ntrimethylammoniummethylsulfate
(DOTAP)
were
purchased from Avanti Polar Lipids (USA). High molecular weight hyaluronic acid
(HA) (1500 KDa) was obtained from Acros Organics (Belgium); while 1-ethyl-3-[3dimethyl)aminopropyl]carbodiimide (EDAC) and molybdenum blue spray reagent 1.3%
were purchased from Sigma-Aldrich (France).
Plasmid
The plasmid pCMV-luc (7.1 Kb) was kindly provided by Professor Renoir
(Université Paris XI, France). It expresses the luciferases protein under CMV promoter
and can also be used to assess transfection as well as expression efficiency. The plasmid
pCMV-GFP (3.4 Kb) was purchased from PlasmidFactory (Germany). It expresses the
EGFP (Enhanced Green Fluorescent Protein) under a CMV promoter and can be used to
assess transfection as well as expression efficiency. It was endotoxin free and presented
research grade.
78
ARTIGOS DERIVADOS DA TESE
Animals
9 months old Lewis rats female were used in this work. These animals were
treated in accordance with the Association for Research in Vision and Ophthalmology
(ARVO). Experimental procedures were submitted and approved by the ethic
committee of Paris Descartes University.
HA-DOPE conjugate synthesis and characterization
HA-DOPE conjugate was synthesized by an adapted protocol previously
described (12). Briefly, 14 mg of HA was dissolved in 5 mL of distilled water and
preactivated for 2 h at 37°C by incubation with 6 mg of EDAC at pH 4 adjusted by
titration with HCl0.1 N. After that, a suspension of DOPE (360 μg) was added to the
HA solution and the pH was adjusted at 8.6with a 0.1 M borate buffer pH 9.4. The
reaction proceeded for 24 h at 37°C.To ensure total elimination of DOPE (as
demonstrated by thin layer chromatography) the mixture was further dialyzed. Dialysis
was carried out using a Spectra/Por regenerated cellulose membrane with a molecular
cutoff of 15,000.Sample volume was 6.0 mL while the volume of the dialysis fluid was
3 L. The dialysis bag was changed 3 times in 24h ensuring elimination of the last traces
of DOPE. Although DOPE is known to self-aggregate, the dilution was such that it
allows total removal of DOPE. The solution containing the HA-DOPE conjugate was
purified by ultrafiltration (MWCO 10 kDa) (Amicon Ultrafiltration, Millipore
Corporate, France). Through this process, the HA-DOPE conjugate was completely
retained over the filter, while EDAC and all other byproducts of the reaction were
washed away. DOPE that did not react with HA was present as very small traces and
was also eliminated during ultrafiltration. These purification methods do not allow
removal of free HA which remained in the solution containing the HA-DOPE
conjugate. The final product was then lyophilized and the reactions were monitored by
TLC using F254 silica gel precoated sheets (Saint- Quentin-Fallavier, France). After
migration of the mobile phase, sheets were exposed to iodine vapors through
molybdenum blue solution (100 mg/100 mL ethanol).
Preparation and Characterization of Liposomes and Lipoplexes
Liposomes were prepared by the hydration film method. Briefly, the lipids (1,2dioleoyl-3-trimethylammoniumpropane
phosphoethanolamine
(DOPE)
and
(DOT AP),
1,2-dioleoyl-sn-glycero-3-
rhodamine-phosphatidylethanolamine
(PE79
ARTIGOS DERIVADOS DA TESE
Rhodamine) dissolved in chloroform were mixed to reach a final lipid mass ratio of
5.0:4.7:0.3 respectively. The chloroform was evaporated under vacuum and the
resulting lipid film was hydrated with milliQ water to a final concentration of 1 and 10
mg/ mL and vortexed for 8 min. In order to prepare HA-DOPE containing liposomes
the conjugate was dissolved in Milli-Q water (1 mg/mL) and added in to the lipid
suspensions in final concentration of 10 % (HA-DOPE/lipid). Plasmid DNA, pCMV-luc
or pCMV-GFP (1 μg), was complexed with plain cationic liposomes or cationic
liposomes containing HA-DOPE at a 2:1 lipid/DNA ratio (w/w) as described above.
After formation, lipoplexes were incubated at room temperature for 30 min in the case
of pCMV-luc. Concerning pCMV-GFP lipoplexes, kinetics studies were made in the
interval time between 30 min and 7 days. The main physicochemical characteristics as
droplet size, polydispersity index (PI) and zeta potential of both, liposomes and
lipoplexes, were then evaluated by photon correlation spectroscopy (PCS) and
electrophoretic mobility, respectively, at 25°C and at an angle of 173° (Malvern
Zetasizer Instrument, England).
In vivo studies
To study the intraocular distribution of liposomes, 10 μl of each cationic
DOTAP/DOPE/PE-Rhodamine liposomes formulation was injected into the vitreous
body of the rats. Eight Lewis rats were anesthetized by intraperitoneal injection of 0.15
mL pentobarbital (5.47 g/100 mL saline). Pupils were dilated by instillation of one drop
of tropicamide 5%. One drop of tetracaine 1% was administered for local anesthesia.
Intravitreal injections (10 μL) were performed in both eyes using sterile syringes fitted
with a 30-gauge needle (Microfine, Becton Dickinson AG, Meylan, France), as
previously described (18). For therapeutic study, 4 groups of rats received one
intravitreal injection of different formulations in both eyes as described in Table 1 and
were sacrificed in day 3 or 7. Immunohistochemistry was used to identify
internalization of liposomes. For sections, rat eyes were enucleated and post-fixed in
4% paraformaldehyde and cryoprotected using sucrose. They were embedded in optimal
cutting-temperature (OCT) compound (Tissue-Tek; Miles Inc., Bayer Diagnostics,
Puteaux, France), frozen in liquid nitrogen and stored at −80 °C. Cryostat frozen
sections (10 μm thick) (Leica CM 3050S, Wetzlar, Germany) were performed and
mounted on gelatin-coated slides for immunohistochemical analysis.
80
ARTIGOS DERIVADOS DA TESE
RESULTS AND DISCUSSION
Liposomes and Lipoplexes were prepared by hydration film method and were
composed by DOTAP/DOPE/PE-Rhod (5.0/4.7/0.3 w/w/w). Four different groups of
formulations (1 or 10 mg of lipids, containing or not 10% of HA-DOPE) were made and
each of them were complexed with pCMV –luc or pCMV -GFP . The results of Size,
Polydispersity Index (PI) and zeta potential of liposomes and lipoplexes are shown in
Table 2 A and B respectively. Liposomes presented a variation of medium size values
between 300 and 500 nm depending on the formulation. The addition of HA-DOPE
conjugate does not highly modify size of formulations but decreases zeta potential
values. This was expected since HA is negatively charge and the conjugate is placed in
the system’s interfaces.
Concerning lipoplexes, it is observed that the addition of plasmid DNA reduces
size, PI and turns zeta potential negative, which was expected because of the negative
charge of DNA. However, there was a difference in size between the ones using pCMVluc as nucleic acid, and the others using pCMV-GFP. Lipoplexes containing pCMV-luc
present a medium size around 250 nm, a PI around 0.250 and zeta potential value
around -25 mV. However, lipoplexes of 10 mg/mL of lipids formed with pCMV-luc
precipitated after complex formation and could not be used for further studies, even
with good results of size, PI and Zeta Potential. pCMV-GFP lipoplexes showed higher
medium size values and PI increased significantly after complexation time of 30
minutes. In order to investigate if the difference between the plasmids studied could
interfere in the complexation time, kinetics studies were made for pCMG-GFP
lipoplexes in one interval of 7 days. Figure 1 shows the results of kinetics studies for
formulations of 1mg/mL of lipids concentration (A) and 10 mg/mL of lipids
concentration (B), both containing HADOPE conjugate. It was observed that after 2
days pCMV-GFP lipoplexes were well formed for both formulations. The higher time
for complex formation between the two plasmids could be explained by the difference
in conformation between them. pCMG-GFP presents a more supercoiled conformation
and therefore, could get more time to form stable complexes.
The design of highly efficient carriers for gene delivery has been approached by
many research groups. These nonviral vectors should be able not only to cure diseases
with genetic defects but also to treat and prevent major chronic diseases such as cancer,
cardiovascular diseases and rheumatoid arthritis. Among the nonviral gene delivery
81
ARTIGOS DERIVADOS DA TESE
systems, cationic liposomes have been widely investigated. Lipoplexes containing a
Hyaluronic acid-dioleoylphosphatidylethanolamine (HA-DOPE) conjugate had already
been designed to target the CD44 receptor on breast cancer (12) and lung cancer cells
(13) and the physical-chemical characteristics showed in this study agree with the
results demonstrated by these previous works.
Because these systems were formulated for ophthalmic administration, we
evaluated size and PI of formulations after dilution in NaCl 0.9%. The results are shown
in Figure 2. It is shown that there is no difference between size and PI after dilution of
formulations in NaCl 0.1 mM or 0.9%. This means that these formulations could be
used in biological fluids without aggregates formation.
In vivo studies of pCMV-luc lipoplexes were carried out using only the
concentration of 1 mg/mL of lipids. It had been demonstrated that liposomes and
lipoplexes containing HA could penetrate into the retina and that inflammation severity
seemed to impact on system stability resulting in the delayed release of Vasoactive
Intestinal Peptide (VIP) turning this system one efficient strategy to obtain a sustained
delivery of VIP in ocular and lymph node tissues (18). In the present study,
immunohistochemistry analysis showed that after 3 and 7 days of incubation in the
animals, the formulations caused high inflammation and destroyed the retina. In order to
evaluate if the inflammation was caused by the endotoxins presented in the plasmid that
was not previously purified, lipoplexes containing pCMV-GFP with high purity and
endotoxin free were evaluated. Figure 3 shows the results of immunohistochemistry for
lipoplexes in a concentration of 1 mg/mL of lipids without HA-DOPE (A), lipoplexes in
a concentration of 1 mg/mL of lipids with HA-DOPE (B), lipoplexes in a concentration
of 10 mg/mL of lipids without HA-DOPE (C), and lipoplexes in a concentration of 10
mg/mL of lipids with HA- DOPE (D). It is observed that all lipoplexes formulations
induced inflammation into the vitreous and that inflammatory cells internalize the
lipoplexes. Therefore, it can be say that inflammation is caused by the formulations and
not by endotoxins present in the pCMV-luc. Comparing the formulations containing or
not HADOPE, it is observed in a qualitatively analysis that HA-DOPE conjugate
decreases the inflammation caused by the lipoplexes, but this could just be confirmed
after quantitative analysis, as counting of inflammatory cells. Because all formulations
caused inflammation, it would be interesting to investigate what could be the reason for
that. Some possibilities could be the charge and toxicity of cationic surfactants or the
residue of solvents.
82
ARTIGOS DERIVADOS DA TESE
CONCLUSIONS
The eye is a good candidate for gene therapy because of its easy accessibility
and the fact that the eye is an immune-privileged site. While recent trends in the
literature show that non-viral chemical routes for ocular gene delivery are being
developed, most of the systems chosen for delivery are not specially designed to
overcome its barriers. The presence of HA and receptor CD44 in ocular surface and
retina promoted the interest in studying the biodistribution of liposomes containing HADOPE conjugate. It was demonstrated that the difference in size and conformation of
plasmids interferes in the complex formed between DNA and lipids. Also, it was
demonstrated that lipoplexes containing pCMV-GFP can be used in a concentration 10
times higher than the lipoplexes prepared with pCMV-luc. This could be interesting
because the amount of liposomes instilled in the eyes of the animals could be lower,
which is more comfortable and less problematic. Unfortunately, all the formulations
caused inflammation in the animals’ eyes and further studies should be made to
investigate the possible reasons of that.
83
ARTIGOS DERIVADOS DA TESE
REFERENCES
1. R. Naik, A. Mukhopadhyay, and M. Ganguli. Gene delivery to the retina: focus on
non-viral approaches. Drug Discov Today 14: 306-15 (2009).
2. C. Andrieu-Soler, R. A. Bejjani, T. de Bizemont, N. Normand, D. BenEzra, and F.
Behar-Cohen. Ocular gene therapy: a review of nonviral strategies. Mol Vis 12: 133447 (2006).
3. C. Bloquel, J. L. Bourges, E. Touchard, M. Berdugo, D. BenEzra, and F. BeharCohen. Non-viral ocular gene therapy: potential ocular therapeutic avenues. Adv Drug
Deliv Rev 58: 1224-42 (2006).
4. K. A. Williamsand D. J. Coster. Gene therapy for diseases of the cornea - a review.
Clin Experiment Ophthalmol 38: 93-103 (2010).
5. J. Hao, S. K. Li, W. W. Kao, and C. Y. Liu. Gene delivery to cornea. Brain Res Bull
81: 256-61 (2010).
6. K. Hironaka, Y. Inokuchi, Y. Tozuka, M. Shimazawa, H. Hara, and H. Takeuchi.
Design and evaluation of a liposomal delivery system targeting the posterior segment of
the eye. Journal of Controlled Release 136: 247-253 (2009).
7. E. Fattal and A. Bochot. Ocular delivery of nucleic acids: antisense oligonucleotides,
aptamers and siRNA. Adv Drug Deliv Rev 58: 1203-23 (2006).
8. J. Gaffney, S. Matou-Nasri, M. Grau-Olivares, and M. Slevin. Therapeutic
applications of hyaluronan. Mol Biosyst 6: 437-43 (2009).
9. R. C. Savani, G. Cao, P. M. Pooler, A. Zaman, Z. Zhou, and H. M. DeLisser.
Differential involvement of the hyaluronan (HA) receptors CD44 and receptor for HAmediated motility in endothelial cell function and angiogenesis. J Biol Chem 276:
36770-8 (2001).
10. C. M. Isackeand H. Yarwood. The hyaluronan receptor, CD44. Int J Biochem Cell
Biol 34: 718-21 (2002).
84
ARTIGOS DERIVADOS DA TESE
11. V. M. Plattand F. C. Szoka, Jr. Anticancer therapeutics: targeting macromolecules
and nanocarriers to hyaluronan or CD44, a hyaluronan receptor. Mol Pharm 5: 474-86
(2008).
12. C. Surace, S. Arpicco, A. Dufay-Wojcicki, V. Marsaud, C. Bouclier, D. Clay, L.
Cattel, J. M. Renoir, and E. Fattal. Lipoplexes targeting the CD44 hyaluronic acid
receptor for efficient transfection of breast cancer cells. Mol Pharm 6: 1062-73 (2009).
13. S. Taetz, A. Bochot, C. Surace, S. Arpicco, J. M. Renoir, U. F. Schaefer, V.
Marsaud, S. Kerdine-Roemer, C. M. Lehr, and E. Fattal. Hyaluronic acid-modified
DOTAP/DOPE liposomes for the targeted delivery of anti-telomerase siRNA to CD44expressing lung cancer cells. Oligonucleotides 19: 103-16 (2009).
14. S. N. Zhu, B. Nolle, and G. Duncker. Expression of adhesion molecule CD44 on
human corneas. Br J Ophthalmol 81: 80-4 (1997).
15. N. P. Liu, W. L. Roberts, L. P. Hale, M. C. Levesque, D. D. Patel, C. L. Lu, and G.
J. Jaffe. Expression of CD44 and variant isoforms in cultured human retinal pigment
epithelial cells. Invest Ophthalmol Vis Sci 38: 2027-37 (1997).
16. L. E. Lerner, D. M. Schwartz, D. G. Hwang, E. L. Howes, and R. Stern. Hyaluronan
and CD44 in the human cornea and limbal conjunctiva. Exp Eye Res 67: 481-4 (1998).
17. M. Hornof, M. de la Fuente, M. Hallikainen, R. H. Tammi, and A. Urtti. Low
molecular weight hyaluronan shielding of DNA/PEI polyplexes facilitates CD44
receptor mediated uptake in human corneal epithelial cells. J Gene Med 10: 70-80
(2008).
18. L. Lajavardi, S. Camelo, F. Agnely, W. Luo, B. Goldenberg, M. C. Naud, F. BeharCohen, Y. de Kozak, and A. Bochot. New formulation of vasoactive intestinal peptide
using liposomes in hyaluronic acid gel for uveitis. J Control Release 139: 22-30 (2009).
19. A. M. Henriques, C. Madeira, M. Fevereiro, D. M. Prazeres, M. R. Aires-Barros,
and G. A. Monteiro. Effect of cationic liposomes/DNA charge ratio on gene expression
and antibody response of a candidate DNA vaccine against Maedi Visna virus. Int J
Pharm 377: 92-8 (2009).
85
ARTIGOS DERIVADOS DA TESE
ARTIGOS DERIVADOS DA TESE
ARTIGOS DERIVADOS DA TESE
T ABL E L EGENDS:
TABLE LEGENDS:
T ABL E L EGENDS:
Table 1: Distribution of animals and formulations for in vivo studies.
Table Table
1: Distribution
of animals
forininvivo
vivo
studies.
1: Distribution
of animalsand
andformulations
formulations for
studies.
Group
Animal
Group
1
2
For mulation
T ime of
For mulation
T ime
of
analysis
Animal
Rat 1
analysis
Day
3
DOPE/DOTAP/PE-Rhod 1 mg/mL
Rat 1
DOPE/DOTAP/PE-Rhod 1 mg/mL
DOPE/DOTAP/PE-Rhod 1 mg/mL
1 Rat 2
Rat 2
DOPE/DOTAP/PE-Rhod 1 mg/mL
Rat 3
Rat 3
Day 3
Day 7
Day 7
DOPE/DOTAP/PE-Rhod 1 mg/mL + HADOPE
Day 3
DOPE/DOTAP/PE-Rhod 1 mg/mL + HADOPE
Day 3
2 Rat 4
DOPE/DOTAP/PE-Rhod 1 mg/mL + HADOPE
Rat 4
DOPE/DOTAP/PE-Rhod 1 mg/mL + HADOPE
3
3
4
4
Day 7
Day 7
RatRat
5 5 DOPE/DOTAP/PE-Rhod
10 mg/mL
mg/mL
DOPE/DOTAP/PE-Rhod 10
RatRat
6 6 DOPE/DOTAP/PE-Rhod
10 mg/mL
mg/mL
DOPE/DOTAP/PE-Rhod 10
Day
Day
3 3
Day
Day
7 7
RatRat
7 7 DOPE/DOTAP/PE-Rhod
10 mg/mL
mg/mL++HADOPE
HADOPE DayDay
DOPE/DOTAP/PE-Rhod 10
3 3
DOPE/DOTAP/PE-Rhod 10
7 7
RatRat
8 8 DOPE/DOTAP/PE-Rhod
10 mg/mL
mg/mL++HADOPE
HADOPE DayDay
Table
2: Characterization
liposomes(A)
(A) and
and lipoplexes
Table
2:2:Characterization
of
liposomes
lipoplexes(B).
(B).
Table
Characterization
ofof
liposomes
(A)
and
lipoplexes
(B).
L iposomes
L iposomes
Size (nm)
PI
Z eta (mV )
526 ± 7
0.291 ± 0.03
+73 ± 2
+39 ± 1
Size (nm)
1 mg/mL Lipids
PI
1 mg/mL Lipids
526 ± 7
436 ± 8
0.279 ± 0.02
1 mg/mL
Lipids with HADOPE
10 mg/mL Lipids
436
±8
334 ± 6
0.445 ± 0.01
10 mg/mL
Lipids
10 mg/mL
Lipids with HADOPE
334±±10
6
402
10 mg/mL Lipids with HADOPE
402 ± 10
(A)
1 mg/mL Lipids with HADOPE
Size (nm)
(A)
L ipoplexes
L ipoplexes
1 mg/mL Lipids
luc
GFP
10 mg/mL Lipids
luc
GFP
0.279 ± 0.02 +77+39
±1
±1
0.445± ±0.01
0.01 +39+77
0.440
± 1± 1
0.440 ± 0.01
+39 ± 1
PI
Z eta (mV )
PIpCM V pCM V -luc
GFP
pCM V -
pCM VZ- eta
pCM(mV
V- )
luc
GFP
pCM V - pCM V -
pCM V -luc
GFP
luc
GFP
0.242 ± 0.02 0.249 ± 0.03 -26 ± 2 -36 ± 2
248 ± 10 319 ± 11 0.218 ± 0.01 0.198 ± 0.02 -25 ± 1 -41 ± 2
231± 11 380 ± 15 0.244 ± 0.02 0.233 ± 0.03 -24 ±3 -57 ± 2
1 mg/mL Lipids with HADOPE 277 ± 12 331 ± 3
10 mg/mL Lipids with HADOPE 258 ± 9
10 mg/mL Lipids
+73 ± 2
248 ± 10 319 ± 11 0.218 ± 0.01 0.198 ± 0.02 -25 ± 1 -41 ± 2
1 mg/mL Lipids with HADOPE 277 ± 12 331 ± 3
1 mg/mL Lipids
0.291 ± 0.03
pCM
V - (nm)
pCM V Size
pCM V - pCM V -
Z eta (mV )
0.242 ± 0.02 0.249 ± 0.03 -26 ± 2 -36 ± 2
383 ± 15 0.254 ± 0.05 0.271± 0.07 -31 ± 1 -55 ± 1
231± 11 380(B)
± 15 0.244 ± 0.02 0.233 ± 0.03 -24 ±3 -57 ± 2
10 mg/mL Lipids with HADOPE 258 ± 9
383 ± 15 0.254 ± 0.05 0.271± 0.07 -31 ± 1 -55 ± 1
(B)
86
ARTIGOS DERIVADOS DA TESE
FIGURE LEGENDS:
Figure 1: Kinetics studies of lipoplexes containing HADOPE (10%) formed by pCMVGFP in concentrations of 1 mg/mL of lipids (A) and 10 mg/mL of lipids (B).
87
______________________________
Capítulo 4
Considerações Finais
CONSIDERAÇÕES FINAIS
5. CONSIDERAÇÕES FINAIS
A Biotecnologia é um ramo muito amplo da Tecnologia que se ocupa da
transformação ou tratamento de materiais de origem biológica onde se insere a terapia
gênica.
Durante os últimos anos, o desenvolvimento de diferentes vetores para o
transporte de genes às células de mamíferos tem despertado um enorme interesse devido
à possibilidade de tratamento de doenças humanas de origem genética. Apesar do
enorme progresso, para que a terapia gênica seja segura e eficientemente aplicada
clinicamente, uma série de problemas técnicos ainda necessita de resolução.
O Sucesso da terapia gênica requer um conhecimento considerável quanto à
natureza da patologia alvo, do período de tratamento, e da segurança e eficiência das
ferramentas de transporte gênico. Um vetor ideal seria aquele que fosse biocompatível,
não imunogênico e estável na circulação sanguínea, protegesse o ADN durante o
transporte, pudesse acomodar um tamanho ilimitado de material genético, fosse
disponível em uma forma concentrada, pudesse ser facilmente produzido, pudesse ser
direcionado para tipos celulares específicos, não permitisse replicação autônoma do
material genético, pudesse garantir uma expressão gênica em longo prazo e fosse nãotóxico. Infelizmente, tal vetor ainda não existe e nenhum dos sistemas de entrega de
DNA atualmente disponíveis para transferência gênica in vivo pode ser aplicado de
maneira universal.
Os vetores não virais mediados por lipídeos catiônicos, como lipossomas e
nanoemulsões catiônicos, são bastante promissores para utilização na terapia gênica e
um grande progresso tem sido alcançado no desenvolvimento destes sistemas no que
concerne o transporte de genes em células de mamíferos em estudos in vivo e in vitro.
Lipossomas e nanoemulsões catiônicas apresentam biocompatibilidade, baixa
toxicidade, e a possibilidade de serem produzidos em larga escala, o que é fundamental
em futuras aplicações clínicas. As características físico-químicas destes sistemas podem
ser controladas variando seus constituintes como lipídeos catiônicos, lipídeos neutros,
cotensoativos, e núcleo oleoso (no caso das nanoemulsões). Além disso, o maior tempo
de circulação ou a vetorização célula-específica destes sistemas podem prolongar sua
circulação sanguínea e melhorar seus efeitos terapêuticos reduzindo os efeitos adversos.
Contudo, os lipídeos catiônicos ainda apresentam alguns problemas como baixa
91
CONSIDERAÇÕES FINAIS
eficiência de transfecção e incompatibilidade sérica quando comparados aos vetores
virais. Alguns fatores como, a composição e arquitetura dos lipídeos, a razão de carga
lipídeo/ADN, os diferentes tipos celulares, força iônica e as estruturas dos lipoplexos
ainda precisam ser otimizados para o sucesso da terapia gênica em ensaios clínicos.
Após atingir a membrana celular, um dos maiores obstáculos é a instabilidade destes
sistemas no citoplasma e conseqüentemente, seu transporte até o núcleo. Logo, ainda
existe uma enorme necessidade de continuação nas pesquisas de desenvolvimento de
vetores eficientes, que possam ajudar os agentes terapêuticos a atravessarem as barreiras
começando pela membrana celular, passando pelo citoplasma até chegar ao núcleo.
Neste trabalho, dois diferentes tipos de vetores não virais, nanoemulsões e
lipossomas catiônicos, foram avaliados. Ambos os sistemas se apresentaram físicoquimicamente adequados possibilitando que os estudos in vitro e in vivo possam ser
realizados posteriormente. No caso das nanoemulsões, as que contêm DOTAP parecem
ser mais eficientes na formação dos lipoplexos. No entanto, os resultados também
apontam que não se pode descartar a utilização da EA como lipídeo catiônico para esta
finalidade. Considerando o segundo tipo de sistema, os lipossomas, observou-se que a
presença do conjugado ácido hialurônico – DOPE (HA-DOPE) na sua interface não
interfere nas suas características físico-químicas, tornando o sistema promissor para
vetorização às células que expressam o receptor CD44 e que estes sistemas apresentam
as características necessárias para administração vitreal.
Apesar dos grandes desafios enfrentados pela pesquisa na área da terapia gênica,
existe uma evolução notável especialmente no que concerne o desenvolvimento de
novos vetores não virais e diferentes formulações que podem ser utilizadas para
tratamento de diferentes tipos de doenças e administrados através das mais diversas
vias.
92
______________________________
Anexo
Trabalhos derivados da tese
TRABALHOS DERIVADOS DA TESE
6. ANEXO
6.1 RESUMOS PUBLICADOS EM CONGRESSOS
1. VERÍSSIMO, Lourena Mafra; JÚNIOR ALEXANDRINO, Francisco; MARTINS,
Alexandre da Silva; SILVA, André Leandro; AGNEZ-LIMA, Lucymara Fassarela;
EGITO, Eryvaldo Sócrates Tabosa Do. DIFFERENCE ON PHYSICOCHEMICAL
PROPERTIES
AND DNA COMP ACTION EFFICIENCY OF NANOEMULSIONS
FOR
THERAPY
GENE
USING
DISTINCT
SURFACTANTS.
In:
70TH
INTERNATIONAL CONGRESS OF FIP, 2010, Lisboa. 70th International Congress of
FIP, 2010.
2. VERISSIMO, L. M.; ALEXANDRINO JÚNIOR, F.; SILVA, A. L.; MARTINS, A.
S.; SILVA, K. G. H.; Silva, G. C.; AGNEZ-LIMA, L.F.; EGITO, E. S. T..
REPRODUCIBILITY
EVALUATION
OF
STEARYLAMINE
CONTAINING
NANOEMULSIONS FOR GENE THERAPY. In: 3rd International NanoBio
Conference, 2010, Zurique, Suiça. 3rd International NanoBio Conference, 2010.
3. VERÍSSIMO, Lourena Mafra; JÚNIOR ALEXANDRINO, Francisco; SILVA, André
Leandro; MARTINS, Alexandre da Silva; SILVA, Acarízia Eduardo; AGNEZ-LIMA,
Lucymara Fassarela; EGITO, Eryvaldo Sócrates Tabosa Do. AVALIAÇÃO DA
CITOTOXICIDADE DE
NANOEMULSÕES
CATIÔNICAS
CONTENDO
ESTEARILAMINA PARA TERAPIA GÊNICA. In: XX CONGRESSO PANAMERICANO DE FARMÁCIA E XIV
CONGRESSO DA FEDERAÇÃO
FARMACÊUTICA SUL-AMERICANA, 2010, Porto Alegre. XX Congresso PanAmericano de Farmácia e XIV Congresso da Federação Farmacêutica Sul-Americana,
2010.
4. VERÍSSIMO, Lourena Mafra; SILVA, André Leandro; JÚNIOR ALEXANDRINO,
Francisco; MARTINS, Alexandre da Silva; AGNEZ-LIMA, Lucymara Fassarela;
EGITO, Eryvaldo Sócrates Tabosa Do. AVALIAÇÃO DA ESTABILIDADE DE
NANOEMULSÕES
PARA
MICROEMULTÓCRITO.
In:
TERAPIA
XX
GÊNICA
CONGRESSO
PAN-
ATRAVÉS
DO
AMERICANO
DE
94
TRABALHOS DERIVADOS DA TESE
FARMÁCIA E XIV CONGRESSO DA FEDERAÇÃO FARMACÊUTICA SULAMERICANA, 2010, Porto Alegre. XX Congresso Pan-Americano de Farmácia e XIV
Congresso da Federação Farmacêutica Sul- Americana, 2010.
5. VERÍSSIMO, Lourena Mafra; SILVA, André Leandro; JÚNIOR ALEXANDRINO,
Francisco; AGNEZ-LIMA, Lucymara Fassarela; EGITO, Eryvaldo Sócrates Tabosa Do.
AVALIAÇÃO QUALITATIVA DA INFLUÊNCIA DO TEMPO NA FORMAÇÃO
DE LIPOPLEXOS PARA TERAPIA GÊNICA. In: II Simpósio Internacional de
Genética Clínica da UFRN, 2010, Natal. II Simpósio Internacional de Genética Clínica
da UFRN, 2010.
6. VERÍSSIMO, Lourena Mafra; SILVA, André Leandro; JÚNIOR ALEXANDRINO,
Francisco; AGNEZ-LIMA, Lucymara Fassarela; EGITO, Eryvaldo Sócrates Tabosa Do.
INFLUENCIA DEL CAMBIO DE LA FASE DE INCORPORACIÓN DE
ESTEARILAMINA EN EL PROCCESO DE COMPLEJACIÓN DEL ADN POR
NANOEMULSIÓN CATIÓNICA. In: 2da Escuela de Nanomedicinas - 1er Simposio
Latinoamericano
de
Nanomedicinas,
2010,
Buenos
Aires.
2da
Escuela
de
Nanomedicinas - 1er Simposio Latinoamericano de Nanomedicinas - Libro de
Resúmenes, 2010. p. 49-50.
7. VERÍSSIMO, Lourena Mafra; SILVA, André Leandro; JÚNIOR ALEXANDRINO,
Francisco; MARTINS, Alexandre da Silva; SILVA, Kattya Gyselle de Holanda e;
BRUXEL, Fernanda L; AGNEZ-LIMA, Lucymara Fassarela; EGITO, Eryvaldo
Sócrates Tabosa Do. INVESTIGATION OF STEARYLAMINE LOADING PROCESS
ON AQUEOUS AND OIL PHASE OF CATIONIC NANOEMULSIONS. In: 2nd
Conference Innovation in Drug Delivery: From Preformulation to Development
Through Innovative Evaluation Process, 2010, Aix en Provence. 2nd Conference
Innovation in Drug Delivery: From Preformulation to Development Through Innovative
Evaluation Process - Programme and Abstracts, 2010.
8. VERÍSSIMO, Lourena Mafra; JÚNIOR ALEXANDRINO, Francisco; SILVA, André
Leandro; ARAÚJO, Ivonete Batista; AGNEZ-LIMA, Lucymara Fassarela; EGITO,
Eryvaldo Sócrates Tabosa Do. THE ROLE OF DOTAP AND STEARYLAMINE ON
THE DNA COMPACTION PROCESS OF CATIONIC EMULSIONS FOR GENE
95
TRABALHOS DERIVADOS DA TESE
THERAPY.
In:
CIFARP
2009
7th
INTERNATIONAL
CONGRESS
OF
PHARMACEUTICAL SCIENCES, 2009, Ribeirão Preto. CIFARP 2009 7th
INTERNATIONAL CONGRESS OF PHARMACEUTICAL SCIENCES, 2009.
9. VERÍSSIMO, Lourena Mafra; SILVA, André Leandro; JÚNIOR ALEXANDRINO,
Francisco; ARAÚJO, Ivonete Batista; AGNEZ-LIMA, Lucymara Fassarela; EGITO,
Eryvaldo
Sócrates
Tabosa
Do.
PRE-VALIDATION
STEP
ON
THE
SPECTROPHOTOMETRIC ANALYSIS FOR NUCLEIC ACIDS. In: CIFARP 2009
7th INTERNATIONAL CONGRESS OF PHARMACEUTICAL SCIENCES, 2009,
Ribeirão
Preto.
CIFARP
2009
7th
INTERNATIONAL
CONGRESS
OF
PHARMACEUTICAL SCIENCES, 2009.
10. VERÍSSIMO, Lourena Mafra; SILVA, André Leandro; JÚNIOR ALEXANDRINO,
Francisco; AGNEZ-LIMA, Lucymara Fassarela; EGITO, Eryvaldo Sócrates Tabosa Do.
INFLUENCE OF THE CATIONIC AGENT OF AN EMULSION SYSTEM
INTENDED FOR GENE THERAPY ON DNA COMPACTION PROCESS. In:
Meeting on Nanotechnology, Liposomes and Health, 2009, Itaparica. Meeting on
Nanotechnology, Liposomes and Health, 2009.
11. AMORIM, Marcelo Vitor de Paiva; VERÍSSIMO, Lourena Mafra; AGNEZ- LIMA,
Lucymara Fassarela; EGITO, Eryvaldo Sócrates Tabosa Do. INFLUENCE OF DOTAP
AND PLASMID DNA ON THE STABILITY OF NANOEMULSIONS FOR GENE
THERAPY. In: I International Symposium in Pharmaceutical Sciences of Northeast
Brazil, 2008, Natal. I International Symposium in Pharmaceutical Sciences of Northeast
Brazil, 2008.
12. EGITO, Eryvaldo Sócrates Tabosa Do; VERÍSSIMO, Lourena Mafra; AGNEZLIMA, Lucymara Fassarela; AMORIM, Marcelo Vitor de Paiva. EVALUATION OF A
NEW EMULSION FORMULATION FOR GENE DELIVERY. In: PSWC 2007
Pharmaceutical Sciences World Congress, 2007, AMSTERDAM. Optimising Drug
Therapy: an imperative for world health, 2007.
13. VERÍSSIMO, Lourena Mafra; AMORIM, Marcelo Vitor de Paiva; AGNEZ- LIMA,
Lucymara Fassarela; EGITO, Eryvaldo Sócrates Tabosa Do. CHARACTERIZATION
96
TRABALHOS DERIVADOS DA TESE
OF A NEW NANOEMULSION FOR GENE DELIVERY. In: CIFARP 6th
International Congress of Pharmaceutical Sciences, 2007, Ribeirao Preto. CIFARP 6th
International Congress of Pharmaceutical Sciences, 2007.
14. AMORIM, Marcelo Vitor de Paiva; VERÍSSIMO, Lourena Mafra; AGNEZ- LIMA,
Lucymara Fassarela ; EGITO, Eryvaldo Sócrates Tabosa Do. PERSPECTIVAS DA
UTILIZAÇÃO DE SISTEMAS EMULSIONADOS PARA TERAPIA GÊNICA. In:
XVIII Congresso de Iniciação Científica da UFRN - CIC 2007, 2007, Natal. XVIII
Congresso de Iniciação Científica da UFRN - CIC 2007, 2007.
15. AMORIM, Marcelo Vitor de Paiva; VERÍSSIMO, Lourena Mafra; AGNEZ- LIMA,
Lucymara Fassarela; EGITO, Eryvaldo Sócrates Tabosa Do. UTILIZAÇÃO DO
MÉTODO DE SONICAÇÃO PARA OBTENÇÃO DE EMULSÕES PARA TERAPIA
GÊNICA. In: IX Congresso Científico da UNP Educação, Ciência e Cultura:
Construindo a Cidadania, 2007, Natal. IX Congresso Científico da UNP Educação,
Ciência e Cultura: Construindo a Cidadania, 2007.
97
TRABALHOS DERIVADOS DA TESE
6.2 ARTIGO PUBLICADO NO JOURNAL OF DRUG TARGETING
Pharmaceutical emulsions: a new approach for gene therapy Lourena Mafra Verissimo,
Lucymara Fassarela Agnez Lima, Lucila Carmem Monte Egito, Anselmo Gomes de
Oliveira, E. Sócrates Tabosa do Egito.
Journal of Drug Targeting Jun 2010, Vol. 18, No. 5, Pages 333-342: 333-342.
Summary:
The concept of gene therapy involves the experimental transfer of a therapeutic gene
into an individual’s cells and tissues to replace an abnormal gene aiming to treat a
disease, or to use the gene to treat a disease just like a medicine, improving the clinical
status of a patient. The achievement of a foreigner nucleic acid into a population of cells
requires its transfer to the target. Therefore, it is essential to create carriers (vectors) that
transfer and protect the nucleic acid until it reaches the target. The obvious
disadvantages of the use of viral vectors have directed the research for the development
of a nonviral organized system such as emulsions. In fact, recently, there has been an
increase of interest in its use in biotechnology as a nonviral vector for gene therapy.
This review focuses on the progress of cationic emulsions and the improvement of the
formulations, as a potential delivery system for gene therapy.
Keywords
Cationic emulsions, gene transfection, gene therapy, carrier systems, delivery system
98
TRABALHOS DERIVADOS DA TESE
TRABALHOS DERIVADOS DA TESE
99
TRABALHOS DERIVADOS
DERIVADOSDA
DATESE
TESE
TRABALHOS
100
TRABALHOS DERIVADOS DA TESE
101
TRABALHOS DERIVADOS
DERIVADOS DA
DA TESE
TESE
TRABALHOS
102
TRABALHOS DERIVADOS
DERIVADOSDA
DATESE
TESE
TRABALHOS
103
TRABALHOS DERIVADOS DA TESE
104
DERIVADOS DA
DA TESE
TESE
TRABALHOS DERIVADOS
105
TRABALHOS
TRABALHOS DERIVADOS
DERIVADOS DA TESE
106
DERIVADOS DA
DA TESE
TESE
TRABALHOS DERIVADOS
107
TRABALHOS DERIVADOS
DERIVADOS DA
DA TESE
TESE
TRABALHOS
108
TRABALHOS DERIVADOS DA TESE
6.3 ARTIGO ACEITO NO THE AMERICAN JOURNAL OF PATHOLOGY
MICROGLIA/MACROPHAGES
MIGRATE
THROUGH
RETINAL
EPITHELIUM BARRIER BY A TRANSCELLULAR ROUTE: INVOLVEMENT
IN DIABETIC RETINOPATHY
ROLE OF PKCΖ IN MICROGLIA/MACROPHAGES TRAFFICKING DURING
DIABETIC RETINOPATHY IN GOTO KAKIZAKI RATS.
1,2,3
Samy Omri
1,2,3,4
, Francine Behar-Cohen
1,2,3
Sennlaub
1,2,3
, Yvonne de Kozak
5
1,2,3
, Boubaker Omri
Florian
1,2,3
, Lourena Mafra Verissimo , Laurent Jonet
1,2,3,4
,
, Michèle Savoldelli
1,2,3
, Patricia Crisanti
Crisanti P and Omri B contributed equally to the work
1
INSERM, U872 Physiopathology of ocular diseases: Therapeutic innovations, Paris,
France
2
Centre de Recherche des Cordeliers, Pierre et Marie Curie University, UPMC UMRS
872, Paris, France
3
Paris Descartes University, UMRS 872, Paris, France
4
Department of Ophthalmology, Hôtel-Dieu de Paris, France
5
Paris Sud 11 University, UMR CNRS 8612, Physico-chemistry-PharmacotechnyBiopharmacy, Faculty of Pharmacy, Châtenay-Malabry, France
Number of text pages: 25
Number of table: 1 Number of figures: 7
Short running title: Transcellular RPE route for retinal microglia
Corresponding author
Correspondence to: Crisanti P.
Centre de recherche des Cordeliers
15 Rue de l’Ecole de Medecine, 75270 Paris Cedex 06, France.
Tel 33 1 40 46 78 67
Fax: 33 1 40 46 78 65;
e-mail: [email protected]
109
TRABALHOS DERIVADOS DA TESE
ABSTRACT
Diabetic retinopathy is associated with ocular inflammation leading to retinal barriers
breakdown, macular edema and visual cell loss. We investigated molecular mechanisms
involved in microglia/macrophages trafficking in retina and retinal pigment epithelium
(RPE) and the role of protein kinase Cζ (PKCζ) in this process. Goto Kakizaki (GK)
rats, a model for spontaneous type 2 diabetes were studied until 12 months of
hyperglycemia. During early stages of diabetes (up to 5 months), low number of
microglia/macrophages was detected in the subretinal space together with numerous
pores in RPE cells that allowed inflammatory cells trafficking between retina and
choroid. Expression of intercellular adhesion molecule-1 (ICAM-1), caveolin-1 (CAV1) and the atypical PKCζ involved in glucose transport to cell membrane, was identified
around RPE pores. In late stages of diabetic retinopathy (12 months of hyperglycemia),
the
number
of
pores
decreased
simultaneously
with
accumulation
of
microglia/macrophages in the subretinal space. Intravitreal injection of PKCζ inhibitor
in 12 months-old GK rats, reduced iNOS expression in microglia/macrophages, blocked
their migration through the retina preventing their subretinal accumulation. We show
here that a transcellular pathway through RPE contributes to microglia/macrophages
retinal trafficking, a physiological process in which PKCζ plays a key role. During
diabetic retinopathy, slowing of this process leads to subretinal accumulation of
activated microglia/macrophages that may participate to retinal pathogenic processes.
110
TRABALHOS DERIVADOS DA TESE
INTRODUCTION
1, 2
Diabetes is associated with immune imbalance and inflammation
. Diabetic
retinopathy is a severe complication of type 2 diabetes, leading to blindness due to
macular edema and loss of photoreceptors. Ruptures of ocular barriers and local
inflammation have been demonstrated as pathogenic events during the course of
2
diabetes . The inner blood retinal barrier is formed by tight-junctions between vascular
endothelial cells whilst the outer retinal barrier is specific to the eye and consists of the
tight-junction present in a monolayer epithelium, the retinal pigment epithelial cells
(RPE). The apical side of RPE faces the photoreceptor outer segments (the neuroretina)
and the basolateral side lies on the Bruch’s membrane, which separates the RPE from
the fenestrated endothelium of the choriocapillaris. The RPE is a selective exchange
platform between the systemic circulation and the retina. The subretinal space between
2
RPE and the neuroretina is an immune-privileged site and RPE and subretinal space
are the main sites of pathological manifestations during diabetes onset.
Microglial cells, the main resident sentinel immune cells are located around vessels in
3-8
the healthy retina
. These cells become activated, accumulate in the subretinal space
9-12
in diabetic retinopathy
13
, and may become neurotoxic
. Whilst activation of
microglia induced by hyperglycemia has been associated with the early development of
diabetic retinopathy, the chronic activation of microglia induced the release of cytokines
14
that cause neuronal cell death . In addition, chronic hyperglycemia also causes
oxidative stress that results in the activation of the atypical PKCζ which controls the
activity of the transcription factor NF-κB, and regulates the expression of inducible
nitric oxide synthase (iNOS), cyclo-oxygenase 2 (COX2), ICAM-1, thus controlling
15-17
vascular permeability and leukostasis
. We have previously shown that PKCζ is
expressed in ocular macrophages in a rat model of ocular inflammation. Further,
specific local inhibition of PKCζ reduced retinal vascular leakage, iNOS expression in
15
cells infiltrating the eye, and ocular cytokines production
. Over expression of iNOS
18-23
was also found in retinas of diabetic rodents and patients
.
111
TRABALHOS DERIVADOS DA TESE
Goto Kakizaki (GK) rat is a Wistar non-obese model of non-insulin dependent type 2
diabetes. These rats present hyperglycemia from 14 weeks after birth. Since microglial
9
activation has
been
reported in
human diabetic retinopathy
and since
15
microglia/macrophages play a critical role in inflammation and tissue damage
, we
investigated in the present study microglia/macrophages retinal trafficking and
activation during diabetes in GK rats. We show for the first time the presence of pores
in the RPE similar to those described in the vascular endothelium in inflammatory
24-26
situation
. We then studied the role of RPE pores in the accumulation of
microglia/macrophages cells in the subretinal space at late stages of diabetic retinopathy
in GK rats. We also analyzed the role of PKCζ (molecule involved in glucose transport
to cell membrane) in microglia/macrophages retinal accumulation by inhibiting PKCζ
activity in 12 months GK rats.
MATERIALS AND METHODS
Animals
The animals used in this work were treated in accordance with the Association for
Research in Vision and Ophthalmology (ARVO). Experimental procedures were
submitted and approved by the ethic committee of Paris Descartes University.
GK rats (Taconic Europe, Denmark), a Wistar non-obese model of Non-Insulin
Dependent type 2 Diabetes were used at different ages of hyperglycemia. They present
hyperglycemia from 14 weeks after birth to the time of sacrifice significantly different
from controls as shown in table 1. Plasma glucose > 250mg/ dl was considered as
diabetic state. Controls were selected from age-matched non-diabetic rats and with
plasma glucose < 150mg/ dl. Glycemia was measured using Accutrend GC and Accucheck compact equipments (Roche).
Immunohistochemistry on cryostat ocular sections and on flat mounts of retina or
RPE/ choroids
Immunohistochemistry was used to identify microglia/ macrophages and proteins
involved in transcellular pathways at 2, 5 and 12 months.
For sections, rat eyes were enucleated and post-fixed in 4% paraformaldehyde and
cryoprotected using sucrose. They were embedded in optimal cutting-temperature
112
TRABALHOS DERIVADOS DA TESE
(OCT) compound (Tissue-Tek; Miles Inc., Bayer Diagnostics, Puteaux, France), frozen
in liquid nitrogen and stored at−80 °C. Cryostat frozen sections (10 μm thick) (Leica
CM 3050S, Wetzlar, Germany) were performed and mounted on gelatin-coated slides
for immunohistochemical analysis. (n=7 per group).
For flatmounts, rat eyes were enucleated, fixed in 4% paraformaldehyde (PFA) for 15
min at room temperature and sectioned at the limbus; the anterior segments were
discarded. Retinas and choroids were fixed separately for additional 15min in acetone at
- 20°C. Specimens were incubated overnight at 4°C with primary antibodies diluted in
PBS supplemented with 10% fetal calf serum (FCS) and 0.1% Triton X-100. (n=9 per
group).
Antibodies
Primary antibodies used were: rabbit polyclonal anti-caveolin-1 (# 3238) (Cell
Signaling Saint Quentin Yvelines, France) (dilution 1:200), rabbit polyclonal antioccludin (71-1500) (Zymed, San Francisco, CA, USA) (dilution 1:200), mouse
monoclonal anti-PKCζ (ab57432) raised against to amino acid 165-255 specific of the
N-terminal region of the human PKCζ sequence (Abcam, Cambridge, UK) (dilution
1:400), mouse monoclonal anti-ICAM-1 (MCA773) (Serotec, Oxford, UK) (dilution
1:200), rabbit polyclonal anti-ionized calcium binding adaptor molecule 1, anti-IBA-1, a
specific marker for microglia/ macrophages (Wako, Richmond, USA) (dilution 1:400),
mouse monoclonal iNOS (sc-7271) (Santa Cruz Biotechnology, CA, USA) (dilution
1:75), mouse monoclonal anti glial fibrillary acidic protein-Cy3, (C9205) (Sigma
aldrich, St. Louis, MO USA) (dilution 1:200), Rhodamine Phalloidin (R415) (dilution 1
:400), anti zonula-occludens-1 (ZO-1) (sc-10804) (Santa Cruz Biotechnology, CA,
USA) (dilution 1: 100). The corresponding Alexa secondary antibodies (Invitrogen life
technology Carlsbad) were used to reveal the primary antibodies, and sections were
counterstained with 4', 6-diamino-2-phenylindol (DAPI) (Sigma aldrich St. Louis, MO
USA).
Sections and flatmounts were viewed with a fluorescence microscope (BX51; Olympus,
Rungis, France) and confocal microscope (LSM 510 laser scanning microscope Zeiss,
Carl Zeiss, Le Pecq, France). Three dimensional reconstruction and projection of Zstacks was performed with Zen 2009 LE software (Carl Zeiss). Images were then
exported to Photoshop software for preparation of final images. All immunostainings
were repeated at least 3 times, and staining that omitted the primary antibody served as
negative control.
113
TRABALHOS DERIVADOS DA TESE
Western Blotting analyses
Proteins were extracted from 5 neuroretinas and RPE/ choroids from GK rats at 2, 5 and
12 months of hyperglycemia and from non diabetic controls. Proteins were
homogenized in lysis buffer (10 mM Tris-HCl, pH 7.5, 1 mM EDTA, 1 mM EGTA,
150 mM NaCl, 0.5% Nonidet P40, 1% Triton X-100, β-mercaptoethanol) containing a
protease inhibitor cocktail (Roche, France). Protein concentration was determined using
a Bradford assay. Proteins (40–50 μg) were subjected to SDS-PAGE in a 12% sodium
dodecyl
sulfate-polyacrylamide
gel
electrophoresis,
and
electroblotted
onto
nitrocellulose membranes (Schleicher and Schuell BioScience, Dassel, Germany).
Membranes were incubated with: anti-PKCζ mouse monoclonal antibody (ab57432)
raised against amino acid 165-255 of the N-terminal region of the human PKCζ
sequence) (dilution 1:400), rabbit polyclonal anti-p-PKCζ (Thr 560) ab59412 obtained
from Abcam, Cambridge, UK) (dilution 1:200), rabbit polyclonal anti pPKCζ (Thr 410)
SC-12894-R (dilution 1:400) and rat anti-β-tubulin SC-5274 (dilution 1:400) obtained
from Santa Cruz Biotechnology CA, USA), rabbit polyclonal anti-caveolin-1 (# 3238)
Cell
Signaling,
Saint
Quentin
Yvelines,
France)
(dilution
1:400),
mouse
monoclonalanti-ICAM-1 (MCA773 Serotec, Oxford, UK,) (dilution 1:400).Then
membrane were incubated with corresponding secondary antibodies: peroxidase
conjugated F(ab)2 fragment (Caltag, Burlingame, Canada). Immunoreactive bands were
detected with the ECL Western Blotting Detection Reagents Kit (Amersham
Biosciences, Orsay, France). The relative abundance of individual proteins identified
was quantified by scanning densitometry. The relative band intensity of CAV-1, ICAM1, was calculated in comparison to b-tubulin after densitometry analysis.
For the
phosphorylated PKCζ Thr 410 and Thr 560 the relative band intensity was calculated in
comparison to nonphosphorylated PKCζ after densitometry analysis (Adobe photoshop
software).
Intravitreal injection of PKCζ specific inhibitor (PKCζi).
Rats were anesthetized with intramuscular injection of ketamine (88 mg/kg; Virbac,
France) and chlorpromazine (Largactil, 0.6 mg/kg; Sanofi-Aventis, Paris, France).
Pupils were dilated by instillation of 1 drop of 5% tropicamide (Ciba Vision, Toulouse,
France) and 1 drop of 1% tetracaine (Ciba Vision) was administered for local
anesthesia. Under a surgical microscope, an intravitreal injection of 4 µL of either
sterile pyrogen-free saline or PKCζi was performed using a sterile syringe and 30114
TRABALHOS DERIVADOS DA TESE
gaugeneedle (Microfine; Becton Dickinson, Meylan, France). The needle was left in the
eye for 10 seconds to allow aqueous humor to leave the eye via the trabecular
meshwork rather than by reflux along the needle track. The injection was performed
near the apex of the cornea, taking care not to damage the iris or the lens.
For inhibitory experiments, we injected PKCζi into the vitreous (4µL, 0.15µM in PBS)
(myr-SIYRRGARRWRKL (ref. 539624 obtained from Calbiochem, San Diego, CA,
USA) of 12 months-old diabetic GK rats and their controls (n=15 per group). Rats were
sacrificed 48 hours after PKCζi injection and eyes were used for immunohistochemistry
on sections (n=7/ n=5), on flatmounted tissues (n=9/ n=5) and for western blots (n=5/
n=5). To evidence the cellular targets of the peptide, we performed intravitreous
injections
(3µl,
0.15µM
in
PBS)
of
a
fluorescent
peptide
5-
Carboxytetramethylrhodamine (5-TAMRA) conjugated with the PKCζi (myr-K-(5TAMRA)-SIYRRGARRWRKL) (Proteogenix (France) in 12 months-old diabetic GK
rats and their controls (n=15 per group).
Intravitreal injection of rhodamine-liposome (Rh-Lip)
We have previously shown that after intravitreous injection, rhodamine-conjugated
27
liposomes were internalized in microglia
. To study the intraocular distribution of
microglia, we injected 3µl of cationic DOTAP/DOPE/ PE-Rhodamine liposomes into
the vitreous body of control and 5 months-old diabetic rats (n= 3). Cationic
DOTAP/DOPE/ PE-Rhodamine liposomes were prepared as follows. Briefly, the lipids
(1,2-dioleoyl-3-trimethylammoniumpropane
phosphoethanolamine
(DOPE)
and
(DOTAP),
1,2-dioleoyl-sn-glycero-3-
rhodamine-phosphatidylethanolamine
(PE-
Rhodamine) dissolved in chloroform were mixed to reach a final lipid mass ratio of 5.0:
4.7: 0.3 respectively. The chloroform was evaporated under vacuum and the resulting
lipid film was hydrated with milliQ water to a final concentration of 1 mg/ mL.
Liposomes containing 3% PE-Rhodamine had a size below 450 nm and exhibited
positive zeta potential values higher than +50 mV (≥ +70mV).
Quantification of activated microglia/macrophages in the neuroretina
Round IBA-1 stained cells were counted on neuroretina flatmounts from control or 12
months-old diabetic rats injected with saline or with PKCζi (n=3 rats per group and 4
areas per eye). The cell number was expressed as the mean number of round activated
115
TRABALHOS DERIVADOS DA TESE
IBA-1 positive cells/ mm².
Quantification of microglia/macrophages infiltrating the eye
Microglia/macrophages (IBA-1 stained cells) were counted on cryostat sections in retina
from control or 12 months-old diabetic rats injected with saline or with PKCζi (n=7 rats
per group and 12 sections per eye). For this quantification, 2 areas were chosen on each
section: the inner retina i.e. from the ganglion cell layer (GCL) to the outer plexiform
layer (OPL) and the outer retina i.e. from the outer nuclear cell layer (ONL) to the RPE,
as shown in figure 1A. The cell number was expressed as the mean number of IBA-1
positive cells/ retinal sections.
Quantification and criteria to identify transcellular pores
A transcellular pore was identified by three dimensional analyses as a circular
intracytoplasmic structure, delineated by PKCζ, ICAM-1, CAV-1 and actin
fluorescence in both the x-y and the z dimensions. With these criteria, quantification of
transcellular pores was performed on 9 eyes per experiment on whole flatmount of RPE
from 2, 5 and 12 months-old GK diabetic rats and their non diabetic controls. Number
of transcellular pores was expressed as the mean number of pores/ whole flatmount.
Semi-thin and ultra-thin sections
Eyes were fixed for 1 h in 2.5% glutaraldehyde in cacodylate buffer (0.1 M, pH 7.4).
Eyeballs were dissected, fixed for 3 h, postfixed in 1% osmium tetroxide in cacodylate
buffer, and dehydrated in graduated ethanol solutions. Samples were included in epoxy
resin and oriented. Semi-thin sections (1 μm, ultra microtome Reichert Ultracut E
[Leica]), were stained by toluidine blue. Ultra-thin sections (80 nm) were contrasted by
uranyl acetate and lead citrate and were observed with an electron microscope JEOL
100 CX II (JEOL) with 80 kV.
Statistics
Values are expressed as mean ± SEM. Student t test was used when comparing two
groups or using the non parametric Mann–Whitney U-test when comparing three or
more groups (Prism software version 4.0c; GraphPad Software, San Diego, CA).
Statistical significance was accepted as P value <0.05
116
TRABALHOS DERIVADOS DA TESE
RESULTS
Subretinal accumulation of microglia/macrophages and alteration of RPE in
diabetic rats after 12 months of hyperglycemia
In order to compare the distribution of microglia/macrophages in retina from diabetic
rats versus controls, IBA-1, a specific marker for microglia and macrophages, was used.
In control rats, few microglia/macrophages are located in the inner retinal layers (INL)
and in the choroid but no IBA-1 positive cells are detected in the outer retina or in the
subretinal space (Fig.1A).
By contrast, after 12 months of hyperglycemia in GK rats, numerous IBA-1 positive
cells accumulate in the retina and the subretinal space (Fig.1B and inset for higher
magnification). Indeed, the number of IBA-1 positive cells significantly increased after
12 months of diabetes, in the inner and outer layers of the retina (Fig.1C). The study in
semi-thin ocular sections of GK rats confirmed the presence of cells between
disorganized outer segments of photoreceptors (OS) and the RPE (Fig.1F, arrow). In
addition, diabetes was associated with important alterations of the RPE outer retinal
barrier.
To visualize RPE tight junctions, RPE flatmounts were stained with Zonula-occludens-1
(ZO1). It shows that in non-diabetic rats, ZO-1 labelled the regular hexagonal
membrane of RPE cells (Fig.1E) whereas in diabetic rats, RPE cytoplasmic membrane
showed a complete disorganization of ZO-1 labelling (Fig.1G).
Trans-epithelial pores are evidenced in RPE cells of diabetic
After 5 months of diabetes using phalloidin staining of RPE/ choroids flatmounts, we
observed significant F-actin remodeling, with a central actin ring forming a ―pore‖ in
some RPE cells, with apparent maintenance of cell membrane integrity (Fig.2A). Semithin sections of these flatmounts showed a focal cytoplasmic invagination towards the
choroid at the level of the pore (Fig.2B1). In electron microscopy sections, the RPE
nucleus appeared unchanged and a pore was observed in the center of the cell; in the
vicinity of the invaginated RPE, capillaries in the choroid had vertical orientation
(Fig.2B2).
Co-localization of CAV-1 and ICAM-1 is detected around the pore in RPE (Fig.2C-E)
supporting the hypothesis that a transcellular pathway occurs in the RPE of diabetic
117
TRABALHOS DERIVADOS DA TESE
rats. In RPE from control non-diabetic rats, PKCζ was located in the cytoplasm and
partly colocalized with occludin at the tight-junctions (Fig.3A, E). By contrast, in 5
months diabetic rats, whilst cell-cell junctions were not yet altered at this time point,
PKCζ clearly delineated the pore in RPE cells (Fig.3B-D, F-G). Confocal microscopy
observation showed that the apical (Fig.3C) and basal (Fig.3D) side of the pore were
stained by anti-PKCζ and the tight-junctions stained with anti-occludin antibodies,
demonstrating that the pores crossed the whole cell thickness without altering tightjunctions.
Confocal microscopy combined with 3D imaging of RPE flatmounts from non diabetic
(Fig.3E, E’) or diabetic rats (Fig.3F, F’, G, G’) allowed scanning of the whole RPE
thickness from the apical side towards the baso-lateral side. In non diabetic rats (Fig.3E,
E’) PKCζ was localized in the cytoplasm and at the membrane, partially co-localized
with occludin. In diabetic rats, (Fig.3F, F’, G, G’), PKCζ stained the pore from the basal
up to the apical side of RPE cells. Furthermore, double staining for CAV-1 and PKCζ
(Fig.3H-J) showed a similar distribution, suggesting that in RPE cells PKCζ, F-actin,
ICAM-1 and CAV-1 contribute to the pore formation.
The pores: a transcellular route for microglia/macrophages through the RPE
RPE flatmount from 5 months old GK rat were studied by confocal scanning
microscopy with triple staining for IBA-1/ PKCζ/ DAPI, to visualize both
microglia/macrophages and the pores. Orthogonal images of the RPE monolayer were
reconstructed from a stack of confocal sections taken from the apical towards the basal
membrane of the RPE layer (Fig.4A). The first Z-sections of the confocal stack analysis
highlighted the beginning of the cell process as a green point. We identified IBA-1
positive cells with intact nuclei, inside the whole length of the transcellular pore.
Microglia/macrophages transmigration through RPE was also confirmed using 3D
images (Fig.4B). In parallel, frozen sections prepared from diabetic retina were stained
for IBA-1. On transversal sections, we were able to observe IBA-1 positive cells just
below the RPE layer (Fig.4C-D) with some cytoplasmic extensions between RPE cells,
suggesting that microglia/macrophages may pass through the RPE barrier.
To determine whether microglia/macrophages could exit from retina through RPE
barrier, intravitreal rhodamine-liposomes (Rh-Lip) injection was performed in control
and
diabetic
rats
at
5
months.
Rh-Lip
were
internalized
in
activated
microglia/macrophages identified by IBA-1 staining. Indeed, double stained Rh-Lip/
118
TRABALHOS DERIVADOS DA TESE
IBA-1 cells were mainly detected in the inner retina and in the subretinal space (Fig.4F)
but IBA-1 positive cells containing Rh-Lip could also be observed in the choroid at the
basolateral side of RPE indicating that cells might have migrated from the subretinal
space towards the choroid (Fig.4G).
Pores density in RPE from diabetic and non-diabetic rats
RPE pores were quantified in diabetic and non-diabetic rats at 2, 5 and 12 months
(Fig.5A). Whilst in control non-diabetic animals, the number of pores/ mm2
significantly increased from 5 to 12 months, in diabetic rats it significantly increased
from 2 to 5 months to significantly decrease at 12 months. The reduced number of RPE
pores at 12 months in diabetic rats correlated well with the increasing number of
subretinal microglia/macrophages at this time point (Fig.1B). The decrease of pores was
associated with significant lower expression of CAV-1 and ICAM-1 at 12 months
(Fig.5B-C). Interestingly, expression of PKCζ did not significantly change in diabetic
eyes (not shown), but its phosphorylated (p Thr 410) active form increased during early
stages of diabetes (2 and 5 months) and then significantly decreased at 12 months
(Fig.5D). At this time point we observed a lower number of transcellular pores in RPE
suggesting a role for PKCζ in pore formation process.
Interestingly, in 12 months old non-diabetic rats (Fig.5A), pores were observed within
RPE cells with high amounts of CAV-1 and activated PKCζ similar to young diabetic
rats (5 months). These data suggest a physiological role for a transcellular route through
RPE cells taking place in aging non diabetic rats and in an accelerated manner in
diabetic retina, reinforcing the idea that type 2 diabetes can be viewed as a form of
premature aging.
Intravitreal injection of the PKCζinhibitor in 12 months old diabetic rats
deactivated microglia/ macrophages, blocked their migration and impaired pore
formation
To ascertain that PKCζ activity participated to microglia cells trafficking and pores
formation, control and diabetic 12 months old rats were given one intravitreal injection
of PKCζ inhibitor (PKCζi) 48 hours before sacrifice. We first evaluated the distribution
of PKCζi conjugated with the fluorochrome (TAMRA) at 48 hours after its intravitreous
injection in control and diabetic rats. The peptide was mainly located in
microglia/macrophages (as shown by IBA-1 co-labeling) as well as in RPE cells
119
TRABALHOS DERIVADOS DA TESE
(Fig.6C, D). It is interesting to note that when PKCζi was injected into the vitreous (Fig.
6C, D) microglia/macrophages were not observed in the subretinal space of diabetic
rats, suggesting a role of PKCζ in microglia/macrophages migration. Moreover, we
show that PKCζ activity was reduced in the retina of diabetic rats as evaluated by its
autophosphorylation on Thr 560 which decreased 2.5-fold in non diabetic rats injected
into the vitreous with PKCζ i and 4.4fold in diabetic rats (Fig.6E).
The quantification of microglia/macrophages was performed in the inner retina (GCL,
INL) and outer retina (ONL, RPE) of non-diabetic and diabetic rats. Results indicated
that intravitreal injection of PKCζi decreased significantly (10-fold) the number of
microglia/ macrophages in the subretinal space and the outer retina of diabetic rats
compared to non treated diabetic rats (Fig.6F). Furthermore, inhibition of PKCζ
activation significantly reduced pore formation in RPE from treated diabetic and control
rats compared to RPE from untreated diabetic and control rats (respectively 5 and 3.5fold) (Fig.6G).
To evaluate microglia activation state, flatmounts of the neuroretina were double stained
by GFAP/ IBA-1 (Fig.7A-H), iNOS/ IBA-1 (Fig.7I-J). In 12 months old-diabetic rats,
IBA-1 labelling of flat-mounted neuroretina showed round amoeboid shape activated
microglial cells located around blood vessels surrounded by GFAP stained astrocytes
(Fig.7B, D). PKCζ inhibition induced a change in microglia morphology showing a
resting dendritic shape with long branching processes and a small cellular body (Fig.7,
G, H) similar to that observed in 12 months old non diabetic rats (Fig. 7C).
Quantification of activated microglia was performed by counting round activated IBA-1
cells in neuroretina flatmounts (Fig 7I). The number of activated IBA-1 cells was
significantly increased in diabetic retinas compared to non diabetic controls. The
intravitreal injection of PKCζi decreased the number of activated IBA-1 cells in diabetic
rats and controls. In addition, PKCζ inhibition suppressed iNOS expression as shown in
a macrophage/microglial cell present in the retina of a PKCζi treated GK rat (Fig.7J, K)
further demonstrating that PKCζ inhibition deactivated microglia/macrophages.
DISCUSSION
Low grade inflammation has been evidenced in the retina of diabetic animals and
9, 14, 17-19, 28
diabetic patients
. Particularly, microglial cells activation was found to be an
120
TRABALHOS DERIVADOS DA TESE
early marker of diabetic changes in different animal models and to potentially release
neurotoxic agents at advanced stages of diabetes. Indeed activated microglia produce
cytotoxic substances, such as tumor necrosis factor α (TNF-α), reactive oxygen species,
14, 29, 30
proteases, and excitatory amino acids, which may induce neuronal degeneration
.
Moreover, the role of microglia has been confirmed in human retina at different stages
of diabetes with accumulation of activated cells in the outer retina and subretinal space
9
in case of advanced macular edema .
The central question of our study was how, in vivo, in the time course of diabetes,
macrophages/microglial cells trafficking is modified leading to subretinal accumulation
and potential toxicity. Unexpectedly, we observed that ―pores‖ in RPE cells are formed
in normal old non diabetic rat retinas and that at the early stages of diabetic retinopathy,
when tight junctions between RPE cells are intact, these pores serve as a migratory
pathway for inflammatory cells (microglia/macrophages). At more advanced stages of
diabetes (12 months), the number of pores decreases in RPE paralleling the
accumulation of subretinal activated microglia/macrophages.
In the vascular endothelium, it has become increasingly clear that in addition to the
―paracellular‖ route, a ―transcellular‖ route is used by leukocytes or lymphocytes for
24-26
migration through the endothelial cell body
. However, no such phenomenon has
been previously described in epithelia. In our study, we report strong data favouring the
hypothesis that a transcellular pathway takes place in RPE cells: -the identification of
―tunnel structures‖ crossing the whole cell thickness with preserved tight-junctions, -the
recruitment of ICAM-1 and CAV-1 around the pores and the involvement of PKCζ in
the pore formation, -the identification of IBA-1 positive cells (microglial resident cells)
crossing the RPE through the pore.
Presence of microglia/macrophages in the retina of diabetic GK rat could be related to
the expression of ICAM-1, which is essential for inflammatory cells migration. In this
context, glucose was shown to enhance ICAM-1 expression in a dose-dependent
manner. Further, in RPE cells of rats presenting a diabetes induced by STZ, an up31
regulation of ICAM-1 was reported
. In addition, transcellular migration of
32, 33
inflammatory cells requires CAV-1 protein
. As previously shown in vascular
endothelial cells, we show in the present study that colocalization of CAV-1 and ICAM1 is present at the pore border of RPE supporting the hypothesis that a transcellular
121
TRABALHOS DERIVADOS DA TESE
pathway occurs through RPE pores of diabetic rats.
What is the link between diabetes and RPE transmigration of microglia/macrophages?
We have demonstrated that at the early stages of diabetes, a RPE transcellular pathway
is functional. At later stages of diabetes (12 months), decreased ICAM-1 and CAV-1
protein expression in RPE cells and accumulation of subretinal microglia/macrophages
are observed together with significant decrease of RPE pores. This suggests that a
reduction
of
this
RPE
functional
pathway could
contribute
to
subretinal
microglia/macrophages accumulation. To ascertain that a migration of cells from the
retina towards the choroid could occur through RPE, we injected into the vitreous
cationic liposomes containing rhodamine. In normal rats, such liposomes injected into
the vitreous do not cross the outer retinal barrier and are engulfed by resident or
27
activated macrophages and by RPE cells . In 5 months-old diabetic rats, intense uptake
of Rh-Lip is observed in activated microglia. A more striking finding was that we could
identify IBA-1 positive cells containing Rh-Lip migrating into the choroid at a time
when the RPE tight junctions are preserved further suggesting that a RPE transcellular
pathway is operating.
We also showed herein that PKCζ is a new molecule participating in this process. Our
results are supported by a recent review reporting that inhibition of PKCζ activity
prevented the TNF-α-induced ICAM-1 clustering and the early onset of endothelial
26
adhesivity
. Activation of the PKCζ/ NF-κB signaling pathway induced the
25
transcription of cytokines and the adhesion molecules ICAM-1 and CAV-1
required
for inflammatory cells transcellular migration. Indeed, blocking PKCζ activity in LPSinduced ocular inflammation led to a decrease of inflammation via the inhibition of
15
PKCζ/ NF-κB signaling pathway
34, 35
. Besides its role in the junction regulation
,
PKCζ could also participate in the pore formation since CAV-1 interacts with PKCζ via
its scaffolding domain. This may explain the propensity to accumulate PKCζ in
caveolae, where it may be directly activated by ceramides contained within such
36
domains
. Taken together, our results show that a transcellular pathway involving
proteins similar to those described in vascular endothelial cells can occur in the outer
retinal barrier constituted by RPE cells.
We also show in the present study that PKCζ is activated during the early stages of the
diabetic retinopathy (2 and 5 months) when the number of pores is increasing, and its
122
TRABALHOS DERIVADOS DA TESE
activation is significantly reduced at later stage when pores number also decreases.
To further determine the role of PKCζ activation in the pores formation, an intravitreous
injection of a specific fluoresceine labeled PKCζ inhibitor (PKCζi) was performed. It
showed that PKCζi was efficiently phagocytosed by IBA-1 positive cells and RPE cells.
Furthermore, PKCζ inhibition reduced microglia/macrophages migration and activation,
as confirmed by lower iNOS production and deactivated cell morphology. Under these
conditions of PKCζ inhibition, the subretinal microglia/macrophages accumulation was
impaired and the number of RPE cell pores was reduced, demonstrating that PKCζ is
involved in microglia/macrophages trafficking during DR.
Very recently, it was shown that PKCζ plays a crucial role in retinal vascular
permeability induced by TNF-α suggesting its possible implication in diabetes-induced
37
blood retinal barrier breakdown .
In conclusion, migration of microglia/macrophages through the RPE seems to be a
physiological process facilitating cell trafficking between retina and choroid. During
early stages of diabetes, we show that the number of RPE pores increased. In later
stages of diabetes, the number of RPE pores decreased resulting in subretinal
accumulation of activated microglia/macrophages and subsequent retinal damages.
Therefore, the alteration of the transcellular migration pathway could further worsen
diabetic induced photoreceptor death. Intravitreal injection of PKCζi prevented
microglia/macrophages
subretinal
accumulation
and
activation.
Targeting
microglia/macrophages activation and trafficking using PKCζ inhibitors may be of great
interest for preventing diabetic retinopathy.
123
TRABALHOS DERIVADOS DA TESE
ACKNOWLEDGMENTS
This work was supported by the National Institutes of Health and Medical Research:
INSERM, by the Fedération des Aveugles et Handicapés Visuels de France: (FAF), by
the Association CRO; Research Center in Ophtalmology", and by the Association
Retina France (AFRP). We are grateful to Christophe Klein (UMRS 872 Centre de
Recherche des Cordeliers) for technical assistance. We are grateful to Amélie Bochot
and Elias Fattal (Paris Sud 11 University, UMR CNRS 8612, Physico-chemistryPharmacotechny-Biopharmacy, Faculty of Pharmacy, Châtenay-Malabry, France) for
Rhodamine-Liposomes gift.
124
TRABALHOS DERIVADOS DA TESE
REFERENCES
1. Wellen KE, Hotamisligil GS: Inflammation, stress, and diabetes, J Clin Invest 2005,
115:1111-1119
2. Xu H, Chen M, Forrester JV: Para-inflammation in the aging retina, Prog Retin Eye
Res 2009, 28:348-368
3. Hickey WF, Kimura H: Perivascular microglial cells of the CNS are bone marrow
derived and present antigen in vivo, Science 1988, 239:290-292
4. Perry VH, Gordon S: Macrophages and microglia in the nervous system, Trends
Neurosci 1988, 11:273-277
5. Streit WJ, Graeber MB, Kreutzberg GW: Functional plasticity of microglia: a review,
Glia 1988, 1:301-307
6. Lassmann H, Schmied M, Vass K, Hickey WF: Bone marrow derived elements and
resident microglia in brain inflammation, Glia 1993, 7:19-24
7. Ling EA, Wong WC: The origin and nature of ramified and amoeboid microglia: a
historical review and current concepts, Glia 1993, 7:9-18
8. Ling EA: Monocytic origin of ramified microglia in the corpus callosum in postnatal
rat, Neuropathol Appl Neurobiol 1994, 20:182-183
9. Zeng HY, Green WR, Tso MO: Microglial activation in human diabetic retinopathy,
Arch Ophthalmol 2008, 126:227-232
10. Combadiere C, Feumi C, Raoul W, Keller N, Rodero M, Pezard A, Lavalette S,
Houssier M, Jonet L, Picard E, Debre P, Sirinyan M, Deterre P, Ferroukhi T, Cohen SY,
Chauvaud D, Jeanny JC, Chemtob S, Behar-Cohen F, Sennlaub F: CX3CR1-dependent
subretinal microglia cell accumulation is associated with cardinal features of age-related
macular degeneration, J Clin Invest 2007, 117:2920-2928
11. Xu H, Chen M, Manivannan A, Lois N, Forrester JV: Age-dependent accumulation
oflipofuscin in perivascular and subretinal microglia in experimental mice, Aging Cell
2008,7:58-68
12. Xu H, Chen M, Mayer EJ, Forrester JV, Dick AD: Turnover of resident retinal
microglia in the normal adult mouse, Glia 2007, 55:1189-1198
13. Ma W, Zhao L, Fontainhas AM, Fariss RN, Wong WT: Microglia in the mouse
retina alter the structure and function of retinal pigmented epithelial cells: a potential
cellular interaction relevant to AMD, PLoS One 2009, 4:e7945
125
TRABALHOS DERIVADOS DA TESE
14. Krady JK, Basu A, Allen CM, Xu Y, LaNoue KF, Gardner TW, Levison SW:
Minocycline reduces proinflammatory cytokine expression, microglial activation, and
caspase-3 activation in a rodent model of diabetic retinopathy, Diabetes 2005, 54:15591565
15. de Kozak Y, Omri B, Smith JR, Naud MC, Thillaye-Goldenberg B, Crisanti P:
Proteinkinase Czeta (PKCzeta) regulates ocular inflammation and apoptosis in
endotoxin-induced uveitis (EIU): signaling molecules involved in EIU resolution by
PKCzeta inhibitor andinterleukin-13, Am J Pathol 2007, 170:1241-1257
16. Banan A, Zhang L, Fields JZ, Farhadi A, Talmage DA, Keshavarzian A: PKC-zeta
prevents oxidant-induced iNOS up regulation and protects the microtubules and gut
barrier integrity, Am J Physiol Gastrointest Liver Physiol 2002, 283:G909-922
17. Kern TS: Contributions of inflammatory processes to the development of the early
stages of diabetic retinopathy, Exp Diabetes Res 2007, 2007:95103
18. Du Y, Sarthy VP, Kern TS: Interaction between NO and COX pathways in retinal
cells exposed to elevated glucose and retina of diabetic rats, Am J Physiol Regul Integr
CompPhysiol 2004, 287:R735-741
19. Abu El-Asrar AM, Desmet S, Meersschaert A, Dralands L, Missotten L, Geboes K:
Expression of the inducible isoform of nitric oxide synthase in the retinas of human
subjects with diabetes mellitus, Am J Ophthalmol 2001, 132:551-556
20. Du Y, Smith MA, Miller CM, Kern TS: Diabetes-induced nitrative stress in the
retina, and correction by aminoguanidine, J Neurochem 2002, 80:771-779
21. Kowluru RA, Engerman RL, Kern TS: Abnormalities of retinal metabolism in
diabetes or experimental galactosemia VIII. Prevention by aminoguanidine, Curr Eye
Res2000, 21:814-819
22. Kowluru RA: Retinal metabolic abnormalities in diabetic mouse: comparison with
diabetic rat, Curr Eye Res 2002, 24:123-128
23. Kowluru RA: Effect of reinstitution of good glycemic control on retinal oxidative
stress and nitrative stress in diabetic rats, Diabetes 2003, 52:818-823
24. Dejana E: The transcellular railway: insights into leukocyte diapedesis, Nat Cell
Biol2006, 8:105-107
25.
Millan
J,
Hewlett
L,
Glyn
M,
Toomre
D,
Clark
P,
Ridley
AJ:
Lymphocytetranscellular migration occurs through recruitment of endothelial ICAM-1
to caveola- and Factin-rich domains, Nat Cell Biol 2006, 8:113-123
126
TRABALHOS DERIVADOS DA TESE
26. Rahman A, Fazal F: Hug tightly and say goodbye: role of endothelial ICAM-1 in
leukocyte transmigration, Antioxid Redox Signal 2009, 11:823-839
27. Camelo S, Lajavardi L, Bochot A, Goldenberg B, Naud MC, Fattal E, Behar-Cohen
F,de Kozak Y: Ocular and systemic bio-distribution of rhodamine-conjugated liposomes
loaded with VIP injected into the vitreous of Lewis rats, Mol Vis 2007, 13:2263-2274
28. Wang AL, Yu AC, He QH, Zhu X, Tso MO: AGEs mediated expression and
secretion of TNF alpha in rat retinal microglia, Exp Eye Res 2007, 84:905-913
29. Zeng XX, Ng YK, Ling EA: Neuronal and microglial response in the retina of
streptozotocin-induced diabetic rats, Vis Neurosci 2000, 17:463-471
30. Rungger-Brandle E, Dosso AA, Leuenberger PM: Glial reactivity, an early feature
of diabetic retinopathy, Invest Ophthalmol Vis Sci 2000, 41:1971-1980
31. Hirano Y, Sakurai E, Matsubara A, Ogura Y: Suppression of ICAM-1 in retinal and
choroidal endothelial cells by plasmid small-interfering RNAs in vivo, Invest
Ophthalmol VisSci 51:508-515
32. Marmon S, Hinchey J, Oh P, Cammer M, de Almeida CJ, Gunther L, Raine CS,
Lisanti MP: Caveolin-1 expression determines the route of neutrophil extravasation
throughskin microvasculature, Am J Pathol 2009, 174:684-692
33. Marmon S, Hinchey J, Raine CS, Lisanti MP: Chemokine transport and leukocyte
extravasation through dermal microvasculature in the absence of caveolae, J Dermatol
Sci2009, 53:225-228
34. Gopalakrishnan S, Hallett MA, Atkinson SJ, Marrs JA: aPKC-PAR complex
dysfunction and tight junction disassembly in renal epithelial cells during ATP
depletion, AmJ Physiol Cell Physiol 2007, 292:C1094-1102
35. Etienne-Manneville S, Hall A: Cell polarity: Par6, aPKC and cytoskeletal crosstalk,
Curr Opin Cell Biol 2003, 15:67-72
36. Fox TE, Houck KL, O'Neill SM, Nagarajan M, Stover TC, Pomianowski PT, Unal
O,Yun JK, Naides SJ, Kester M: Ceramide recruits and activates protein kinase C zeta
(PKCzeta) within structured membrane microdomains, J Biol Chem 2007, 282:1245012457
37. Aveleira CA, Lin CM, Abcouwer SF, Ambrosio AF, Antonetti DA: TNF-(65)
signals through PKC{zeta}/NF-{kappa}B to alter the tight junction complex and
increase retinal endothelial cell permeability, Diabetes 2010
127
TRABALHOS DERIVADOS DA TESE
FIGURE LEGENDS
TABLE 1. Weight and blood glucose concentration in normoglycemic controls and
hyperglycemic diabetic GK rats.
Values are expressed as the mean +/- SEM. *P< 0,05 control vs. diabetic
FIGURE 1. Microglia/macrophages accumulation in the subretinal space of 12 month
sold diabetic GK rats
A-B: Sections from 12 months old GK rat retina immunostained with IBA-1 antibody
(green)and DAPI (blue) associated with phase contrast. In 12 months-old non-diabetic
rats, rare IBA-1 positive cells are located in the inner retina (A). In 12 months-old
diabetic GK rats, number of IBA-1 positive cells increases in the inner retina and
accumulate in the subretinal space (arrowhead and inset) (B).
C: Cellular counts of IBA-1 positive cells on cryostat sections of the retina showed a
significant increase of their number in the inner retina (1.9-fold) and subretinal space
(7.6-fold) in 12 months-old diabetic rats vs. non diabetic rats. (n= 7 eyes per group); *,
P< 0, 05.
D, F: Vacuolization of RPE cells is observed (asterisk), and presence of a large
subretinal cell(arrowhead, F) is detected between disorganized outer segments of
photoreceptors (OS) in 12months old diabetic GK rats compared to non diabetic
controls (D), toluidine blue–stainedsemi-thin sections.
E, G: RPE flatmounts stained by ZO-1 (red) and DAPI show RPE cells morphology
changes and syncytium formation (*) in 12 months old diabetic rats (G) as compared to
control (E).
Scale bar: 25 μm (A-G). (GCL) ganglion cell layer, (IPL) inner plexiform layer, (INL)
inner nuclear layer, (OPL) outer plexiform layer, (ONL) outer nuclear layer, (RPE)
retinal pigmented epithelium, (OS) outer segment of photoreceptors.
FIGURE 2. ICAM-1, CAV-1 expression, actin recruitment and cell invagination
strongly suggest the presence of a transcellular pore in diabetic RPE
A: RPE flatmount from 5 months old diabetic GK rat stained by phalloidin (red) and
DAPI(blue) shows the formation of a central intracytoplasmic actin ring (arrow) in
some RPE cells.
128
TRABALHOS DERIVADOS DA TESE
B1-B2: Semi and ultra-thin sections of the pore visualized by actin in A, show
invagination of the RPE cells from the apical toward the basal part (arrow), highlighting
the direction of the pore formation in the RPE (B1). On ultrathin section, the cell
nucleus is preserved, displaced laterally by a pore formation in the cell (B2).
C-E: Triple staining by CAV-1 (green), ICAM-1 (red) and DAPI (blue) shows
colocalization of CAV-1 and ICAM-1 surrounding the pore with preserved nucleus on
the edge of the cell (arrow) (E). Scale bar: 25 μm (A-B1-C-D-E), 5μm (B2).
FIGURE 3. Involvement of PKCζin the pore formation
A-G: Double staining of RPE flat mounts from 5 months-old GK rats by PKCζ (red)
and occludin (green). In non diabetic rats, cytoplasmic and membrane PKCζ
localization (A).Under diabetic conditions, PKCζ labeling delineates the pore in the
center of RPE cell(arrow). RPE cell junctions are not altered (B).
C-D: Higher magnification of confocal images from apical and basal side of the cell,
with the pore double stained by anti-PKCζ (red) and anti-occludin (green).
E’-F’-G’: 3D imaging corresponding to the top view projection of all z-series sections
of RPEcell imaged on E, F, G confirmed the distribution of PKCζ around the pore
crossing the cellfrom the apical to the basal side.
H-I-J: Triple staining by CAV-1 (green), PKCζ (red) and DAPI (blue) shows the
colocalization of CAV-1 and PKCζ around the pore. Scale bar: 25 μm.
FIGURE 4. Transcellular migration of microglia/macrophages through RPE pores
A: RPE flatmount from 5 months old GK rat immunostained with PKCζ (red), IBA-1
(green),DAPI (blue) and imaged by confocal microscopy. Top view projection of all zseries sections of a representative IBA-1 positive cell (green) in a transcellular pore
delimited by PKCζ expression (red). The first Z –sections of the confocal stack analysis
highlighted the beginning of the cell process as a green point (arrow). The end Zsections clearly show a microglia/macrophage within the pore.
B: 3D imaging corresponding to projection of all z-series sections of RPE cell and IBA1positive cell imaged in A, confirmed the presence of IBA-1 positive cell inside the
pore.
C-D: Sections from 5 months old GK rat retina immunostained with IBA-1 antibody
(green) and DAPI (blue) associated with phase contrast. IBA-1 staining shows a
129
TRABALHOS DERIVADOS DA TESE
macrophage/microglia passing through the RPE (arrow) (C) and showing a cytoplasmic
extension between 2 RPE cells (arrowhead) (D).
E-G: Retinal sections 72 hrs after intravitreous injection of rhodamine-liposome (RhLip)(red), macrophages/microglia stained with IBA-1 (green). E: In 5 old months non
diabeticrats, liposomes are engulfed by IBA-1 positive cells in the inner retina (black
arrow). F: Atthe same age in diabetic GK rats, numerous IBA-1 positive cells having
engulfed Rh-Lip are located in the outer retina and subretinal space (black arrows) and
under the RPE, in the choroid (white arrow). Higher magnification confirmed that IBA1 positive cells loaded with Rh-Lip have migrated from the vitreous through the retina
and RPE towards the choroid.
Scale bar: 25 μm. (RPE) retinal pigmented epithelium, (OS) outer segment of
photoreceptor.
FIGURE 5. Quantification of the number of pores in RPE cells and CAV-1, ICAM1,PKCζexpression in the time course of diabetes
A: Quantification of pores as a function of aging in non-diabetic and diabetic GK rats.
In diabetic rats, the density of pores increases with a maximum at 5 months (2.8-fold)
and then decreases at 12 months (3-fold). In non-diabetic rats, pore density increases
significantly only at 12 months (4.4-fold from 5 to 12 months) to reach a higher density
compared to olddiabetic rats (7-fold). (n=9 eyes per group). *, P< 0, 05 vs. non diabetic;
#, P<0, 05 vs. five months. Number of transcellular pores was expressed as the mean
number of pores/whole flatmount.
B-D: Immunoblotting of RPE/ choroid: expression of β-tubulin, CAV-1 (B), ICAM-1
(C)and, phosphorylated PKCζ Thr 410 (D) in 2, 5 and 12 months non-diabetic and
diabetic rats. In diabetic rats, ICAM-1 and CAV-1 increase significantly during the
early phase of diabetes(2 and 5 months) and then decrease at 12 months. PKCζ activity
evaluated by Thr 410immunodetection (D) showed the same timing of expression as
CAV-1 and ICAM-1. In non diabeticrats, ICAM-1 significantly increases at 12 months
(C).
* P<0, 05 vs. non diabetic; #, P<0, 05 vs. five months. (Closed bar: diabetic; open bar:
nondiabetic).
130
TRABALHOS DERIVADOS DA TESE
FIGURE 6. Effects of PKCζinhibition on microglia/macrophages retinal infiltration and
on the pore density
Retinal sections from non-diabetic (Control) (A, C) or 5 months-old diabetic GK rats
(Diabetic) (B, D) were immunostained with anti-IBA-1 (green). PKCζ myristoylated
inhibitory peptide conjugated with fluorochrome TAMRA (TAMRA- PKCζ inhibitor)
(red)was injected into the vitreous 48 hours before sacrifice. TAMRA- PKCζ inhibitor
(red) is phagocytosed by IBA-1 positive cells and by RPE cells (C, D) and it blocks the
mobilization of IBA-1 positive cells in the internal layers of the retina impeding them to
reach the external layers of the retina in diabetic conditions (D) compared to non
diabetic controls (B).
(GCL) ganglion cell layer; (INL) inner nuclear layer; (ONL) outer nuclear layer; (RPE)
retinal pigmented epithelium. Scale bar: 25μM.
E: Proteins from non diabetic (control) and diabetic GK rat retinas treated or not with
PKCζi were analysed by immunoblotting and quantified for PKCζ autophosphorylation
site: phosphorylated PKCζ Thr 560. (n=5 eyes per group); *, P< 0,05 vs. without PKCζ
inhibitor(PKCζi) injection.
F: Quantification of IBA-1 positive cells density in the inner retina and in the subretinal
spaceon retinal sections, confirmed that PKCζ inhibition significantly increased the
IBA-1 positive cell density in the inner retina of diabetic rats compared to non diabetic
controls, whereas educed their number in the outer retina. (n=7 eyes per group); *, P<
0,05 vs. without PKCζi injection. The cell number was expressed as the mean number
of IBA-1 positive cells /retinal sections.
G: Pore density was evaluated by counting the number of pores in RPE flatmounts from
12months-old GK diabetic and non-diabetic rats. The pore density was reduced in old
diabetic rats as compared to controls and PKCζ inhibition significantly decreased the
pore density inboth cases. (n=9 eyes per group); *, P< 0,05 vs. without injection.
(Closed bar: diabetic; openbar: non diabetic).
FIGURE 7. Effects of PKCζon microglia/macrophages activation
A-H: IBA-1 (green) and GFAP (red) immunostaining on whole neuroretina flamounts
from12 months-old non diabetic (A, E) or diabetic GK rats (B, F).
Non diabetic controls treated with the PKCζ inhibitor (E) or not treated (A) showed in
the retina, microglia with an activated form (G, C respectively). By contrast, in diabetic
131
TRABALHOS DERIVADOS DA TESE
GK rats not treated with PKCζ inhibitor (B), microglia showed a round, amoeboid
shape (D), whereas PKCζ inhibition (F) induced a change in IBA-1 positive cells
morphology, indicating a return to a normal resting microglia (H).
Quantification of round activated IBA-1 microglia/macrophages (green) in neuroretina
flatmounts. Graph shows the mean number of cells/ mm2 counted in 4 areas in 3
separate flatmounts (I). Double staining of IBA-1 positive cells (green) with iNOS (red)
showed that in diabetic GK rats treated with PKCζ inhibitor (K) IBA-1 positive cells do
not express iNOS as compared to activated IBA-1 positive cells in the diabetic GK rats
non treated (J). Scale bar:25 μm.
132
TRABALHOS DERIVADOS DA TESE
133
TRABALHOS DERIVADOS DA TESE
134
TRABALHOS DERIVADOS DA TESE
135
TRABALHOS DERIVADOS DA TESE
136
TRABALHOS DERIVADOS DA TESE
137
TRABALHOS DERIVADOS DA TESE
138
TRABALHOS DERIVADOS DA TESE
139
TRABALHOS DERIVADOS DA TESE
140
TRABALHOS DERIVADOS DA TESE
TRABALHOS DERIVADOS DA TESE
141
TRABALHOS DERIVADOS DA TESE
TRABALHOS DERIVADOS DA TESE
142
TRABALHOS DERIVADOS DA TESE
TRABALHOS DERIVADOS DA TESE
143
TRABALHOS DERIVADOS DA TESE
TRABALHOS DERIVADOS DA TESE
144
TRABALHOS DERIVADOS DA TESE
TRABALHOS DERIVADOS DA TESE
145
Download